Abstract
Cardiac rehabilitation is a complex intervention that seeks to improve the functional capacity, wellbeing and health-related quality of life of patients with heart disease. A substantive evidence base supports cardiac rehabilitation as a clinically effective and cost-effective intervention for patients with acute coronary syndrome or heart failure with reduced ejection fraction and after coronary revascularization. In this Review, we discuss the major contemporary challenges that face cardiac rehabilitation. Despite the strong recommendation in current clinical guidelines for the referral of these patient groups, global access to cardiac rehabilitation remains poor. The COVID-19 pandemic has contributed to a further reduction in access to cardiac rehabilitation. An increasing body of evidence supports home-based and technology-based models of cardiac rehabilitation as alternatives or adjuncts to traditional centre-based programmes, especially in low-income and middle-income countries, in which cardiac rehabilitation services are scarce, and scalable and affordable models are much needed. Future approaches to the delivery of cardiac rehabilitation need to align with the growing multimorbidity of an ageing population and cater to the needs of the increasing numbers of patients with cardiac disease who present with two or more chronic diseases. Future research priorities include strengthening the evidence base for cardiac rehabilitation in other indications, including heart failure with preserved ejection fraction, atrial fibrillation and congenital heart disease and after valve surgery or heart transplantation, and evaluation of the implementation of sustainable and affordable models of delivery that can improve access to cardiac rehabilitation in all income settings.
Key points
-
Cardiac rehabilitation is a complex, multicomponent intervention that includes exercise training and physical activity promotion, health education, cardiovascular risk management and psychological support, personalized to the individual needs of patients with heart disease.
-
Data from randomized, controlled trials support cardiac rehabilitation as a clinically effective and cost-effective intervention for patients with acute coronary syndrome or heart failure with reduced ejection fraction and after coronary revascularization.
-
Despite this robust evidence base and strong guideline recommendations, global access to cardiac rehabilitation is persistently poor, with scarce cardiac rehabilitation provision in low-income and middle-income settings.
-
Home-based and technology-based models of cardiac rehabilitation with appropriate quality assurance as an alternative or adjunct to traditional, centre-based programmes are needed to improve access to cardiac rehabilitation.
-
Cardiac rehabilitation programmes need to cater for and manage the needs of the increasing number of patients with heart disease who present with two or more chronic diseases.
-
Further research needs to strengthen the evidence base for cardiac rehabilitation in patients with heart failure with preserved ejection fraction, atrial fibrillation or congenital heart disease and after cardiac valve surgery or heart transplantation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Richardson, C. R., Franklin, B., Moy, M. L. & Jackson, E. A. Advances in rehabilitation for chronic diseases: improving health outcomes and function. BMJ 365, l2191 (2019).
Dempster, M. & Donnelly, M. Measuring the health related quality of life of people with ischaemic heart disease. Heart 83, 641–644 (2000).
Taylor, R., Dibben, G., Faulkner, J. & Dalal, H. More evidence of cardiac rehabilitation: need to consider patient quality of life. Can. J. Cardiol. https://doi.org/10.1016/j.cjca.2021.01.012 (2021).
Cook, R., Davidson, P. & Martin, R. et al. Cardiac rehabilitation for heart failure can improve quality of life and fitness. BMJ 367, l5456 (2019).
Ambrosetti, M. et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 28, 460–495 (2021).
BACPR. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2017 (3rd Edition) https://www.bacpr.com/resources/BACPR_Standards_and_Core_Components_2017.pdf (2017).
Abreu, A. et al. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: the avenue towards EAPC accreditation programme: a position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC). Eur. J. Prev. Cardiol. 28, 496–509 (2021).
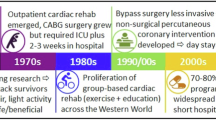
Kavanagh, T. in Cardiac Rehabilitation (eds Jones, D. & West, R.) 4–30 (BMJ Publishing Group, 1995).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926 (2008).
Faulkner, J. et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. (in press).
Anderson, L. et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 3, CD001800 (2016).
West, R. R., Jones, D. A. & Henderson, A. H. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 98, 637–644 (2012).
Rauch, B. et al. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: a systematic review and meta-analysis of randomized and non-randomized studies - The Cardiac Rehabilitation Outcome Study (CROS). Eur. J. Prev. Cardiol. 23, 1914–1939 (2016).
Salzwedel, A. et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur. J. Prev. Cardiol. 27, 1756–1774 (2020).
Long, L. et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 1, CD003331 (2019).
American Thoracic Society. Minnesota Living with Heart Failure questionnaire http://qol.thoracic.org/sections/instruments/ko/pages/mlwhfq.html (2004).
Risom, S. S. et al. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst. Rev. 2, CD011197 (2017).
Williams, C. A. et al. Physical activity interventions for people with congenital heart disease. Cochrane Database Syst. Rev. 10, CD013400 (2020).
Nielsen, K. M. et al. Exercise-based cardiac rehabilitation for adult patients with an implantable cardioverter defibrillator. Cochrane Database Syst. Rev. 2, CD011828 (2019).
Anderson, L. et al. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst. Rev. 4, CD012264 (2017).
Abraham, L. N. et al. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst. Rev. 5, CD010876 (2021).
Higgins, J. P. T. Cochrane handbook for systematic reviews of interventions version 6.2. Cochrane Training https://training.cochrane.org/handbook (2021).
Scherrenberg, M. et al. Is there an optimal dose of cardiac rehabilitation in coronary artery disease patients? Int. J. Cardiol. 330, 7–11 (2021).
Nichols, S. et al. Routine exercise-based cardiac rehabilitation does not increase aerobic fitness: a CARE CR study. Int. J. Cardiol. 305, 25–34 (2020).
Ganga, H. V. et al. Supervised exercise training versus usual care in ambulatory patients with left ventricular assist devices: a systematic review. PLoS ONE 12, e0174323 (2017).
Tajrishi, F. Z. et al. Spontaneous coronary artery dissection and associated myocardial bridging: current evidence from cohort study and case reports. Med. Hypotheses 128, 50–53 (2019).
Wang, H. L. et al. Exercise interventions in cardio-oncology populations: a scoping review of the literature. J. Cardiovasc. Nurs. 36, 385–404 (2021).
Shields, G. E. et al. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart 104, 1403–1410 (2018).
Rawlins, M. D. & Culyer, A. J. National Institute for Clinical Excellence and its value judgments. BMJ 329, 224–227 (2004).
Knuuti, J. et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 41, 407–477 (2020).
Ponikowski, P. et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 18, 891–975 (2016).
Smith, S. C. Jr et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a Guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. J. Am. Coll. Cardiol. 58, 2432–2446 (2011).
Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 62, e147–e239 (2013).
NICE. Acute coronary syndromes: NICE guideline [NG185]. https://www.nice.org.uk/guidance/NG185 (2020).
NICE. Chronic heart failure in adults: diagnosis and management: NICE guideline [NG106]. https://www.nice.org.uk/guidance/ng106 (2018).
Chew, D. P. et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes. Med. J. Aust. 205, 128–133 (2016).
Atherton, J. J. et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: guidelines for the prevention, detection, and management of heart failure in Australia 2018. Heart Lung Circ. 27, 1123–1208 (2018).
Thomas, R. J. et al. Home-based cardiac rehabilitation: a scientific statement from the American association of cardiovascular and pulmonary rehabilitation, the American Heart Association, and the American College of Cardiology. J. Am. Coll. Cardiol. 74, 133–153 (2019).
Price, K. J. et al. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus? Eur. J. Prev. Cardiol. 23, 1715–1733 (2016).
BHF. National Audit of Cardiac Rehabilitation (NACR) Quality and Outcomes Report 2019. https://www.bhf.org.uk/informationsupport/publications/statistics/national-audit-of-cardiac-rehabilitation-quality-and-outcomes-report-2019 (2019).
Peters, A. E. & Keeley, E. C. Trends and predictors of participation in cardiac rehabilitation following acute myocardial infarction: data from the behavioral risk factor surveillance system. J. Am. Heart Assoc. 7, e007664 (2017).
Ruano-Ravina, A. et al. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int. J. Cardiol. 223, 436–443 (2016).
Ragupathi, L. et al. Availability, use, and barriers to cardiac rehabilitation in LMIC. Glob. Heart 12, 323–334.e10 (2017).
Kotseva, K. et al. Use and effects of cardiac rehabilitation in patients with coronary heart disease: results from the EUROASPIRE III survey. Eur. J. Prev. Cardiol. 20, 817–826 (2013).
NHS. Long-term Plan. Cardiovascular disease. https://www.longtermplan.nhs.uk/online-version/chapter-3-further-progress-on-care-quality-and-outcomes/better-care-for-major-health-conditions/cardiovascular-disease/ (2019).
Ades, P. A. et al. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin. Proc. 92, 234–242 (2017).
Dalal, H. M. et al. The effects and costs of home-based rehabilitation for heart failure with reduced ejection fraction: the REACH-HF multicentre randomized controlled trial. Eur. J. Prev. Cardiol. 26, 262–272 (2019).
Taylor, R. S. et al. The cost effectiveness of REACH-HF and home-based cardiac rehabilitation compared with the usual medical care for heart failure with reduced ejection fraction: a decision model-based analysis. Eur. J. Prev. Cardiol. 26, 1252–1261 (2019).
Purcell, C. et al. Protocol for an implementation study of an evidence-based home cardiac rehabilitation programme for people with heart failure and their caregivers in Scotland (SCOT:REACH-HF). BMJ Open 10, e040771 (2020).
Daw, P. et al. Getting evidence into clinical practice: protocol for evaluation of the implementation of a home-based cardiac rehabilitation programme for patients with heart failure. BMJ Open 10, e036137 (2020).
Harrison, A. S. & Doherty, P. Does the mode of delivery in routine cardiac rehabilitation have an association with cardiovascular risk factor outcomes? Eur. J. Prev. Cardiol. 25, 1925–1933 (2018).
Buckingham, S. A. et al. Home-based versus centre-based cardiac rehabilitation: abridged Cochrane systematic review and meta-analysis. Open Heart 3, e000463 (2016).
Imran, H. M. et al. Home-Based cardiac rehabilitation alone and hybrid with center-based cardiac rehabilitation in heart failure: a systematic review and meta-analysis. J. Am. Heart Assoc. 8, e012779 (2019).
Thomas, R. J. et al. Home-based cardiac rehabilitation: a scientific statement from the american association of cardiovascular and pulmonary rehabilitation, the American Heart Association, and the American College of Cardiology. J. Am. Coll. Cardiol. 74, 133–153 (2019).
Hartley, D. M., Reisinger, H. S. & Perencevich, E. N. When infection prevention enters the temple: intergenerational social distancing and COVID-19. Infect. Control Hosp. Epidemiol. 41, 868–869 (2020).
Guo, T. et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 5, 811–818 (2020).
Nishiga, M. et al. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 17, 543–558 (2020).
Schimelpfenig, N. What does a stay-at-home order mean? 11 questions answered. Healthline. https://www.healthline.com/health-news/what-a-stay-at-home-order-means (2020).
Babu, A. S., Arena, R., Ozemek, C. & Lavie, C. J. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can. J. Cardiol. 36, 792–794 (2020).
Scherrenberg, M. et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 28, 524–540 (2021).
Doherty, P. & Harrison, A. Investigation of the impact of COVID-19 on UK CR: what can we learn from this experience? [abstract]. Presented at the 2020 BACPR Annual Conference (2020).
Buckingham, S. A. et al. Home-based versus centre-based cardiac rehabilitation: abridged Cochrane systematic review and meta-analysis. Open Heart 3, e000463 (2016).
Rawstorn, J. C. et al. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart 102, 1183–1192 (2016).
Thomas, R. J. et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J. Am. Coll. Cardiol. 71, 1814–1837 (2018).
Vishwanath, V., Beckman, A. L. & Kazi, D. S. Reimagining cardiac rehabilitation in the era of coronavirus disease 2019. JAMA Health Forum 1, e201346 (2020).
Thomas, E., Gallagher, R. & Grace, S. L. Future-proofing cardiac rehabilitation: transitioning services to telehealth during COVID-19. Eur. J. Prev. Cardiol. 28, e35–e36 (2021).
Dalal, H. et al. Correspondence to the EJPC in response to position paper by Ambrosetti M et al. 2020 Cardiovascular rehabilitation and COVID-19: the need to maintain access to evidence-based services from the safety of home. Eur. J. Prev. Cardiol. https://doi.org/10.1177/2047487320923053 (2020).
Anderson, M. & Kumar, M. Digital divide persists even as lower-income Americans make gains in tech adoption. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/ (2021).
Balady, G. J. et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation 124, 2951–2960 (2011).
Eberly, L. A. et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation 142, 510–512 (2020).
Nouri, S., Khoong, E. C., Lyles, C. R. & Karliner, L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst https://doi.org/10.1056/CAT.20.0123 (2020).
NICE. COVID-19 ready rehabilitation for heart failure: REACH-HF can deliver. https://www.nice.org.uk/sharedlearning/covid-19-ready-rehabilitation-for-heart-failure-reach-hf-can-deliver (2020).
O’Connor, C. M. et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301, 1439–1450 (2009).
Barnett, K. et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380, 37–43 (2012).
Jani, B. D. et al. Relationship between multimorbidity, demographic factors and mortality: findings from the UK Biobank cohort. BMC Med. 17, 74 (2019).
Makovski, T. T. et al. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res. Rev. 53, 100903 (2019).
Sumner, J., Böhnke, J. R. & Doherty, P. Does service timing matter for psychological outcomes in cardiac rehabilitation? Insights from the National Audit of Cardiac Rehabilitation. Eur. J. Prev. Cardiol. 25, 19–28 (2018).
Barker, K. et al. A rehabilitation programme for people with multimorbidity versus usual care: a pilot randomized controlled trial. J. Comorb. 8, 2235042X18783918 (2018).
Cowie, A., McKay, J. & Keenan, A. Combined generic-specialist multimorbidity rehabilitation post acute cardiac event. Brit. J. Card. Nurs. 13, 340–347 (2018).
Taylor, R. S. & Singh, S. Personalised rehabilitation for cardiac and pulmonary patients with multimorbidity: time for implementation? Eur. J. Prev. Cardiol. https://doi.org/10.1177/2047487320926058 (2020).
GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1859–1922 (2018).
WHO. Global status report on noncommunicable diseases 2010. United Nations Digital Library https://digitallibrary.un.org/record/706319?ln=en (2011).
Turk-Adawi, K. et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine 13, 31–45 (2019).
Global Health Data Exchange. Institute for Health Metrics and Evaluation. GBD results tool. http://ghdx.healthdata.org/gbd-results-tool (2021).
Pesah, E. et al. Cardiac rehabilitation delivery in low/middle-income countries. Heart 105, 1806–1812 (2019).
Taylor, R. S., Grace, S., Mamataz, T., Uddin, J. & Ibn Alam, S. Effects of cardiac rehabilitation in low- and middle-income countries: a systematic review and meta-analyses of randomised controlled trials. https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=185296 (2020).
Uddin, J. et al. Predictors of exercise capacity following exercise-based rehabilitation in patients with coronary heart disease and heart failure: a meta-regression analysis. Eur. J. Prev. Cardiol. 23, 683–693 (2016).
Oldridge, N. B., Pakosh, M. T. & Thomas, R. J. Cardiac rehabilitation in low- and middle-income countries: a review on cost and cost-effectiveness. Int. Health 8, 77–82 (2016).
Salvetti, X. M., Oliveira, J. A., Servantes, D. M. & Vincenzo de Paola, A. A. How much do the benefits cost? Effects of a home-based training programme on cardiovascular fitness, quality of life, programme cost and adherence for patients with coronary disease. Clin. Rehabil. 22, 987–996 (2008).
Uddin, J. et al. Effect of home-based cardiac rehabilitation in a lower-middle income country: results from a controlled trial. J. Cardiopulm. Rehabil. Prev. 40, 29–34 (2020).
Grace, S. L. et al. Cardiac rehabilitation delivery model for low-resource settings: an International Council of Cardiovascular Prevention and Rehabilitation consensus statement. Prog. Cardiovasc. Dis. 59, 303–322 (2016).
Taylor, R., Zwisler, A. D. & Uddin, J. Global health-care systems must prioritise rehabilitation. Lancet 396, 1946–1947 (2021).
WHO. Global status report on noncommunicable diseases 2014. https://apps.who.int/iris/handle/10665/148114 (2014).
WHO. Rehabilitation 2030: a call for action. https://www.who.int/news-room/events/detail/2017/02/06/default-calendar/rehabilitation-2030-a-call-for-action (2017).
Acknowledgements
The authors thank J. Uddin (Physiotherapy Unit, Department of Cardiac Surgery Ibrahim Cardiac Hospital & Research Institute, Dhaka, Bangladesh) for drafting the content of Box 6, G. Dibben (MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, UK) for preparing Fig. 2 for initial submission and U. Ahmed (MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, UK) for editorial review of the text.
Author information
Authors and Affiliations
Contributions
All the authors researched data for the article, contributed substantially to discussions of its content, wrote the article, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
R.S.T. is a member of the ESC Association of Cardiovascular Nursing and Allied Professions (ACNAP) Science Committee 2020–2022 and lead investigator for the following ongoing funded projects: ‘Implementation of an evidence-based cardiac rehabilitation home programme for heart failure patients and their caregivers in Scotland: SCOT:REACH-HF project’, funded by Heart Research UK; ‘A randomized controlled trial of a facilitated home-based rehabilitation intervention in patients with heart failure with preserved ejection fraction and their caregivers: the REACH-HFpEF Study’, funded by NIHR HTA Programme (NIHR130487). H.M.D. is a co-opted member of the British Association of Cardiovascular Prevention and Rehabilitation (BACPR) and a co-lead for the ongoing funded research projects: ‘D REACH-HF: Digital Rehabilitation Enablement in Chronic Heart Failure’, funded by the British Heart Foundation, Hope for Hearts fund’; ‘Extending the reach and implementation of the successful REACH-HF programme with a digitally delivered training programme’, funded by NIHR Programme Development Grant (NIHR202040). S.J.D.M. is a researcher on the following ongoing funded research projects: ‘D REACH-HF: Digital Rehabilitation Enablement in Chronic Heart Failure’, funded by the British Heart Foundation, Hope for Hearts fund’; ‘Extending the reach and implementation of the successful REACH-HF programme with a digitally delivered training programme’, funded by NIHR Programme Development Grant (NIHR202040).
Additional information
Peer review information
Nature Reviews Cardiology thanks D. Forman and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Taylor, R.S., Dalal, H.M. & McDonagh, S.T.J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol 19, 180–194 (2022). https://doi.org/10.1038/s41569-021-00611-7
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-021-00611-7
This article is cited by
-
Merging geographic regions for the analysis of the cardiological rehabilitation care system in Hungary
International Journal of Health Geographics (2026)
-
Development and validation of a multidimensional tool for baseline functional phenotyping in cardiac rehabilitation
BMC Cardiovascular Disorders (2025)
-
Changing physical activity behavior among individuals with inflammatory arthritis: an umbrella review of current behaviors, behavioral determinants, and behavior change interventions
BMC Rheumatology (2025)
-
A multicenter randomized single-blinded clinical trial to investigate the effects of an individualized home-based cognitive training program in patients with chronic heart failure: the SYNAPSE protocol
Trials (2025)
-
The impact of cardiac rehabilitation exercises incorporating music movement therapy on atrial fibrillation patients: a forward-looking investigation
Journal of Cardiothoracic Surgery (2025)