Abstract
Evidence supporting the use of coronary physiology as an adjunct to coronary angiography to guide percutaneous coronary interventions has accumulated over the past 25 years. The fractional flow reserve has dominated this evolving physiological guidance of coronary intervention and its use is supported by large clinical outcome trials. However, despite clinical practice guidelines advocating its use in most patients with coronary stenosis who are eligible for coronary intervention, the uptake of a physiology-guided approach remains limited. The use of non-hyperaemic coronary pressure measurements to guide coronary interventions was introduced in an attempt to simplify the routine application of coronary physiology-guided intervention in daily practice. Over the past decade, a large scientific effort has focused on the development of several non-hyperaemic pressure ratios. In this Review, we detail the basic principles of coronary physiology in non-hyperaemic conditions, the rationale for the use of non-hyperaemic coronary pressure measurements for stenosis evaluation, the current evidence base for the available non-hyperaemic coronary pressure ratios, the basis for the discordance between non-hyperaemic coronary pressure ratios and fractional flow reserve, and the potential advantages of these new parameters over fractional flow reserve.
Key points
-
The loss of pressure across a coronary stenosis under non-hyperaemic conditions is intrinsically related to the vasodilatory capacity of the coronary circulation, which, in contrast to fractional flow reserve (FFR), is not informative about the degree of reduction in coronary flow attributable to the stenosis.
-
Non-hyperaemic coronary pressure ratios provide an equivalent diagnostic efficacy as the FFR to identify myocardial perfusion abnormalities on cardiac PET perfusion studies.
-
The use of the instantaneous wave-free ratio to guide coronary interventions results in fewer revascularizations, while maintaining non-inferior 1-year clinical outcomes, compared with the use of FFR.
-
Alternative non-hyperaemic coronary pressure ratios have very high diagnostic efficacy compared with the instantaneous wave-free ratio as well as a similar diagnostic agreement with FFR; however, these indices have not been prospectively studied in terms of clinical outcomes.
-
Non-hyperaemic pressure ratios might provide some benefits in the evaluation of serial coronary stenosis and diffuse epicardial coronary artery disease owing to the lack of stenosis crosstalk for a wide range of stenosis severities under non-hyperaemic conditions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Pijls, N. H. et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N. Engl. J. Med. 334, 1703–1708 (1996).
van Nunen, L. X. et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. Lancet 386, 1853–1860 (2015).
Xaplanteris, P. et al. Five-year outcomes with PCI guided by fractional flow reserve. N. Engl. J. Med. 379, 250–259 (2018).
Fearon, W. F. et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 122, 2545–2550 (2010).
Knuuti, J. et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 41, 407–477 (2020).
Levine, G. N. et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. J. Am. Coll. Cardiol. 58, e44–e122 (2011).
Götberg, M. et al. The evolving future of instantaneous wave-free ratio and fractional flow reserve. J. Am. Coll. Cardiol. 70, 1379–1402 (2017).
Ntalianis, A. et al. Effective radiation dose, time, and contrast medium to measure fractional flow reserve. JACC Cardiovasc. Interv. 3, 821–827 (2010).
Patel, M. R. et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 69, 2212–2241 (2017).
Camici, P. G. & Crea, F. Coronary microvascular dysfunction. N. Engl. J. Med. 356, 830–840 (2007).
Gould, K. L. Pressure-flow characteristics of coronary stenoses in unsedated dogs at rest and during coronary vasodilation. Circ. Res. 43, 242–253 (1978).
Zijlstra, F., Reiber, J. H. C. & Serruys, P. W. Does intracoronary papaverine dilate epicardial coronary arteries? Implications for the assessment of coronary flow reserve. Cathet. Cardiovasc. Diagn. 14, 1–6 (1988).
Jones, C. J., Kuo, L., Davis, M. J. & Chilian, W. M. Myogenic and flow-dependent control mechanisms in the coronary microcirculation. Basic. Res. Cardiol. 88, 2–10 (1993).
Chilian, W. M. Coronary microcirculation in health and disease: summary of an NHLBI workshop. Circulation 95, 522–528 (1997).
DeFily, D. V. & Chilian, W. M. Coronary microcirculation: autoregulation and metabolic control. Basic Res. Cardiol. 90, 112–118 (1995).
Tune, J. D., Gorman, M. W. & Feigl, E. O. Matching coronary blood flow to myocardial oxygen consumption. J. Appl. Physiol. 97, 404–415 (2004).
van de Hoef, T. P. et al. Coronary pressure-flow relations as basis for the understanding of coronary physiology. J. Mol. Cell. Cardiol. 52, 786–793 (2012).
van de Hoef, T. P. et al. Fractional flow reserve as a surrogate for inducible myocardial ischaemia. Nat. Rev. Cardiol. 10, 439–452 (2013).
Kuo, L., Chilian, W. M. & Davis, M. J. Coronary arteriolar myogenic response is independent of endothelium. Circ. Res. 66, 860–866 (1990).
Feliciano, L. & Henning, R. J. Coronary artery blood how: physiologic and pathophysiologic regulation. Clin. Cardiol. 22, 775–786 (1999).
Gould, K. L. & Lipscomb, K. Effects of coronary stenoses on coronary flow reserve and resistance. Am. J. Cardiol. 34, 48–55 (1974).
Gould, K. L., Lipscomb, K. & Calvert, C. Compensatory changes of the distal coronary vascular bed during progressive coronary constriction. Circulation 51, 1085–1094 (1975).
Pijls, N. H. J., van Son, J. A. M., Kirkeeide, R. L., De Bruyne, B. & Gould, K. L. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation 87, 1354–1367 (1993).
Nijjer, S. S. et al. Coronary pressure and flow relationships in humans: phasic analysis of normal and pathological vessels and the implications for stenosis assessment: a report from the Iberian-Dutch-English (IDEAL) collaborators. Eur. Heart J. 37, 2069–2080 (2016).
Lee, J. M. et al. Exploring coronary circulatory response to stenosis and its association with invasive physiologic indexes using absolute myocardial blood flow and coronary pressure. Circulation 136, 1798–1808 (2017).
Johnson, N. P. & Gould, K. L. Physiological basis for angina and ST-segment change: PET-verified thresholds of quantitative stress myocardial perfusion and coronary flow reserve. JACC Cardiovasc. Imaging 4, 990–998 (2011).
Gould, K. L. et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J. Am. Coll. Cardiol. 62, 1639–1653 (2013).
Grüntzig, A. R., Senning, Å. & Siegenthaler, W. E. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty. N. Engl. J. Med. 301, 61–68 (1979).
Mamas, M. A. et al. Resting Pd/Pa measured with intracoronary pressure wire strongly predicts fractional flow reserve. J. Invasive Cardiol. 22, 260–265 (2010).
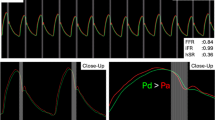
Sen, S. et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J. Am. Coll. Cardiol. 59, 1392–1402 (2012).
Petraco, R. et al. ECG-independent calculation of instantaneous wave-free ratio. JACC Cardiovasc. Interv. 8, 2043–2046 (2015).
Johnson, N. P. et al. Diastolic pressure ratio: new approach and validation vs. the instantaneous wave-free ratio. Eur. Heart J. 40, 2585–2594 (2019).
Svanerud, J. et al. Validation of a novel non-hyperaemic index of coronary artery stenosis severity: the resting full-cycle ratio (VALIDATE RFR) study. EuroIntervention 14, 806–814 (2018).
Escaned, J. et al. Prospective assessment of the diagnostic accuracy of instantaneous wave-free ratio to assess coronary stenosis relevance: results of ADVISE II international, multicenter study (ADenosine Vasodilator Independent Stenosis Evaluation II). JACC Cardiovasc. Interv. 8, 824–833 (2015).
Petraco, R. et al. Classification performance of instantaneous wave-free ratio (iFR) and fractional flow reserve in a clinical population of intermediate coronary stenoses: results of the ADVISE registry. EuroIntervention 9, 91–101 (2013).
Jeremias, A. et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting P/P with fractional flow reserve: the RESOLVE study. J. Am. Coll. Cardiol. 63, 1253–1261 (2014).
Lee, J. M. et al. Physiological and clinical assessment of resting physiological indexes. Circulation 139, 889–900 (2019).
van’t Veer, M. et al. Comparison of different diastolic resting indexes to iFR: are they all equal? J. Am. Coll. Cardiol. 70, 3088–3096 (2017).
Kumar, G. et al. Real world validation of the nonhyperemic index of coronary artery stenosis severity-Resting full-cycle ratio-RE-VALIDATE. Catheter. Cardiovasc. Interv. https://doi.org/10.1002/ccd.28523 (2019).
Hwang, D. et al. Diagnostic performance of resting and hyperemic invasive physiological indices to define myocardial ischemia: validation with 13N-ammonia positron emission tomography. JACC Cardiovasc. Interv. 10, 751–760 (2017).
de Waard, G. A. et al. Fractional flow reserve, instantaneous wave-free ratio, and resting Pd/Pa compared with [15O]H2O positron emission tomography myocardial perfusion imaging: a PACIFIC trial sub-study. Eur. Heart J. 39, 4072–4081 (2018).
Lee, J. M. et al. Similarity and difference of resting distal to aortic coronary pressure and instantaneous wave-free ratio. J. Am. Coll. Cardiol. 70, 2114–2123 (2017).
Petraco, R. et al. Baseline instantaneous wave-free ratio as a pressure-only estimation of underlying coronary flow reserve: results of the JUSTIFY-CFR study (Joined coronary pressure and flow analysis to determine diagnostic characteristics of basal and hyperemic indices of functional lesion severity-coronary flow reserve). Circ. Cardiovasc. Interv. 7, 492–502 (2014).
Cook, C. M. et al. Fractional flow reserve/instantaneous wave-free ratio discordance in angiographically intermediate coronary stenoses: an analysis using Doppler-derived coronary flow measurements. JACC Cardiovasc. Interv. 10, 2514–2524 (2017).
Sen, S. et al. Diagnostic classification of the instantaneous wave-free ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Results of CLARIFY (the CLassification Accuracy of pressure-only Ratios against Indices using Flows. J. Am. Coll. Cardiol. 61, 1409–1420 (2013).
van de Hoef, T. P. et al. Diagnostic accuracy of combined intracoronary pressure and flow velocity information during baseline conditions: adenosine-free assessment of functional coronary lesion severity. Circ. Cardiovasc. Interv. 5, 508–514 (2012).
van de Hoef, T. P. et al. Head-to-head comparison of basal stenosis resistance index, instantaneous wave-free ratio, and fractional flow reserve: diagnostic accuracy for stenosis-specific myocardial ischaemia. EuroIntervention 11, 914–925 (2015).
Cook, C. M. et al. Quantification of the effect of pressure wire drift on the diagnostic performance of fractional flow reserve, instantaneous wave-free ratio, and whole-cycle Pd/Pa. Circ. Cardiovasc. Interv. 9, e002988 (2016).
Davies, J. E. et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N. Engl. J. Med. 376, 1824–1834 (2017).
Götberg, M. et al. Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N. Engl. J. Med. 376, 1813–1823 (2017).
Escaned, J. et al. Safety of the deferral of coronary revascularization on the basis of instantaneous wave-free ratio and fractional flow reserve measurements in stable coronary artery disease and acute coronary syndromes. JACC Cardiovasc. Interv. 11, 1437–1449 (2018).
Wijntjens, G. W. M. et al. Prognostic implications of resting distal coronary-to-aortic pressure ratio compared with fractional flow reserve: a 10-year follow-up study after deferral of revascularisation. Neth. Heart J. 28, 96–103 (2020).
Lee, J. M. et al. Clinical outcome of lesions with discordant results among different invasive physiologic indices — resting distal coronary to aortic pressure ratio, resting full-cycle ratio, diastolic pressure ratio, instantaneous wave-free ratio, and fractional flow reserve. Circ. J. 83, 2210–2221 (2019).
Sen, S. et al. Clinical events after deferral of LAD revascularization following physiological coronary assessment. J. Am. Coll. Cardiol. 73, 444–453 (2019).
Thim, T. et al. Nonculprit stenosis evaluation using instantaneous wave-free ratio in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc. Interv. 10, 2528–2535 (2017).
De Rosa, S. et al. Reliability of instantaneous wave-free ratio (iFR) for the evaluation of left main coronary artery lesions. J. Clin. Med. 8, 1143 (2019).
Warisawa, T. DEFINE-LM: revascularization deferral in patients with left main coronary artery disease based on iFR evaluation [abstract]. Presented at Transcatheter Cardiovascular Therapeutics (2019).
Lee, J. M. et al. Comparison of major adverse cardiac events between instantaneous wave-free ratio and fractional flow reserve-guided strategy in patients with or without type 2 diabetes: a secondary analysis of a randomized clinical trial. JAMA Cardiol. 4, 857 (2019).
Kim, C. H. et al. Sex differences in instantaneous wave-free ratio or fractional flow reserve–guided revascularization strategy. JACC Cardiovasc. Interv. 12, 2035–2046 (2019).
Matsumoto, H. et al. Effect of caffeine on intravenous adenosine-induced hyperemia in fractional flow reserve measurement. J. Invasive Cardiol. 26, 580–585 (2014).
Matsumoto, H. et al. Is caffeine abstention necessary before adenosine-induced fractional flow reserve measurement? J. Am. Coll. Cardiol. 66, 1943–1945 (2015).
Adjedj, J. et al. Intracoronary adenosine: dose–response relationship with hyperemia. JACC Cardiovasc. Interv. 8, 1422–1430 (2015).
Wijntjens, G. W. M. et al. Individual lesion-level meta-analysis comparing various doses of intracoronary bolus injection of adenosine with intravenous administration of adenosine for fractional flow reserve assessment. Circ. Cardiovasc. Interv. 13, e007893 (2020).
Toth, G. G. et al. Standardization of fractional flow reserve measurements. J. Am. Coll. Cardiol. 68, 742–753 (2016).
Berry, C. et al. VERIFY (VERification of Instantaneous Wave-free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): a multicenter study in consecutive patients. J. Am. Coll. Cardiol. 61, 1421–1427 (2013).
Petraco, R. et al. Fractional flow reserve-guided revascularization: practical implications of a diagnostic gray zone and measurement variability on clinical decisions. JACC Cardiovasc. Interv. 6, 222–225 (2013).
van de Hoef, T. P., Siebes, M., Spaan, J. A. E. & Piek, J. J. Fundamentals in clinical coronary physiology: why coronary flow is more important than coronary pressure. Eur. Heart J. 36, 3312–3319 (2015).
van de Hoef, T. P. et al. Contribution of age-related microvascular dysfunction to abnormal coronary: hemodynamics in patients with ischemic heart disease. JACC Cardiovasc. Interv. 13, 20–29 (2020).
van de Hoef, T. P. et al. Impact of hyperaemic microvascular resistance on fractional flow reserve measurements in patients with stable coronary artery disease: Insights from combined stenosis and microvascular resistance assessment. Heart 100, 951–959 (2014).
Lee, J. M. et al. Discrepancy between fractional flow reserve and instantaneous wave-free ratio: Clinical and angiographic characteristics. Int. J. Cardiol. 245, 63–68 (2017).
Lee, J. M. et al. Prognostic implication of thermodilution coronary flow reserve in patients undergoing fractional flow reserve measurement. JACC Cardiovasc. Interv. 11, 1423–1433 (2018).
van de Hoef, T. P. et al. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ. Cardiovasc. Interv. 7, 301–311 (2014).
Lee, S. H. et al. Physiologic characteristics and clinical outcomes of patients with discordance between FFR and iFR. JACC Cardiovasc. Interv. 12, 2018–2031 (2019).
Echavarría-Pinto, M. et al. Combining baseline distal-to-aortic pressure ratio and fractional flow reserve in the assessment of coronary stenosis severity. JACC Cardiovasc. Interv. 8, 1681–1691 (2015).
Wijntjens, G. W. M. et al. Pressure-derived estimations of coronary flow reserve are inferior to flow-derived coronary flow reserve as diagnostic and risk stratification tools. Int. J. Cardiol. 279, 6–11 (2019).
de Bruyne, B. et al. Pressure-derived fractional flow reserve to assess serial epicardial stenoses: theoretical basis and animal validation. Circulation 101, 1840–1847 (2000).
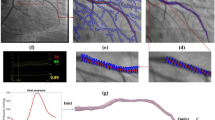
Nijjer, S. S. et al. The instantaneous wave-free ratio (iFR) pullback: a novel innovation using baseline physiology to optimise coronary angioplasty in tandem lesions. Cardiovasc. Revasc. Med. 16, 167–171 (2015).
Gould, K. L., Lipscomb, K. & Hamilton, G. W. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am. J. Cardiol. 33, 87–94 (1974).
Nijjer, S. S. et al. Pre-angioplasty instantaneous wave-free ratio pullback provides virtual intervention and predicts hemodynamic outcome for serial lesions and diffuse coronary artery disease. JACC Cardiovasc. Interv. 7, 1386–1396 (2014).
Kikuta, Y. et al. Pre-angioplasty instantaneous wave-free ratio pullback predicts hemodynamic outcome in humans with coronary artery disease: primary results of the International Multicenter iFR GRADIENT registry. JACC Cardiovasc. Interv. 11, 757–767 (2018).
Higashioka, D. et al. The inter-study reproducibility of instantaneous wave-free ratio and angiography coregistration. J. Cardiol. 75, 507–512 (2019).
Frimerman, A. et al. Novel method for real-time coregistration of coronary physiology and angiography by iFR. JACC Cardiovasc. Interv. 12, 692–694 (2019).
Author information
Authors and Affiliations
Contributions
T.P.v.d.H. researched data and wrote the article. All the authors contributed to discussion of content and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
T.P.v.d.H. has been a speaker at educational events for Boston Scientific, Philips Volcano and St. Jude Medical (Abbott), and a consultant for Philips Volcano. J.M.L. has received research grant support from Philips Volcano and St. Jude Medical (Abbott). M.E.-P. has been a speaker at educational events for Abbott and Philips Volcano. B.-K.K. has received institutional research grant support from Philips Volcano and St. Jude Medical (Abbott). M.R.P. has received grants and personal fees from AstraZeneca, Janssen and Philips Volcano, and personal fees from Bayer. J.E.D. has received research funding from AstraZeneca and Philips Volcano, and consulting fees from Medtronic, Philips Volcano and ReCor Medical, and holds patents pertaining to the instantaneous wave-free ratio technology, which is under license to Volcano Corporation. J.E. has been a speaker at educational events and a consultant for Abbott, Boston Scientific and Philips Volcano. J.J.P. has received institutional research grant support from Philips Volcano and personal fees from Abbott, Miracor and Philips Volcano. H.M. declares no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks M. J. Kern and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van de Hoef, T.P., Lee, J.M., Echavarria-Pinto, M. et al. Non-hyperaemic coronary pressure measurements to guide coronary interventions. Nat Rev Cardiol 17, 629–640 (2020). https://doi.org/10.1038/s41569-020-0374-z
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-020-0374-z
This article is cited by
-
Validation of resting full-cycle ratio and diastolic pressure ratio with [15O]H2O positron emission tomography myocardial perfusion
Heart and Vessels (2024)
-
Insufficient adenosine-induced hyperemia is a major determinant of discordance between non-hyperemic pressure ratio and fractional flow reserve
Scientific Reports (2023)
-
Impact of overestimation of fractional flow reserve by adenosine on anatomical–functional mismatch
Scientific Reports (2022)
-
Diagnostic agreement of quantitative flow ratio with fractional flow reserve in a Latin-American population
The International Journal of Cardiovascular Imaging (2022)