Abstract
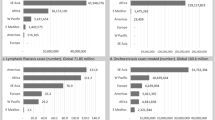
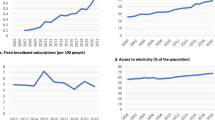
Neglected tropical diseases (NTDs) impose severe health, social and economic burdens on millions in impoverished regions. These diseases, once overlooked, have gained global attention following strategic advocacy and planning by the World Health Organization and its partners, and are now prioritized within the Sustainable Development Goals framework. In this Review, we examine current interventions including preventive chemotherapy, innovative and intensified disease management, vector control, One Health, and improvements in water, sanitation and hygiene; and we highlight the role of human behaviour and community engagement and involvement in driving intervention success, sustainability and ownership within communities. Regional disparities, particularly in sub-Saharan Africa and South Asia, call for tailored approaches that tackle logistical barriers, funding constraints, donor dependency, stigma and drug resistance. To control and eradicate NTDs by 2030, we require sustained political commitment, innovative financing and the greater integration of NTD strategies within broader health systems.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
WHO. Global Report on Neglected Tropical Diseases 2024 (WHO, 2024).
Hotez, P. & Kamath, A. Neglected tropical diseases in sub-Saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Negl. Trop. Dis. 3, e412 (2009).
Molyneux, D. H., Savioli, L. & Engels, D. Neglected tropical diseases: progress towards addressing the chronic pandemic. Lancet 389, 312–325 (2017).
Fenwick, A. The global burden of neglected tropical diseases. Public Health 126, 233–236 (2012).
CDC. Neglected tropical diseases fact sheet. cdc.gov https://www.cdc.gov/neglected-tropical-diseases/index.html (CDC, 2024).
WHO. Strategic and Technical Meeting on Intensified Control of Neglected Tropical Diseases: A Renewed Effort to Combat Entrenched Communicable Diseases of the Poor: Report of an International Workshop, Berlin, 18–20 April 2005 WHO/CDS/NTD/2006.1 (WHO, 2006).
WHO. Intensified Control of Neglected Diseases: Report of an International Workshop, Berlin, 10–12 December 2003 WHO/CDS/CPE/CEE/2004.45 (WHO, 2004).
WHO. Accelerating Work to Overcome the Global Impact of Neglected Tropical Diseases – A Roadmap for Implementation (WHO, 2012).
UN General Assembly. Resolution adopted by the General Assembly on 10 October 2019. 74/2. political declaration of the high-level meeting on universal health coverage. un.org https://docs.un.org/en/A/RES/74/2 (2019).
WHO. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030 (WHO, 2020).
Hotez, P. et al. The Global Burden of Disease Study 2010: interpretation and implications for the neglected tropical diseases. PLoS Negl. Trop. Dis. 8, e2865 (2014).
Lv, J., Zhang, Y., Li, X., Yang, C. & Wang, X. Global, regional, national epidemiology and trends of neglected tropical diseases in youths and young adults aged 15–39 years from 1990 to 2019: findings from the Global Burden of Disease Study 2019. BMC Public Health 24, 2088 (2024).
Martins-Melo, F. R. et al. The burden of neglected tropical diseases in Brazil, 1990–2016: a subnational analysis from the Global Burden of Disease Study 2016. PLoS Negl. Trop. Dis. 12, e0006559 (2018).
Buscaglia, C. A., Kissinger, J. C. & Agüero, F. Neglected tropical diseases in the post-genomic era. Trends Genet. 31, 539–555 (2015).
WHO. Global Report on Neglected Tropical Diseases 2023 (WHO, 2023).
Moeti, M. Africa: the elimination of neglected tropical diseases is finally within reach. afro.who.int https://www.afro.who.int/media-centre/statements-commentaries/africa-elimination-neglected-tropical-diseases-finally-within (2018).
WHO. Promising progress on neglected tropical diseases in Africa. afro.who.int https://www.afro.who.int/news/promising-progress-neglected-tropical-diseases-africa (2022).
Lin, Y., Fang, K., Zheng, Y., Wang, H. L. & Wu, J. Global burden and trends of neglected tropical diseases from 1990 to 2019. J. Travel Med. 29, taac031 (2022).
Tilli, M. et al. Neglected tropical diseases in non-endemic countries in the era of COVID-19 pandemic: the great forgotten. J. Travel Med. 28, taaa179 (2021).
GBD Collaborative Network. Global Burden of Disease Study 2021 (GBD 2021) Results. healthdata.org https://vizhub.healthdata.org/gbd-results/ (2022).
WHO. Echinococcosis. who.int https://www.who.int/news-room/fact-sheets/detail/echinococcosis (2021).
WHO. Dracunculiasis (guinea-worm disease). who.int https://www.who.int/news-room/fact-sheets/detail/dracunculiasis-(guinea-worm-disease) (2025).
van de Sande, W. et al. Closing the mycetoma knowledge gap. Med. Mycol. 56, S153–S164 (2018).
Emery, D. & Denning, D. W. The global distribution of actinomycetoma and eumycetoma. PLoS Negl. Trop. Dis. 14, e0008397 (2020).
WHO. Mycetoma. who.int https://www.who.int/en/news-room/fact-sheets/detail/mycetoma (2022).
WHO. Podoconiosis (non-filarial lymphoedema). who.int https://www.who.int/news-room/fact-sheets/detail/podoconiosis-(non-filarial-lymphoedema) (2023).
Deribe, K. et al. Podoconiosis: key priorities for research and implementation. Trans. R. Soc. Trop. Med. Hyg. 114, 889–895 (2020).
Deribe, K. et al. Mapping the global distribution of podoconiosis: applying an evidence consensus approach. PLoS Negl. Trop. Dis. 13, e0007925 (2019).
Mitra, A. K. & Mawson, A. R. Neglected tropical diseases: epidemiology and global burden. Trop. Med. Infect. Dis. 2, 36 (2017).
Maguire, B. J. et al. Protocol for a systematic review of the evidence-based knowledge on the distribution, associated risk factors, the prevention and treatment modalities for noma [version 1; peer review: 2 approved with reservations]. Wellcome Open Res. 8, 125 (2023).
WHO. Schistosomiasis. who.int https://www.who.int/news-room/fact-sheets/detail/schistosomiasis (2023).
WHO. Lymphatic filariasis. who.int https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis (2023).
WHO. Mental Health of People with Neglected Tropical Diseases: Towards a Person-Centred Approach (WHO, 2020).
Bailey, F. et al. A new perspective on cutaneous leishmaniasis—implications for global prevalence and burden of disease estimates. PLoS Negl. Trop. Dis. 11, e0005739 (2017).
Govindasamy, K., Jacob, I., Solomon, R. M. & Darlong, J. Burden of depression and anxiety among leprosy affected and associated factors—a cross sectional study from India. PLoS Negl. Trop. Dis. 15, e0009030 (2021).
Somar, P., Waltz, M. & van Brakel, W. The impact of leprosy on the mental wellbeing of leprosy-affected persons and their family members—a systematic review. Glob. Ment. Health 7, e15 (2020).
Molyneux, D. H. Mental health and neglected tropical diseases—the neglected dimension of burden: identifying the challenges and understanding the burden. Int. Health 15, iii3–iii6 (2023).
Weiss, M. G. & Ramakrishna, J. Stigma interventions and research for international health. Lancet 367, 536–538 (2006).
Conteh, L., Engels, T. & Molyneux, D. H. Socioeconomic aspects of neglected tropical diseases. Lancet 375, 239–247 (2010).
Lutumba, P., Makieya, E., Shaw, A., Meheus, F. & Boelaert, M. Human African trypanosomiasis in a rural community, Democratic Republic of Congo. Emerg. Infect. Dis. 13, 248–254 (2007).
Aronson, S. M. The global burden of trachoma. Med. Health R. I. 87, 91 (2004).
Gyapong, M. et al. in Neglected Tropical Diseases—Sub-Saharan Africa (eds Gyapong, J. O. & Boatin, B. A.) 479–503 (Springer, 2024).
Goldman, A. S. et al. National mass drug administration costs for lymphatic filariasis elimination. PLoS Negl. Trop. Dis. 1, e67 (2007).
Godwin-Akpan, T. G. et al. Assessing the cost-effectiveness of integrated case management of neglected tropical diseases in Liberia. BMC Health Serv. Res. 23, 705 (2023).
The END Fund. Ending the neglect: cost–benefit analysis of eliminating neglected tropical diseases in Nigeria by 2030. end.org https://end.org/ending-the-neglect-cost-benefit-analysis-of-eliminating-neglected-tropical-diseases-in-nigeria-by-2030/ (END Fund, 2023).
Molyneux, D. H. ‘Neglected’ diseases but unrecognised successes—challenges and opportunities for infectious disease control. Lancet 364, 380–383 (2004).
Seddoh, A., Onyeze, A., Gyapong, J. O., Holt, J. & Bundy, D. Towards an investment case for neglected tropical diseases including new analysis of the cost of intervening against preventable NTDs in sub-Saharan Africa. Lancet 9908, 1898–1955 (2013).
Molyneux, D. H. Combating the ‘other diseases’ of MDG 6: changing the paradigm to achieve equity and poverty reduction? Trans. R. Soc. Trop. Med. Hyg. 102, 509–519 (2008).
Fitzpatrick, C., Nwankwo, U., Lenk, E., de Vlas, S. J. & Bundy, D. A. P. in Disease Control Priorities: Major Infectious Diseases, 3rd edn, Vol. 6 (eds Holmes, K. K. et al.) Ch. 17, 411–431 (World Bank, 2017).
Fitzpatrick, C. & Engels, D. Leaving no one behind: a neglected tropical disease indicator and tracers for the Sustainable Development Goals. Int. Health 8, i15–i18 (2015).
Hotez, P., Ottesen, E., Fenwick, A. & Molyneux, D. in Hot Topics in Infection and Immunity in Children III (eds Pollard, A. J. & Finn, A.) 23–33 (Springer US, 2006).
Addisu, A. et al. Neglected tropical diseases and the Sustainable Development Goals: an urgent call for action from the front line. BMJ Glob. Health 4, e001334 (2019).
Amazigo, U. V. et al. Community-directed distributors—the ‘foot soldiers’ in the fight to control and eliminate neglected tropical diseases. PLoS Negl. Trop. Dis. 15, e0009088 (2021).
Koffi, A. P. et al. Integrated approach in the control and management of skin neglected tropical diseases in three health districts of Côte d’Ivoire. BMC Public Health 20, 517 (2020).
Gyapong, J. O. et al. Integration of control of neglected tropical diseases into health-care systems: challenges and opportunities. Lancet 375, 160–165 (2010).
Molyneux, D. H., Hotez, P. & Fenwick, A. ‘Rapid-impact interventions’: how a policy of integrated control for Africa’s neglected tropical diseases could benefit the poor. PLoS Med. 2, e336 (2005).
Uniting to Combat NTDs. 100% committed to ending NTDs. Uniting to Combat NTDs https://unitingtocombatntds.org/en/ (2024).
Gyapong, J. O. & Boatin, B. A. (eds) Neglected Tropical Diseases—Sub-Saharan Africa (Springer International, 2024).
Engels, D. & Zhou, X. N. Neglected tropical diseases: an effective global response to local poverty-related disease priorities. Infect. Dis. Poverty 9, 10 (2020).
Anesvad Foundation. Anesvad Foundation Strategic Plan 2023–2026. Anesvad Foundation https://www.anesvad.org/en/our-purpose (2024).
Hotez, P., Velasquez, R. M. & Wolf, J. E. Neglected tropical skin diseases: their global elimination through integrated mass drug administration? JAMA Dermatol. 150, 481–482 (2014).
WHO. Control of neglected tropical diseases: vector control. who.int https://www.who.int/teams/control-of-neglected-tropical-diseases/interventions/strategies/vector-control (2024).
Bush, S. & Hopkins, A. D. Public–private partnerships in neglected tropical disease control: the role of nongovernmental organisations. Acta Trop. 120, S169–S172 (2011).
Montresor, A. et al. Preventive chemotherapy and the fight against neglected tropical diseases. Expert Rev. Anti Infect. Ther. 10, 237–242 (2012).
Gyapong, M., Gyapong, J. O. & Owusu-Banahene, G. Community-directed treatment: the way forward to eliminating lymphatic filariasis as a public-health problem in Ghana. Ann. Trop. Med. Parasitol. 95, 77–86 (2001).
WHO. Era of Transformation: Neglected Tropical Diseases in the African Region (WHO Regional Office for Africa, 2023).
WHO. Brazil eliminates lymphatic filariasis as a public health problem. who.int https://www.who.int/news/item/01-10-2024-brazil-eliminates-lymphatic-filariasis-as-a-public-health-problem (2024).
WHO. Onchocerciasis. who.int https://www.who.int/news-room/fact-sheets/detail/onchocerciasis (2022).
Turner, H. C. et al. Are current preventive chemotherapy strategies for controlling and eliminating neglected tropical diseases cost-effective? BMJ Glob. Health 6, e005456 (2021).
Ngatse, J. A. et al. Historical overview and geographical distribution of neglected tropical diseases amenable to preventive chemotherapy in the Republic of the Congo: a systematic review. PLoS Negl. Trop. Dis. 16, e0010560 (2022).
WHO. WHO validates the elimination of trachoma as a public health problem in Pakistan. who.int https://www.who.int/news/item/01-10-2024-who-validates-the-elimination-of-trachoma-as-a-public-health-problem-in-pakistan (2024).
WHO. Countries having eliminated at least one neglected tropical disease. who.int https://www.who.int/images/default-source/maps/elimination_ntds.png?sfvrsn=bb12c410_10 (2025).
Webster, J. P., Molyneux, D. H., Hotez, P. & Fenwick, A. The contribution of mass drug administration to global health: past, present and future. Phil. Trans. R. Soc. B 369, 20130434 (2014).
Asfaw, M. A., Hailu, C. & Beyene, T. J. A qualitative study exploring barriers, facilitators and solutions to equitable coverage of preventive chemotherapy towards the control and elimination of neglected tropical diseases in South Omo zone, nomadic setting of Southern Ethiopia: stakeholders’ perspectives and experiences. Preprint at Research Square https://doi.org/10.21203/rs.3.rs-152413/v1 (2021).
Otoo, D. D., Agbenu, I. A., Nyamekye, M. A. & Appiah-Agyekum, N. N. Challenges of implementation of the preventive chemotherapy neglected tropical diseases programme in Ghana. PLoS Negl. Trop. Dis. 17, e0011116 (2023).
Manyeh, A. K., Ibisomi, L., Ramaswamy, R., Baiden, F. & Chirwa, T. Exploring factors affecting quality implementation of lymphatic filariasis mass drug administration in Bole and Central Gonja Districts in Northern Ghana. PLoS Negl. Trop. Dis. 14, e0007009 (2020).
Bockarie, M. J., Kelly-Hope, L. A., Rebollo, M. & Molyneux, D. H. Preventive chemotherapy as a strategy for elimination of neglected tropical parasitic diseases: endgame challenges. Phil. Trans. R. Soc. B 368, 20120144 (2013).
Franco, J. R. et al. Monitoring the elimination of human African trypanosomiasis at continental and country level: update to 2018. PLoS Negl. Trop. Dis. 14, e0008261 (2020).
Ward, P. et al. Affordable artificial intelligence-based digital pathology for neglected tropical diseases: a proof-of-concept for the detection of soil-transmitted helminths and Schistosoma mansoni eggs in Kato–Katz stool thick smears. PLoS Negl. Trop. Dis. 16, e0010500 (2022).
WHO. Benin, Uganda and Rwanda eliminate human African trypanosomiasis as a public health problem: departmental update. who.int https://www.who.int/news/item/24-05-2022-benin–uganda-and-rwanda-eliminate-human-african-trypanosomiasis-as-a-public-health-problem (2022).
Vouking, M. Z., Tamo, V. C. & Tadenfok, C. N. Clinical efficacy of rifampicin and streptomycin in combination against Mycobacterium ulcerans infection: a systematic review. Pan Afr. Med. J. 15, 155 (2013).
Etuaful, S. et al. Efficacy of the combination rifampin–streptomycin in preventing growth of Mycobacterium ulcerans in early lesions of Buruli ulcer in humans. Antimicrob. Agents Chemother. 49, 3182–3186 (2005).
Amoussouhoui, A. S. et al. Steps toward creating a therapeutic community for inpatients suffering from chronic ulcers: lessons from Allada Buruli Ulcer Treatment Hospital in Benin. PLoS Negl. Trop. Dis. 10, e0004602 (2016).
Asiedu, K. & Etuaful, S. Socioeconomic implications of Buruli ulcer in Ghana: a three-year review. Am. J. Trop. Med. Hyg. 59, 1015–1022 (1998).
Abass, K. M. et al. Buruli ulcer control in a highly endemic district in Ghana: role of community-based surveillance volunteers. Am. Soc. Trop. Med. Hyg. 92, 115–117 (2015).
Debrah, L. B. et al. Morbidity management and surveillance of lymphatic filariasis disease and acute dermatolymphangioadenitis attacks using a mobile phone-based tool by community health volunteers in Ghana. PLoS Negl. Trop. Dis. 14, e0008839 (2020).
Barogui, Y. T. et al. Contribution of the community health volunteers in the control of Buruli ulcer in Bénin. PLoS Negl. Trop. Dis. 8, e3200 (2014).
WHO. India’s massive leprosy case detection campaign reaches 320 million people. who.int https://www.who.int/news/item/18-10-2016-india-s-massive-leprosy-case-detection-campaign-reaches-320-million-people (2016).
Addiss, D. G. & Brady, M. A. Morbidity management in the Global Programme to Eliminate Lymphatic Filariasis: a review of the scientific literature. Filaria J. 6, 2 (2007).
Bockarie, M. J., Taylor, M. J. & Gyapong, J. Current practices in the management of lymphatic filariasis. Expert Rev. Anti Infect. Ther. 7, 595–605 (2009).
Kumari, A. K., Krishnamoorthy, K., Harichandrakumar, K. & Das, L. Health related quality of life, an appropriate indicator to assess the impact of morbidity management and disability prevention activities towards elimination of lymphatic filariasis. Filaria J. 6, 8 (2007).
Malaria Consortium. Strengthening Primary Healthcare for Neglected Tropical Diseases in Ethiopia (Malaria Consortium, 2018).
Emeto, D. C., Salawu, A. T., Salawu, M. M. & Fawole, O. I. Recognition and reporting of neglected tropical diseases by primary health care workers in Ibadan, Nigeria. Pan Afr. Med J. 38, 224 (2021).
Ahlgren, M., Funk, T., Marimo, C., Ndiaye, C. & Alfvén, T. Management of noma: practice competence and knowledge among healthcare workers in a rural district of Zambia. Glob. Health Action 10, 1340253 (2017).
Brattström-Stolt, L., Funk, T., Sié, A., Ndiaye, C. & Alfvén, T. Noma—knowledge and practice competence among primary healthcare workers: a cross-sectional study in Burkina Faso. Int. Health 11, 290–296 (2019).
Srour, M. L., Marck, K. & Baratti-Mayer, D. Noma: overview of a neglected disease and human rights violation. Am. Soc. Trop. Med. Hyg. 96, 268–274 (2017).
Corley, A. G., Thornton, C. P. & Glass, N. E. The role of nurses and community health workers in confronting neglected tropical diseases in sub-Saharan Africa: a systematic review. PLoS Negl. Trop. Dis. 10, e0004914 (2016).
Chotun, N. et al. Sustaining success through strategies for post-elimination management of neglected tropical diseases in African Union Member States. Front. Trop. Dis. 5, 1421522 (2024).
The Lancet Digital Health. Technology for world elimination of neglected tropical diseases. Lancet Digit. Health 5, e51 (2023).
WHO. Advancing the management of skin-related neglected tropical diseases in Ghana: exploration of gender-related factors and mobile technology. who.int https://tdr.who.int/newsroom/news/item/14-12-2022-advancing-the-management-of-skin-related-neglected-tropical-diseases-in-Ghana-exploration-of-gender-related-factors-and-mobile-technology (2022).
Rubiano, L. et al. Adaptation and performance of a mobile application for early detection of cutaneous leishmaniasis. PLoS Negl. Trop. Dis. 15, e0008989 (2021).
WHO. Skin-related neglected tropical diseases: WHO launches new version of the WHO skin NTDs mobile application. who.int https://www.who.int/news/item/09-10-2023-skin-related-neglected-tropical-diseases–who-launches-new-version-of-the-who-skin-ntds-mobile-application (2023).
Simarro, P. P. et al. The atlas of human African trypanosomiasis: a contribution to global mapping of neglected tropical diseases. Int. J. Health Geogr. 9, 57 (2010).
Dil, Y., Strachan, D., Cairncross, S., Korkor, A. S. & Hill, Z. Motivations and challenges of community-based surveillance volunteers in the Northern Region of Ghana. J. Community Health 37, 1192–1198 (2012).
Owusu, L. et al. Role and capacity needs of community based surveillance volunteers in the integrated management of skin neglected tropical diseases (skin NTDs): a qualitative study from central Ghana. BMC Public Health 23, 1086 (2023).
Koschorke, M., Al-Haboubi, Y. H., Tseng, P.-C., Semrau, M. & Eaton, J. Mental health, stigma, and neglected tropical diseases: a review and systematic mapping of the evidence. Front. Trop. Dis. 3, 808955 (2022).
Eaton, J. et al. Integration of services for neglected tropical diseases and mental health in Nigeria: development of a practical model informed by international recommendations, contextual factors and service-user perspectives. Int. Health 15, iii47–iii58 (2023).
Freeman, M. C. et al. Integration of water, sanitation, and hygiene for the prevention and control of neglected tropical diseases: a rationale for inter-sectoral collaboration. PLoS Negl. Trop. Dis. 7, e2439 (2013).
Chinyama, J. et al. Menstrual hygiene management in rural schools of Zambia: a descriptive study of knowledge, experiences and challenges faced by schoolgirls. BMC Public Health 19, 16 (2019).
Joshi, A. & Amadi, C. Impact of water, sanitation, and hygiene interventions on improving health outcomes among school children. J. Environ. Public Health 2013, 1–10 (2013).
WHO. Water, Sanitation and Hygiene for Accelerating and Sustaining Progress on Neglected Tropical Diseases: A Global Strategy, 2015–2020 (WHO, 2016).
Salou Bachirou, Z. et al. WASH and NTDs: outcomes and lessons learned from the implementation of a formative research study in NTD skin co-endemic communities in Benin. Front. Med. 10, 1022314 (2023).
Hürlimann, E. et al. Effect of an integrated intervention package of preventive chemotherapy, community-led total sanitation and health education on the prevalence of helminth and intestinal protozoa infections in Côte d’Ivoire. Parasit. Vectors 11, 115 (2018).
Roba, A. A., Wondimu, A., Patel, D. & Zondervan, M. Effects of intervention with the SAFE strategy on trachoma across Ethiopia. J. Epidemiol. Community Health 65, 626–631 (2011).
WHO. Morocco defeats trachoma: departmental update. who.int https://www.who.int/news/item/15-11-2016-morocco-defeats-trachoma (2016).
Rwakimari, J. B., Hopkins, D. R. & Ruiz-Tiben, E. Uganda’s successful Guinea worm eradication program. Am. J. Trop. Med. Hyg. 75, 3–8 (2006).
Chowdhury, R. et al. Effect of insecticide-treated bed nets on visceral leishmaniasis incidence in Bangladesh: a retrospective cohort analysis. PLoS Negl. Trop. Dis. 13, e0007724 (2019).
Courtenay, O., Gillingwater, K., Gomes, P. A. F., Garcez, L. M. & Davies, C. R. Deltamethrin‐impregnated bednets reduce human landing rates of sandfly vector Lutzomyia longipalpis in Amazon households. Med. Vet. Entomol. 21, 168–176 (2007).
Nagpal, B. N. et al. Control of Aedes aegypti breeding: a novel intervention for prevention and control of dengue in an endemic zone of Delhi, India. PLoS ONE 11, e0166768 (2016).
Waite, R. C., Velleman, Y., Woods, G., Chitty, A. & Freeman, M. C. Integration of water, sanitation and hygiene for the control of neglected tropical diseases: a review of progress and the way forward. Int. Health 8, i22–i27 (2016).
Boakye, D., de Souza, D. & Bockarie, M. in Neglected Tropical Diseases—Sub-Saharan Africa (eds Gyapong, J. O. & Boatin, B. A.) 367–384 (Springer, 2016).
Johnston, E. A., Teague, J. & Graham, J. P. Challenges and opportunities associated with neglected tropical disease and water, sanitation and hygiene intersectoral integration programs. BMC Public Health 15, 547 (2015).
Bhatt, N. et al. What motivates open defecation? A qualitative study from a rural setting in Nepal. PLoS ONE 14, e0219246 (2019).
Koenker, H. M., Loll, D., Rweyemamu, D. & Ali, A. S. A good night’s sleep and the habit of net use: perceptions of risk and reasons for bed net use in Bukoba and Zanzibar. Malar. J. 12, 203 (2013).
Epelboin, Y. et al. Successes and failures of sixty years of vector control in French Guiana: what is the next step? Mem. Inst. Oswaldo Cruz 113, e170398 (2018).
WHO. Ending the Neglect to Attain the Sustainable Development Goals One Health: Approach for Action Against Neglected Tropical Diseases 2021–2030 (WHO, 2022).
Dhimal, M. et al. Risk factors for the presence of chikungunya and dengue vectors (Aedes aegypti and Aedes albopictus), their altitudinal distribution and climatic determinants of their abundance in central Nepal. PLoS Negl. Trop. Dis. 9, e0003545 (2015).
Esser, H. J. et al. Risk factors associated with sustained circulation of six zoonotic arboviruses: a systematic review for selection of surveillance sites in non-endemic areas. Parasit. Vectors 12, 265 (2019).
Parham, P. E. et al. Climate, environmental and socio-economic change: weighing up the balance in vector-borne disease transmission. Phil. Trans. R. Soc. B 370, 20130551 (2015).
Pedersen, U. B. et al. Modelling climate change impact on the spatial distribution of fresh water snails hosting trematodes in Zimbabwe. Parasit. Vectors 7, 536 (2014).
Slater, H. & Michael, E. Predicting the current and future potential distributions of lymphatic filariasis in Africa using maximum entropy ecological niche modelling. PLoS ONE 7, e32202 (2012).
Chalghaf, B. et al. Ecological niche modeling predicting the potential distribution of leishmania vectors in the Mediterranean basin: impact of climate change. Parasit. Vectors 11, 461 (2018).
Yang, G.-J. & Bergquist, R. Potential impact of climate change on schistosomiasis: a global assessment attempt. Trop. Med. Infect. Dis. 3, 117 (2018).
World Meteorological Organization. WMO Statement on the State of the Global Climate (World Meteorological Organization, 2019).
Zammarchi, L. et al. Schistosomiasis, strongyloidiasis and Chagas disease: the leading imported neglected tropical diseases in Italy. J. Travel Med. 27, taz100 (2020).
Ruscio, B. A., Brubaker, M., Glasser, J., Hueston, W. & Hennessy, T. W. One Health—a strategy for resilience in a changing arctic. Int. J. Circumpolar Health 74, 27913 (2015).
Richard Stauffer, J. & Madsen, H. A One Health approach to reducing schistosomiasis transmission in Lake Malawi. Prev. Med. Community Health 1, 100761 (2018).
Lushasi, K. et al. One Health in practice: using integrated bite case management to increase detection of rabid animals in Tanzania. Front. Public Health 8, 13 (2020).
Mackenzie, J. S. et al. eds. One Health: The Human–Animal–Environment Interfaces in Emerging Infectious Diseases Vol. 365 (Springer Berlin Heidelberg, 2013).
COR-NTD. Funding. COR-NTD https://www.cor-ntd.org/funding (2025).
RTI International. Controlling and eliminating NTDs around the world. rti.org https://www.rti.org/focus-area/neglected-tropical-diseases (2025).
CIFF. 2023 CIFF annual report. ciff.org https://year-in-review.ciff.org/ (2024).
Wellcome. Investments. wellcome.org https://wellcome.org/who-we-are/investments (2025).
Gates Foundation. Global donors pledge over US$777 million to defeat neglected tropical diseases and improve the lives of 1.6 billion people at the reaching the Last Mile Forum at COP28. Gates Foundation https://www.gatesfoundation.org/ideas/media-center/press-releases/2023/12/reaching-the-last-mile-ntds-cop28 (2023).
Adekeye, O. et al. Mass administration of medicines in changing contexts: acceptability, adaptability and community directed approaches in Kaduna and Ogun states, Nigeria. PLoS Negl. Trop. Dis. 14, e0008857 (2020).
Kabona, G. Sustainability plan—lesson learnt on neglected tropical diseases in Tanzania—a mini review. J. Infect. Dis. Travel Med. 6, 1–4 (2022).
Liese, B. H. & Schubert, L. Official development assistance for health—how neglected are neglected tropical diseases? An analysis of health financing. Int. Health 1, 141–147 (2009).
Liese, B. H., Houghton, N. & Teplitskaya, L. Development assistance for neglected tropical diseases: progress since 2009. Int. Health 6, 162–171 (2014).
Ocholaid, E. A., Karanja, D. M. S. & Elliott, S. J. The impact of neglected tropical diseases (NTDs) on health and wellbeing in sub-Saharan Africa (SSA): a case study of Kenya. PLoS Negl. Trop. Dis. 15, e0009131 (2021).
Dorkenoo, M. A. et al. Monitoring migrant groups as a post-validation surveillance approach to contain the potential reemergence of lymphatic filariasis in Togo. Parasit. Vectors 14, 134 (2021).
African Union. Call to action: Africa’s new public health order. africacdc.org https://africacdc.org/news-item/call-to-action-africas-new-public-health-order/ (2022).
Flueckiger, R. M. et al. Integrating data and resources on neglected tropical diseases for better planning: the NTD Mapping Tool (NTDmap.org). PLoS Negl. Trop. Dis. 9, e0003400 (2015).
Makaula, P. et al. An assessment of implementation and effectiveness of mass drug administration for prevention and control of schistosomiasis and soil-transmitted helminths in selected southern Malawi districts. BMC Health Serv. Res. 22, 517 (2022).
Krentel, A. et al. Review of the factors influencing the motivation of community drug distributors towards the control and elimination of neglected tropical diseases (NTDs). PLoS Negl. Trop. Dis. 11, e0006065 (2017).
Krentel, A., Gyapong, M., Ogundahunsi, O., Amuyunzu-Nyamongo, M. & McFarland, D. A. Ensuring no one is left behind: urgent action required to address implementation challenges for NTD control and elimination. PLoS Negl. Trop. Dis. 12, e0006426 (2018).
Martin, S. et al. Evaluating the feasibility and acceptability of a community dialogue intervention in the prevention and control of schistosomiasis in Nampula province, Mozambique. PLoS ONE 16, e0255647 (2021).
Mensah, E. O. et al. Extent of integration of priority interventions into general health systems: a case study of neglected tropical diseases programme in the Western Region of Ghana. PLoS Negl. Trop. Dis. 10, e0004725 (2016).
Dembélé, M. et al. Implementing preventive chemotherapy through an integrated national neglected tropical disease control program in Mali. PLoS Negl. Trop. Dis. 6, e1574 (2012).
Lankester, F. et al. An integrated health delivery platform, targeting soil-transmitted helminths (STH) and canine mediated human rabies, results in cost savings and increased breadth of treatment for STH in remote communities in Tanzania. BMC Public Health 19, 1398 (2019).
Banda, G. T., Deribe, K. & Davey, G. How can we better integrate the prevention, treatment, control and elimination of neglected tropical diseases with other health interventions? A systematic review. BMJ Glob. Health 6, e006968 (2021).
Chowdhury, S. et al. A holistic approach to well-being and neglected tropical diseases: evaluating the impact of community-led support groups in Nigeria using community-based participatory research. Int. Health 15, i87–i99 (2023).
Gichuki, P. M. et al. Using community-based participatory approaches to improve access to mass drug administration for trachoma elimination in a pastoral conflict area of Kenya. PLoS Negl. Trop. Dis. 18, e0012653 (2024).
Madon, S. et al. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: a pilot project in Tanzania. Soc. Sci. Med. 202, 28–37 (2018).
WHO. WHO certifies Ghana free of dracunculiasis. who.int https://www.who.int/news/item/16-01-2015-who-certifies-ghana-free-of-dracunculiasis (2015).
Hofstraat, K. & van Brakel, W. H. Social stigma towards neglected tropical diseases: a systematic review. Int. Health 8, i53–i70 (2016).
Dharmawan, Y., Fuady, A., Korfage, I. & Richardus, J. H. Individual and community factors determining delayed leprosy case detection: a systematic review. PLoS Negl. Trop. Dis. 15, e0009651 (2021).
Tabi, M. M., Powell, M. & Hodnicki, D. Use of traditional healers and modern medicine in Ghana. Int. Nurs. Rev. 53, 52–58 (2006).
Nxumalo, N., Alaba, O., Harris, B., Chersich, M. & Goudge, J. Utilization of traditional healers in South Africa and costs to patients: findings from a national household survey. J. Public Health Policy 32, S124–S136 (2011).
Merritt, R. W., Benbow, M. E. & Small, P. L. Unraveling an emerging disease associated with disturbed aquatic environments: the case of Buruli ulcer. Front. Ecol. Environ. 3, 323–331 (2005).
Weir, E. Buruli ulcer: the third most common mycobacterial infection. CMAJ 166, 1691 (2002).
Wagner, T., Benbow, M. E., Brenden, T. O., Qi, J. & Johnson, R. C. Buruli ulcer disease prevalence in Benin, West Africa: associations with land use/cover and the identification of disease clusters. Int. J. Health Geogr. 7, 25 (2008).
Landier, J. et al. Spatio-temporal patterns and landscape-associated risk of Buruli ulcer in Akonolinga, Cameroon. PLoS Negl. Trop. Dis. 8, e3123 (2014).
WHO. Control of neglected tropical diseases. who.int https://www.who.int/teams/control-of-neglected-tropical-diseases (2024).
International Coalition for Trachoma Control. Key statistics. trachomacoalition.org https://www.trachomacoalition.org/about-trachoma/key-facts (2025).
Rifkin, S. B. Examining the links between community participation and health outcomes: a review of the literature. Health Policy Plan. 29, ii98–ii106 (2014).
Hardwick, R. J. et al. Individual adherence to mass drug administration in neglected tropical disease control: a probability model conditional on past behaviour. PLoS Negl. Trop. Dis. 15, e0009112 (2021).
Vande Velde, F., Overgaard, H. J. & Bastien, S. Nudge strategies for behavior-based prevention and control of neglected tropical diseases: a scoping review and ethical assessment. PLoS Negl. Trop. Dis. 15, e0009239 (2021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Caroline Ackley and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gyapong, J.O., Gohoho, M., Manyeh, A.K. et al. Current state and future directions of interventions for neglected tropical diseases. Nat Hum Behav 9, 1557–1570 (2025). https://doi.org/10.1038/s41562-025-02219-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41562-025-02219-0