Abstract
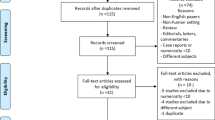
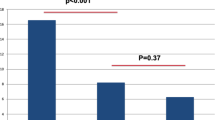
Penile detumescence is crucial for erectile physiology and may play a role in erectile dysfunction and priapism. However, few studies focus on the process of penile detumescence. This pilot study explores the feasibility of measuring the perceived duration of post-ejaculatory penile detumescence in real-life conditions in a convenience sample. Voluntary participants could access a survey between November 2020 and February 2021, with measurement instructions shared by the researchers across several online social networks. Participants measured penile detumescence, starting a stopwatch at ejaculation and recording two time points: onset of flaccidity and complete flaccidity. The survey collected basic demographics for description purposes. At survey closure, full responses of 83 (mean age 26.9 ± 8.9 years) participants were analyzed. The mean duration to onset of flaccidity was 57.9 ± 35.5 s, and to complete flaccidity was 180.7 ± 83.5 s, both following an approximately normal distribution. These durations were significantly correlated with each other (r = 0.47, p < 0.001), but not with any other variables. The results suggest that quantifying penile detumescence in real-life conditions is feasible. Future studies with a more robust design should verify these measurements and explore factors influencing detumescence duration in both real-life conditions and research settings.
This is a preview of subscription content, access via your institution
Access options

Similar content being viewed by others
Data availability
Data is available upon reasonable request by contacting the corresponding author.
References
Andersson KE. Mechanisms of penile erection and basis for pharmacological treatment of erectile dysfunction. Pharmacol Rev. 2011;63:811–59.
Altman AL, Seftel AD, Brown SL, Hampel N. Cocaine associated priapism. J Urol. 1999;161:1817–8.
Broderick GA, Gordon D, Hypolite J, Levin RM. Anoxia and corporal smooth muscle dysfunction: a model for ischemic priapism. J Urol. 1994;151:259–62.
De Tejada IS, Kim NN, Daley JT, Hypolite J, Broderick GA, Garcia-Diaz F, et al. Acidosis impairs rabbit trabecular smooth muscle contractility. J Urol. 1997;157:722–6.
Christ GJ, Stone B, Melman A. Age-dependent alterations in the efficacy of phenylephrine-induced contractions in vascular smooth muscle isolated from the corpus cavernosum of impotent men. Can J Physiol Pharmacol. 1991;69:909–13.
Christ GJ, Maayani S, Valcic M, Melman A. Pharmacological studies of human erectile tissue: characteristics of spontaneous contractions and alterations in α-adrenoceptor responsiveness with age and disease in isolated tissues. Br J Pharmacol. 1990;101:375–81.
Taub HC, Lerner SE, Melman A, Christ GJ. Relationship between contraction and relaxation in human and rabbit corpus cavernosum. Urology. 1993;42:698–704.
Francavilla S, Properzi G, Bellini C, Marino G, Ferri C, Santucci A. Endothelin-1 in diabetic and nondiabetic men with erectile dysfunction. J Urol. 1997;158:1770–4.
Jannini EA, Lenzi A, Isidori A, Fabbri A. Subclinical erectile dysfunction: proposal for a novel taxonomic category in sexual medicine. J Sex Med. 2006;3:787–94.
Claes H, Opsomer RJ, Andrianne R, Vanbelle S, Albert A, Vanderdonck F. Characteristics and expectations of patients with erectile dysfunction: results of the SCORED study. Int J Impot Res. 2008;20:418–24.
Claes HIM, Goldstein I, Althof SE, Berner MM, Cappelleri JC, Bushmakin AG, et al. Understanding the effects of sildenafil treatment on erection maintenance and erection hardness. J Sex Med. 2010;7:2184–91.
Yafi FA, Jenkins L, Albersen M, Corona G, Isidori AM, Goldfarb S, et al. Erectile dysfunction. Nat Rev Dis Primers. 2016;2:16003.
Ekmekçioǧlu O, Inci M, Demirci D, Tatlişen A. Effects of sildenafil citrate on ejaculation latency, detumescence time, and refractory period: placebo-controlled, double-blind, crossover laboratory setting study. Urology. 2005;65:347–52.
Ückert S, Fuhlenriede MH, Becker AJ, Stief CG, Scheller F, Knapp WH, et al. Is serotonin significant for the control of penile flaccidity and detumescence in the human male? Urol Res. 2003;31:55–60.
Becker AJ, Ückert S, Stief CG, Scheller F, Knapp WH, Hartmann U, et al. Cavernous and systemic plasma levels of norepinephrine and epinephrine during different penile conditions in healthy men and patients with erectile dysfunction. Urology. 2002;59:281–6.
Ückert S, Becker AJ, Ness BO, Stief CG, Scheller F, Knapp WH, et al. Oxytocin plasma levels in the systemic and cavernous blood of healthy males during different penile conditions. World J Urol. 2003;20:323–6.
Becker AJ, Ückert S, Stief CG, Truss MC, Hartmann U, Jonas U. Systemic and cavernosal plasma levels of endothelin (1–21) during different penile conditions in healthy males and patients with erectile dysfunction. World J Urol. 2001;19:371–6.
Broderick GA, Kadioglu A, Bivalacqua TJ, Ghanem H, Nehra A, Shamloul R. Priapism: pathogenesis, epidemiology, and management. J Sex Med. 2010;7:476–500.
Suijker CA, van Mazijk C, Keijzer FA, Meijer B. Phenomenological and existential contributions to the study of erectile dysfunction. Med Health Care Philos. 2021;24:597–608.
Bancroft J, Janssen E. The dual control model of male sexual response: a theoretical approach to centrally mediated erectile dysfunction. Neurosci Biobehav Rev. 2000;24:571–9.
Barlow DH. Causes of sexual dysfunction: the role of anxiety and cognitive interference. J Consult Clin Psychol. 1986;54:140–8.
Hedon F. Anxiety and erectile dysfunction: a global approach to ED enhances results and quality of life. Int J Impot Res. 2003;15:16–9.
Janssen E, McBride KR, Yarber W, Hill BJ, Butler SM. Factors that influence sexual arousal in men: a focus group study. Arch Sex Behav. 2008;37:252–65.
Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–7.
Waldinger MD, Hengeveld MW, Zwinderman AH, Olivier B. Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline. J Clin Psychopharmacol. 1998;18:274–81.
Waldinger D, Hengeveld W, Zwinderman AH. Paroxetine treatment of premature ejaculation. Am J Psychiatry. 1994;151:1377–99.
Althof SE, Levine SB, Corty EW, Risen CB, Stern EB, Kurit DM. A double-blind crossover trial of clomipramine for rapid ejaculation in 15 couples. J Clin Psychiatry. 1995;56:402–7.
Cooper AJ, Magnus RV. A clinical trial of the beta blocker propranolol in premature ejaculation. J Psychosom Res. 1984;28:331–6.
Tanner BA. Two case reports on the modification of the ejaculatory response with the squeeze technique. Psychotherapy. 1973;10:297–300.
Serefoglu EC, McMahon CG, Waldinger MD, Althof SE, Shindel A, Adaikan G, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second International Society for Sexual Medicine Ad Hoc committee for the definition of premature ejaculation. J Sex Med. 2014;11:1423–41.
Herbenick D, Reece M, Schick V, Sanders SA, Dodge B, Fortenberry JD. An event-level analysis of the sexual characteristics and composition among adults ages 18 to 59: Results from a national probability sample in the United States. J Sex Med. 2010;7:346–61.
Schick V, Herbenick D, Reece M, Sanders SA, Dodge B, Middlestadt SE, et al. Sexual behaviors, condom use, and sexual health of americans over 50: implications for sexual health promotion for older adults. J Sex Med. 2010;7:315–29.
Herbenick D, Reece M, Hensel D, Sanders S, Jozkowski K, Fortenberry JD. Association of lubricant use with women’s sexual pleasure, sexual satisfaction, and genital symptoms: a prospective daily diary study. J Sex Med. 2011;8:202–12.
Herbenick D, Fu TC, Dodge B, Fortenberry JD. The alcohol contexts of consent, wanted sex, sexual pleasure, and sexual assault: results from a probability survey of undergraduate students. J Am Coll Health. 2019;67:144–52.
Mulhall JP, Goldstein I, Bushmakin AG, Cappelleri JC, Hvidsten K. Validation of the erection hardness score. J Sex Med. 2007;4:1626–34.
Bosch RJLH, Benard F, Aboseif SR, Stief CG, Lue TF, Tanagho EA. Penile detumescence: characterization of three phases. J Urol. 1991;146:867–71.
Georgiadis JR, Farrell MJ, Boessen R, Denton DA, Gavrilescu M, Kortekaas R, et al. Dynamic subcortical blood flow during male sexual activity with ecological validity: a perfusion fMRI study. Neuroimage. 2010;50:208–16.
Hoaglin DC, Iglewicz B. Fine-tuning some resistant rules for outlier labeling. J Am Stat Assoc. 1987;82:1147–9.
Nair P, Kashyap I. Hybrid pre-processing technique for handling imbalanced data and detecting outliers for KNN classifier. In: Sharma, S, Batra N, eds. Proceedings of the 2019 international conference on machine learning, big data, cloud and parallel computing (COMITCon). Faridabad, India. Piscataway (NJ): IEEE; 2019. p. 460–4.
Sansone A, Aversa A, Corona G, Fisher AD, Isidori AM, La Vignera S, et al. Management of premature ejaculation: a clinical guideline from the Italian Society of Andrology and Sexual Medicine (SIAMS). J Endocrinol Invest. 2021;44:1103–18.
Rowland DL, Oosterhouse LB, Kneusel JA, Hevesi K. Comorbidities among sexual problems in men: results from an internet convenience sample. Sex Med. 2021;9:100416.
Burri A, Hilpert P. Postcoital symptoms in a convenience sample of men and women. J Sex Med. 2020;17:556–9.
Prah P, Hickson F, Bonell C, Mcdaid LM, Johnson AM, Wayal S, et al. Men who have sex with men in Great Britain: comparing methods and estimates from probability and convenience sample surveys. Sex Transm Infect. 2016;92:455–63.
Li W, Li G, Xin C, Wang Y, Yang S. Challenges in the practice of sexual medicine in the time of COVID-19 in China. J Sex Med. 2020;17:1212–5.
Nelson KM, Gordon AR, John SA, Stout CD, Macapagal K. “Physical sex is over for now”: impact of COVID-19 on the well-being and sexual health of adolescent sexual minority males in the U.S. J Adolesc Heal. 2020;67:756–62.
Nobre PJ, Wiegel M, Bach AK, Weisberg RB, Brown TA, Wincze JP, et al. Determinants of sexual arousal and the accuracy of its self-estimation in sexually functional males. J Sex Res. 2004;41:363–71.
McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The arizona sexual experience scale (ASEX): reliability and validity. J Sex Marital Ther. 2000;26:25–38.
Rosen RC, Catania J, Pollack L, Althof S, O’Leary M, Seftel AD. Male sexual health questionnaire (MSHQ): scale development and psychometric validation. Urology. 2004;64:777–82.
Johnson MJ, McNeillis V, Chiriaco G, Ralph DJ. Rare disorders of painful erection: a cohort study of the investigation and management of stuttering priapism and sleep-related painful erection. J Sex Med. 2021;18:376–84.
Author information
Authors and Affiliations
Contributions
CAS (Conceptualization; Methodology; Formal Analysis; Writing– Original Draft; Writing– Review & Editing). JRG (Conceptualization; Methodology; Writing– Review & Editing; Supervision). BM (Conceptualization; Methodology; Writing– Review & Editing; Supervision).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Notion of this study was given to the Medical Ethical Committee of the University Medical Center Groningen (study no. 202000606), which approved all study procedures.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suijker, C.A., Georgiadis, J.R. & Meijer, B. Measuring the perceived duration of post-ejaculatory penile detumescence: a pilot study in a real-life setting. Int J Impot Res (2025). https://doi.org/10.1038/s41443-025-01122-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-025-01122-6
This article is cited by
-
Comment on: Measuring the perceived duration of post-ejaculatory penile detumescence: a pilot study in a real-life setting
International Journal of Impotence Research (2025)