Abstract
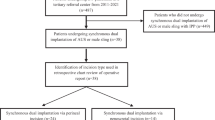
The artificial urinary sphincter is the standard surgical treatment for persistent stress urinary incontinence in male patients when conservative methods fail, with the perineal approach being the most commonly used. However, the penoscrotal approach, which requires only a single incision, offers advantages such as shorter operation times and ease of execution, though concerns about lower dry rates and higher complication risks remain. This retrospective cohort study analyzed outcomes of 156 patients who underwent artificial urinary sphincter implantation via the penoscrotal approach between 2014 and 2024, excluding revision and double prosthesis cases. The mean patient age was 72.5 ± 6.8 years, a median cuff size of 4 cm (3.5–6), a mean operation time of 28.3 ± 8.7 min and a median follow-up of 27.6 (2.6–109.7) months. The most common immediate postoperative complication was urinary retention (5.8%). At six months, 65.4% of patients were completely dry, and 82.7% were socially continent. Revision was required in 32.1% of cases, aligning with literature-reported rates. This study suggests that the penoscrotal approach is a viable alternative to the perineal method, offering potential benefits in operative efficiency while maintaining comparable outcomes to the classic perineal approach.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to privacy reasons but are available from the corresponding author on reasonable request.
References
Cornu (Chair) JN, Gacci M, Hashim H, Herrmann TRW, Malde S, Netsch C, et al. EAU guidelines on Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS). 2024. https://uroweb.org/guidelines/management-of-non-neurogenic-male-luts.
Sacco E, Prayer-Galetti T, Pinto F, Fracalanza S, Betto G, Pagano F, et al. Urinary incontinence after radical prostatectomy: Incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up. BJU Int. 2006;97:1234–41.
Scott FB, Bradley WE, Timm GW. Treatment of urinary incontinence by implantable prosthetic sphincter. Urology. 1973;1:252–9.
Sandhu JS, Breyer B, Comiter C, Eastham JA, Gomez C, Kirages DJ, et al. Incontinence after Prostate Treatment: AUA/SUFU Guideline. J. Urol. 2019;202:369–78.
Data on file with Boston Scientific. 2025. https://www.bostonscientific.com/en-US/products/artificial-urinary-sphincter/ams-800-artificial-urinary-sphincter.html.
Henry GD, Graham SM, Cornell RJ, Cleves MA, Simmons CJ, Vakalopoulos I, et al. A multicenter study on the perineal versus penoscrotal approach for implantation of an artificial urinary sphincter: cuff size and control of male stress urinary incontinence. J. Urol. 2009;182:2404–9.
Wilson SK, Delk JR, Henry GD, Siegel AL. New surgical technique for sphincter urinary control system using upper transverse scrotal incision. J. Urol. 2003;169:261–4.
Altaweel W, Almesned R, Seyam R. A comparison of the perineal and penoscrotal approaches in artificial urinary sphincter implantation for the control of male stress urinary incontinence. Ann. Saudi Med. 2023;43:57–61.
Jamaer C, De Bruyn H, Van Renterghem A, Baten E, Van Renterghem K. Penoscrotal incision for the primary implantation of an artificial urinary sphincter. Curr. Urol. 2020;14:74–8.
Martens F, Heesakkers J, Van der Aa F, Thiruchelvam N, Witjes W, Caris C, et al. SATURN: a European, prospective, multicentre registry for male stress urinary incontinence surgery. Eur. Urol. Open. Sci. 2023;57:91–7.
Staniorski CJ, Singal A, Nettey O, Yura E, Keeter MK, Kielb S, et al. Revisiting the penoscrotal approach to artificial urinary sphincter surgery: how does it compare to a perineal incision for initial implantation? World J. Urol. 2021;39:871–6.
Khouri RK, Ortiz NM, Dropkin BM, Joice GA, Baumgarten AS, Morey AF, et al. Artificial urinary sphincter complications: risk factors, workup, and clinical approach. Curr. Urol. Rep. 2021;22:30.
Anusionwu I, Miles-Thomas J, Hernandez DJ, Wright EJ. Anatomical and manometric comparison of perineal and transscrotal approaches to artificial urinary sphincter placement. J. Urol. 2012;188:1834–6.
Van der Aa F, Drake MJ, Kasyan GR, Petrolekas A, Cornu JN, Young Academic Urologists Functional Urology Group. The artificial urinary sphincter after a quarter of a century: a critical systematic review of its use in male non-neurogenic incontinence. Eur. Urol. 2013;63:681–9.
Linder BJ, Rivera ME, Ziegelmann MJ, Elliott DS. Long-term outcomes following artificial urinary sphincter placement: an analysis of 1082 cases at mayo clinic. Urology. 2015;86:602–7.
Desai TJ, Rozanski AT. Artificial urinary sphincter erosion and infection: a contemporary review of perioperative considerations and management. Transl. Androl. Urol. 2024;13:857–67.
Wang R, McGuire EJ, He C, Faerber GJ, Latini JM. Long-term outcomes after primary failures of artificial urinary sphincter implantation. Urology. 2012;79:922–8.
Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the university of michigan. J. Urol. 2008;179:1912–6.
Gross M, Phillips EA, Carrasquillo R, Thornton A, Greenfield J, Levine LA, et al. Multicenter investigation of the micro-organisms involved in penile prosthesis infection: an analysis of the efficacy of the AUA and EAU guidelines for penile prosthesis prophylaxis. J. Sex. Med. 2017;14:455–63.
Wilson SK, Chung E, Langford B, Schlesinger R, Koca O, Simsek A, et al. First safety outcomes for rigicon conticlassic® artificial urinary sphincter. Int. J. Impot. Res. 2024;36:829–32.
Fuller TW, Ballon-Landa E, Gallo K, Smith TG, Ajay D, Westney OL, et al. Outcomes and risk factors of revision and replacement artificial urinary sphincter implantation in radiated and nonradiated cases. J. Urol. 2020;204:110–4.
Malshy K, Marthi S, Ortiz R, Nicaise E, Golijanin B, Miller K, et al. Timing considerations for artificial urinary sphincter implantation postpelvic radiotherapy. Urology. 2024;193:214–9.
Sotelo TM, Westney OL. Outcomes related to placing an artificial urinary sphincter using a single-incision, transverse-scrotal technique in high-risk patients. BJU Int. 2008;101:1124–7.
Kendirci M, Gupta S, Shaw K, Morey A, Jones LR, Hakim L, et al. Synchronous Prosthetic Implantation Through a Transscrotal Incision: An Outcome Analysis. J. Urol. 2006;175:2218–22.
Sandhu JS, Maschino AC, Vickers AJ. The surgical learning curve for artificial urinary sphincter procedures compared to typical surgeon experience. Eur. Urol. 2011;60:1285–90.
Author information
Authors and Affiliations
Contributions
Lien Verbeke: Corresponding author, first author. Helene De Bruyn: Helped write the article. Caroline Jamaer: Provided feedback on the article. Alexander Van Renterghem: Provided feedback on the article. Evert Baten: Reviewed the article, Koenraad Van Renterghem: Senior author.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. Ethical approval: SATURN trial (NCT02757274). Informed consent for study participation was obtained from all participants. Written consent for publication of images was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verbeke, L., De Bruyn, H., Jamaer, C. et al. The penoscrotal approach is a viable alternative to the perineal approach for artificial urinary sphincter implantation: a retrospective cohort study. Int J Impot Res (2025). https://doi.org/10.1038/s41443-025-01178-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-025-01178-4