Abstract
Venous thromboembolism, that consists of the interrelated conditions deep-vein thrombosis and pulmonary embolism, is an under-appreciated vascular disease. In Western regions, approximately 1 in 12 individuals will be diagnosed with venous thromboembolism in their lifetime. Rates of venous thromboembolism are lower in Asia, but data from other regions are sparse. Numerous risk factors for venous thromboembolism have been identified, which can be classified as acute or subacute triggers (provoking factors that increase the risk of venous thromboembolism) and basal or acquired risk factors (which can be modifiable or static). Approximately 20% of individuals who have a venous thromboembolism event die within 1 year (although often from the provoking condition), and complications are common among survivors. Fortunately, opportunities exist for primordial prevention (prevention of the development of underlying risk factors), primary prevention (management of risk factors among individuals at high risk of the condition) and secondary prevention (prevention of recurrent events) of venous thromboembolism. In this Review, we describe the epidemiology of venous thromboembolism, including the incidence, risk factors, outcomes and opportunities for prevention. Meaningful health disparities exist in both the incidence and outcomes of venous thromboembolism. We also discuss these disparities as well as opportunities to reduce them.
Key points
-
Venous thromboembolism (VTE) surveillance systems are lacking, but VTE is estimated to affect one to two individuals per 1,000 person-years in Europe and the USA, with lower rates in other regions.
-
Risk factors for VTE are varied, and include triggers (acute and subacute), basal risk factors (demographic, behavioural, anthropometric and genetic) and acquired clinical risk factors.
-
Numerous complications can occur after a VTE event, and quality of life can decrease.
-
Reduction in the risk of VTE and adverse outcomes after a VTE event will require prevention across the spectrum of prevention stages (primordial, primary and secondary) and increased awareness of this under-appreciated condition.
-
Disparities exist in VTE incidence and outcomes; reducing these disparities will require individual, systems-based and societal commitments to equity.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Wendelboe, A. M. & Raskob, G. E. Global burden of thrombosis: epidemiologic aspects. Circ. Res. 118, 1340–1347 (2016).
Bell, E. J. et al. Lifetime risk of venous thromboembolism in two cohort studies. Am. J. Med. 129, 339 e19–339.e26 (2016).
Sogaard, K. K., Schmidt, M., Pedersen, L., Horvath-Puho, E. & Sorensen, H. T. 30-year mortality after venous thromboembolism: a population-based cohort study. Circulation 130, 829–836 (2014).
Kort, D. et al. Relationship between neighborhood socioeconomic status and venous thromboembolism: results from a population-based study. J. Thromb. Haemost. 15, 2352–2360 (2017).
Januel, J. M. et al. Clinical and health system determinants of venous thromboembolism event rates after hip arthroplasty: an international comparison. Med. Care 56, 862–869 (2018).
Wattanakit, K. et al. Association between cardiovascular disease risk factors and occurrence of venous thromboembolism. A time-dependent analysis. Thromb. Haemost. 108, 508–515 (2012).
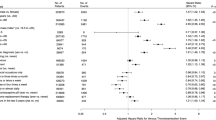
Gregson, J. et al. Cardiovascular risk factors associated with venous thromboembolism. JAMA Cardiol. 4, 163–173 (2019).
Lutsey, P. L. et al. Correlates and consequences of venous thromboembolism: the Iowa Women’s Health Study. Am. J. Public Health 100, 1506–1513 (2010).
Severinsen, M. T. et al. Anthropometry, body fat, and venous thromboembolism: a Danish follow-up study. Circulation 120, 1850–1857 (2009).
Evensen, L. H., Brækkan, S. K. & Hansen, J. B. Regular physical activity and risk of venous thromboembolism. Semin. Thromb. Hemost. 44, 765–779 (2018).
Kunutsor, S. K. et al. Physical activity and risk of venous thromboembolism: systematic review and meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 35, 431–442 (2020).
Centers for Disease Control and Prevention. Strategies to prevent & manage obesity. CDC https://www.cdc.gov/obesity/strategies/index.html (2022).
Mahmoodi, B. K. et al. Association of traditional cardiovascular risk factors with venous thromboembolism: an individual participant data meta-analysis of prospective studies. Circulation 135, 7–16 (2017).
Rosendaal, F. R. Venous thrombosis: a multicausal disease. Lancet 353, 1167–1173 (1999).
Cushman, M. et al. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am. J. Med. 117, 19–25 (2004).
Heit, J. A., Spencer, F. A. & White, R. H. The epidemiology of venous thromboembolism. J. Thromb. Thrombolysis 41, 3–14 (2016).
Ay, C., Pabinger, I. & Cohen, A. T. Cancer-associated venous thromboembolism: burden, mechanisms, and management. Thromb. Haemost. 117, 219–230 (2017).
Albertsen, I. E., Piazza, G. & Goldhaber, S. Z. Let’s stop dichotomizing venous thromboembolism as provoked or unprovoked. Circulation 138, 2591–2593 (2018).
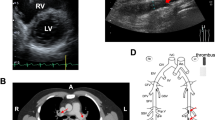
Konstantinides, S. V. et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): the Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur. Respir. J. https://doi.org/10.1183/13993003.01647-2019 (2019).
Ortel, T. L. et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 4, 4693–4738 (2020).
Kearon, C. et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 149, 315–352 (2016).
Hong, J. et al. Incidence of venous thromboembolism in Korea from 2009 to 2013. PLoS ONE 13, e0191897 (2018).
Ceresetto, J. M. Venous thromboembolism in Latin America: a review and guide to diagnosis and treatment for primary care. Clinics 71, 36–46 (2016).
Vázquez, F. J., Posadas-Martínez, M. L., Vicens, J., González Bernaldo de Quirós, F. & Giunta, D. H. Incidence rate of symptomatic venous thromboembolic disease in patients from a medical care program in Buenos Aires, Argentina: a prospective cohort. Thrombosis J. 11, 16 (2013).
Ho, W. K., Hankey, G. J. & Eikelboom, J. W. The incidence of venous thromboembolism: a prospective, community-based study in Perth, Western Australia. Med. J. Aust. 189, 144–147 (2008).
Danwang, C., Temgoua, M. N., Agbor, V. N., Tankeu, A. T. & Noubiap, J. J. Epidemiology of venous thromboembolism in Africa: a systematic review. J. Thromb. Haemost. 15, 1770–1781 (2017).
Virani, S. S. et al. Heart disease and stroke statistics–2021 update: a report from the American Heart Association. Circulation 143, e254–e743 (2021).
Cohen, A. T. et al. Venous thromboembolism (VTE) in Europe. The number of VTE events and associated morbidity and mortality. Thromb. Haemost. 98, 756–764 (2007).
Wiener, R. S., Schwartz, L. M. & Woloshin, S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch. Intern. Med. 171, 831–837 (2011).
den Exter, P. L. et al. Establishing diagnostic criteria and treatment of subsegmental pulmonary embolism: a Delphi analysis of experts. Res. Pract. Thromb. Haemost. 4, 1251–1261 (2020).
Stein, P. D., Matta, F. & Hughes, M. J. Home treatment of deep venous thrombosis according to comorbid conditions. Am. J. Med. 129, 392–397 (2016).
Stein, P. D. et al. Home treatment of pulmonary embolism in the era of novel oral anticoagulants. Am. J. Med. 129, 974–977 (2016).
Klil-Drori, A. J., Coulombe, J., Suissa, S., Hirsch, A. & Tagalakis, V. Temporal trends in outpatient management of incident pulmonary embolism and associated mortality. Thromb. Res. 161, 111–116 (2018).
Gangireddy, C. et al. Risk factors and clinical impact of postoperative symptomatic venous thromboembolism. J. Vasc. Surg. 45, 335–341 (2007).
Hak, D. J. Prevention of venous thromboembolism in trauma and long bone fractures. Curr. Opin. Pulm. Med. 7, 338–343 (2001).
van Stralen, K. J., Rosendaal, F. R. & Doggen, C. J. Minor injuries as a risk factor for venous thrombosis. Arch. Intern. Med. 168, 21–26 (2008).
Heit, J. A. et al. Incidence of venous thromboembolism in hospitalized patients vs community residents. Mayo Clin. Proc. 76, 1102–1110 (2001).
Jordan Bruno, X. et al. Venous thrombosis risk during and after medical and surgical hospitalizations: the Medical Inpatient Thrombosis and Hemostasis (MITH) study. J. Thromb. Haemost. 20, 1645–1652 (2022).
Darzi, A. J. et al. Prognostic factors for VTE and bleeding in hospitalized medical patients: a systematic review and meta-analysis. Blood 135, 1788–1810 (2020).
Darzi, A. J. et al. Risk models for VTE and bleeding in medical inpatients: systematic identification and expert assessment. Blood Adv. 4, 2557–2566 (2020).
Darzi, A. J. et al. Risk-assessment models for VTE and bleeding in hospitalized medical patients: an overview of systematic reviews. Blood Adv. 4, 4929–4944 (2020).
Barnathan, E. S. et al. Increased risk of death in acutely ill medical patients with asymptomatic proximal deep vein thrombosis or symptomatic venous thromboembolism: insights from the Magellan study. Blood 134 (Suppl. 1), 163–163 (2019).
Arepally, G. M. & Cines, D. B. Pathogenesis of heparin-induced thrombocytopenia. Transl. Res. 225, 131–140 (2020).
Cuker, A. & Cines, D. B. How I treat heparin-induced thrombocytopenia. Blood 119, 2209–2218 (2012).
Hogan, M. & Berger, J. S. Heparin-induced thrombocytopenia (HIT): review of incidence, diagnosis, and management. Vasc. Med. 25, 160–173 (2020).
Cowan, L. T., Lutsey, P. L., Pankow, J. S., Cushman, M. & Folsom, A. R. Hospitalization with infection and incident venous thromboembolism: the ARIC study. Thromb. Res. 151, 74–78 (2017).
Bjøri, E., Johnsen, H. S., Hansen, J. B. & Brækkan, S. K. Hospitalization as a trigger for venous thromboembolism–Results from a population-based case-crossover study. Thromb. Res. 176, 115–119 (2019).
Timp, J. F. et al. Antibiotic use as a marker of acute infection and risk of first and recurrent venous thrombosis. Br. J. Haematol. 176, 961–970 (2017).
Nopp, S., Moik, F., Jilma, B., Pabinger, I. & Ay, C. Risk of venous thromboembolism in patients with COVID-19: a systematic review and meta-analysis. Res. Pract. Thromb. Haemost. 4, 1178–1191 (2020).
NIH. Coronavirus disease 2019 (COVID-19): treatment guidelines. COVID-19 Treatment Guidelines https://www.covid19treatmentguidelines.nih.gov/ (2022).
Moores, L. K. et al. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report. Chest 158, 1143–1163 (2020).
Arepally, G. M. & Ortel, T. L. Vaccine-induced immune thrombotic thrombocytopenia: what we know and do not know. Blood 138, 293–298 (2021).
Greinacher, A. et al. Insights in ChAdOx1 nCoV-19 vaccine-induced immune thrombotic thrombocytopenia. Blood 138, 2256–2268 (2021).
Klein, N. P. et al. Surveillance for adverse events after COVID-19 mRNA vaccination. JAMA 326, 1390–1399 (2021).
Tu, T. M. et al. Incidence of cerebral venous thrombosis following SARS-CoV-2 infection vs mRNA SARS-CoV-2 vaccination in singapore. JAMA Netw. Open 5, e222940 (2022).
Houghton, D. E. et al. Risk of venous thromboembolism after COVID-19 vaccination. J. Thromb. Haemost. 20, 1638–1644 (2022).
Olson, N. C. et al. Inflammation markers and incident venous thromboembolism: the reasons for geographic and racial differences in stroke (REGARDS) cohort. J. Thromb. Haemost. 12, 1993–2001 (2014).
Agarwal, V., Phung, O. J., Tongbram, V., Bhardwaj, A. & Coleman, C. I. Statin use and the prevention of venous thromboembolism: a meta-analysis. Int. J. Clin. Pract. 64, 1375–1383 (2010).
Folsom, A. R., Lutsey, P. L., Heckbert, S. R. & Cushman, M. Serum albumin and risk of venous thromboembolism. Thromb. Haemost. 104, 100–104 (2010).
Lindström, S. et al. Genomic and transcriptomic association studies identify 16 novel susceptibility loci for venous thromboembolism. Blood 134, 1645–1657 (2019).
Biedermann, J. S. et al. Rosuvastatin use improves measures of coagulation in patients with venous thrombosis. Eur. Heart J. 39, 1740–1747 (2018).
Glynn, R. J. et al. A randomized trial of rosuvastatin in the prevention of venous thromboembolism. N. Engl. J. Med. 360, 1851–1861 (2009).
Ge, S. Q. et al. Associations of hormonal contraceptives and infertility medications on the risk of venous thromboembolism, ischemic stroke, and cardiovascular disease in women. J. Investig. Med. 67, 729–735 (2019).
Lidegaard, O., Nielsen, L. H., Skovlund, C. W., Skjeldestad, F. E. & Lokkegaard, E. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001-9. BMJ 343, d6423 (2011).
Li, J. et al. Association of risk for venous thromboembolism with use of low-dose extended- and continuous-cycle combined oral contraceptives: a safety study using the sentinel distributed database. JAMA Intern. Med. 178, 1482–1488 (2018).
Kasum, M. et al. Thrombosis following ovarian hyperstimulation syndrome. Gynecol. Endocrinol. 30, 764–768 (2014).
Canonico, M., Plu-Bureau, G., Lowe, G. D. & Scarabin, P. Y. Hormone replacement therapy and risk of venous thromboembolism in postmenopausal women: systematic review and meta-analysis. BMJ 336, 1227–1231 (2008).
Kotamarti, V. S., Greige, N., Heiman, A. J., Patel, A. & Ricci, J. A. Risk for venous thromboembolism in transgender patients undergoing cross-sex hormone treatment: a systematic review. J. Sex. Med. 18, 1280–1291 (2021).
Kourlaba, G., Relakis, J., Kontodimas, S., Holm, M. V. & Maniadakis, N. A systematic review and meta-analysis of the epidemiology and burden of venous thromboembolism among pregnant women. Int. J. Gynaecol. Obstet. 132, 4–10 (2016).
Creanga, A. A., Syverson, C., Seed, K. & Callaghan, W. M. Pregnancy-related mortality in the United States, 2011–2013. Obstet. Gynecol. 130, 366–373 (2017).
Brenner, B. Haemostatic changes in pregnancy. Thromb. Res. 114, 409–414 (2004).
Bazzan, M. & Donvito, V. Low-molecular-weight heparin during pregnancy. Thromb. Res. 101, V175–V186 (2001).
Tepper, N. K. et al. Postpartum venous thromboembolism: incidence and risk factors. Obstet. Gynecol. 123, 987–996 (2014).
Blondon, M. et al. Racial and ethnic differences in the risk of postpartum venous thromboembolism: a population-based, case-control study. J. Thromb. Haemost. 12, 2002–2009 (2014).
Holmegard, H. N., Nordestgaard, B. G., Schnohr, P., Tybjaerg-Hansen, A. & Benn, M. Endogenous sex hormones and risk of venous thromboembolism in women and men. J. Thromb. Haemost. 12, 297–305 (2014).
Roetker, N. S. et al. Prospective study of endogenous hormones and incidence of venous thromboembolism: the atherosclerosis risk in communities study. Thromb. Haemost. 118, 1940–1950 (2018).
Ajayi, A. A., Mathur, R. & Halushka, P. V. Testosterone increases human platelet thromboxane A2 receptor density and aggregation responses. Circulation 91, 2742–2747 (1995).
Fernandez-Balsells, M. M. et al. Clinical review 1: adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 95, 2560–2575 (2010).
Glueck, C. J. & Wang, P. Testosterone therapy, thrombosis, thrombophilia, cardiovascular events. Metabolism 63, 989–994 (2014).
Walker, R. F. et al. Association of testosterone therapy with risk of venous thromboembolism among men with and without hypogonadism. JAMA Intern. Med. 180, 190–197 (2020).
Layton, J. B. et al. Testosterone lab testing and initiation in the United Kingdom and the United States, 2000 to 2011. J. Clin. Endocrinol. Metab. 99, 835–842 (2014).
Baillargeon, J. et al. Risk of venous thromboembolism in men receiving testosterone therapy. Mayo Clin. Proc. 90, 1038–1045 (2015).
FDA. Drug Safety Communication: FDA cautions about using testosterone products for low testosterone due to aging; requires labeling change to inform of possible increased risk of heart attack and stroke with use. FDA https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-cautions-about-using-testosterone-products-low-testosterone-due (2019).
Tan, R. S., Cook, K. R. & Reilly, W. G. Myocardial infarction and stroke risk in young healthy men treated with injectable testosterone. Int. J. Endocrinol. 2015, 970750 (2015).
Vigen, R. et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 310, 1829–1836 (2013).
Naess, I. A. et al. Incidence and mortality of venous thrombosis: a population-based study. J. Thromb. Haemost. 5, 692–699 (2007).
Folsom, A. R. et al. Distributions of hemostatic variables in blacks and whites: population reference values from the Atherosclerosis Risk in Communities (ARIC) study. Ethn. Dis. 2, 35–46 (1992).
Nagashima, J. et al. Influence of physical fitness and smoking on the coagulation system in hypertensive patients: effect on prothrombin fragment F1+2. Intern. Med. 46, 933–936 (2007).
Kannel, W. B. Overview of hemostatic factors involved in atherosclerotic cardiovascular disease. Lipids 40, 1215–1220 (2005).
Becker, R. C. Thrombotic preparedness in aging: a translatable construct for thrombophilias? J. Thromb. Thrombolysis 24, 323–325 (2007).
Moores, L., Bilello, K. L. & Murin, S. Sex and gender issues and venous thromboembolism. Clin. Chest Med. 25, 281–297 (2004).
Pabinger, I. & Grafenhofer, H. Thrombosis during pregnancy: risk factors, diagnosis and treatment. Pathophysiol. Haemost. Thromb. 32, 322–324 (2002).
Robertson, L. & Greer, I. Thromboembolism in pregnancy. Curr. Opin. Obstet. Gynecol. 17, 113–116 (2005).
Wu, O. et al. Oral contraceptives, hormone replacement therapy, thrombophilias and risk of venous thromboembolism: a systematic review. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study. Thromb. Haemost. 94, 17–25 (2005).
Roach, R. E., Cannegieter, S. C. & Lijfering, W. M. Differential risks in men and women for first and recurrent venous thrombosis: the role of genes and environment. J. Thromb. Haemost. 12, 1593–1600 (2014).
Silverstein, M. D. et al. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch. Intern. Med. 158, 585–593 (1998).
Shatzel, J. J., Connelly, K. J. & DeLoughery, T. G. Thrombotic issues in transgender medicine: a review. Am. J. Hematol. 92, 204–208 (2017).
Zakai, N. A. & McClure, L. A. Racial differences in venous thromboembolism. J. Thromb. Haemost. 9, 1877–1882 (2011).
United States Census Bureau. About the topic of race. United States Census Bureau https://www.census.gov/topics/population/race/about.html (2022).
Folsom, A. R. et al. Reasons for differences in the incidence of venous thromboembolism in black versus white Americans. Am. J. Med. 132, 970–976 (2019).
White, R. H., Zhou, H., Murin, S. & Harvey, D. Effect of ethnicity and gender on the incidence of venous thromboembolism in a diverse population in California in 1996. Thromb. Haemost. 93, 298–305 (2005).
Stein, P. D., Kayali, F., Olson, R. E. & Milford, C. E. Pulmonary thromboembolism in Asians/Pacific Islanders in the United States: analysis of data from the National Hospital Discharge Survey and the United States Bureau of the Census. Am. J. Med. 116, 435–442 (2004).
Zakai, N. A. et al. Racial and regional differences in venous thromboembolism in the United States in 3 cohorts. Circulation 129, 1502–1509 (2014).
Martin, K. A. et al. Time trends in pulmonary embolism mortality rates in the United States, 1999 to 2018. J. Am. Heart Assoc. 9, e016784 (2020).
Jørgensen, H. et al. Socioeconomic status and risk of incident venous thromboembolism. J. Thromb. Haemost. 19, 3051–3061 (2021).
Zöller, B., Ohlsson, H., Sundquist, J. & Sundquist, K. Cardiovascular fitness in young males and risk of unprovoked venous thromboembolism in adulthood. Ann. Med. 49, 176–184 (2017).
Kubota, Y., Cushman, M., Zakai, N., Rosamond, W. D. & Folsom, A. R. TV viewing and incident venous thromboembolism: the Atherosclerotic Risk in Communities Study. J. Thrombosis Thrombolysis 45, 353–359 (2018).
Suadicani, P., Hannerz, H., Bach, E. & Gyntelberg, F. Jobs encompassing prolonged sitting in cramped positions and risk of venous thromboembolism: cohort study. JRSM Short. Rep. 3, 8 (2012).
Johannesen, C. D. L. et al. Sedentary work and risk of venous thromboembolism. Scand. J. Work. Env. Health 46, 69–76 (2020).
Folsom, A. R. & Cushman, M. Exploring opportunities for primary prevention of unprovoked venous thromboembolism: ready for prime time? J. Am. Heart Assoc. 9, e019395 (2020).
Lutsey, P. L. Invited commentary: diet and risk of venous thromboembolism–a hard nut to crack. Am. J. Epidemiol. 175, 127–130 (2012). discussion 131-2.
Glynn, R. J., Ridker, P. M., Goldhaber, S. Z., Zee, R. Y. & Buring, J. E. Effects of random allocation to vitamin E supplementation on the occurrence of venous thromboembolism: report from the Women’s Health Study. Circulation 116, 1497–1503 (2007).
Lutsey, P. L., Steffen, L. M., Virnig, B. A. & Folsom, A. R. Diet and incident venous thromboembolism: the Iowa Women’s Health Study. Am. Heart J. 157, 1081–1087 (2009).
Steffen, L. M., Folsom, A. R., Cushman, M., Jacobs, D. R. Jr. & Rosamond, W. D. Greater fish, fruit, and vegetable intakes are related to lower incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology. Circulation 115, 188–195 (2007).
Varraso, R., Kabrhel, C., Goldhaber, S. Z., Rimm, E. B. & Camargo, C. A. Jr Prospective study of diet and venous thromboembolism in US women and men. Am. J. Epidemiol. 175, 114–126 (2012).
Hoevenaar-Blom, M. P. et al. Mediterranean style diet and 12-year incidence of cardiovascular diseases: the EPIC-NL cohort study. PLoS ONE 7, e45458 (2012).
Ohira, T., Iso, H., Yamagishi, K., Tamakoshi, A. & Group, J. S. Fish intake and death from pulmonary embolisms among Japanese men and women–the Japan Collaborative Cohort (JACC) study. Circulation J. 82, 2063–2070 (2018).
Chen, M., Ji, M., Chen, T., Hong, X. & Jia, Y. Alcohol consumption and risk for venous thromboembolism: a meta-analysis of prospective studies. Systematic review. Front. Nutr. 7, 32 (2020).
Tapson, V. F. The role of smoking in coagulation and thromboembolism in chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 2, 71–77 (2005).
Elisia, I. et al. The effect of smoking on chronic inflammation, immune function and blood cell composition. Sci. Rep. 10, 19480 (2020).
Enga, K. F. et al. Cigarette smoking and the risk of venous thromboembolism: the Tromso Study. J. Thromb. Haemost. 10, 2068–2074 (2012).
Lutsey, P. L., Cushman, M., Heckbert, S. R., Tang, W. & Folsom, A. R. Longer legs are associated with greater risk of incident venous thromboembolism independent of total body height. The Longitudinal Study of Thromboembolism Etiology (LITE). Thromb. Haemost. 106, 113–120 (2011).
Glynn, R. J. & Rosner, B. Comparison of risk factors for the competing risks of coronary heart disease, stroke, and venous thromboembolism. Am. J. Epidemiol. 162, 975–982 (2005).
Braekkan, S. K. et al. Body height and risk of venous thromboembolism: the Tromsø Study. Am. J. Epidemiol. 171, 1109–1115 (2010).
Fronek, A., Criqui, M. H., Denenberg, J. & Langer, R. D. Common femoral vein dimensions and hemodynamics including Valsalva response as a function of sex, age, and ethnicity in a population study. J. Vasc. Surg. 33, 1050–1056 (2001).
Kügler, C., Strunk, M. & Rudofsky, G. Venous pressure dynamics of the healthy human leg. Role of muscle activity, joint mobility and anthropometric factors. J. Vasc. Res. 38, 20–29 (2001).
Roetker, N. S. et al. Taller height as a risk factor for venous thromboembolism: a Mendelian randomization meta-analysis. J. Thromb. Haemost. 15, 1334–1343 (2017).
Zöller, B., Ji, J., Sundquist, J. & Sundquist, K. Body height and incident risk of venous thromboembolism: a cosibling design. Circ. Cardiovasc. Genet. https://doi.org/10.1161/circgenetics.116.001651 (2017).
Horvei, L. D., Braekkan, S. K. & Hansen, J. B. Weight change and risk of venous thromboembolism: the Tromso Study. PLoS ONE 11, e0168878 (2016).
French, S. A. et al. Weight change over 9 years and subsequent risk of venous thromboembolism in the ARIC cohort. Int. J. Obes. 44, 2465–2471 (2020).
Klovaite, J., Benn, M. & Nordestgaard, B. G. Obesity as a causal risk factor for deep venous thrombosis: a Mendelian randomization study. J. Intern. Med. 277, 573–584 (2015).
Lindstrom, S. et al. Assessing the causal relationship between obesity and venous thromboembolism through a Mendelian randomization study. Hum. Genet. 136, 897–902 (2017).
Armenta Flores, R., Armenta-Villalobos, D., Ramirez-Centeno, E., Harrison-Ragle, D. & Carrillo, L. G. D. May Thurner syndrome: sixty years later. Phlebology 37, 5–13 (2022).
Harbin, M. M. & Lutsey, P. L. May–Thurner syndrome: history of understanding and need for defining population prevalence. J. Thromb. Haemost. 18, 534–542 (2020).
Klarin, D. et al. Genome-wide association analysis of venous thromboembolism identifies new risk loci and genetic overlap with arterial vascular disease. Nat. Genet. 51, 1574–1579 (2019).
Zoller, B. Genetics of venous thromboembolism revised. Blood 134, 1568–1570 (2019).
Zoller, B., Ohlsson, H., Sundquist, J. & Sundquist, K. Familial risk of venous thromboembolism in first-, second- and third-degree relatives: a nationwide family study in Sweden. Thromb. Haemost. 109, 458–463 (2013).
Hotoleanu, C. In: Thrombosis and Embolism: from Research to Clinical Practice Vol. 1 (ed. Islam, M. S.) 253–272 (Springer, 2017).
Zöller, B. et al. Genetic risk factors for venous thromboembolism. Expert. Rev. Hematol. 13, 971–981 (2020).
Kujovich, J. L. Factor V Leiden thrombophilia. In: GeneReviews. (eds Adam M. P. et al.) (University of Washington, 2018).
Simone, B. et al. Risk of venous thromboembolism associated with single and combined effects of factor V Leiden, prothrombin 20210A and methylenetethraydrofolate reductase C677T: a meta-analysis involving over 11,000 cases and 21,000 controls. Eur. J. Epidemiol. 28, 621–647 (2013).
Morange, P. E., Suchon, P. & Tregouet, D. A. Genetics of venous thrombosis: update in 2015. Thromb. Haemost. 114, 910–919 (2015).
Folsom, A. R. et al. Prospective study of sickle cell trait and venous thromboembolism incidence. J. Thromb. Haemost. 13, 2–9 (2015).
Heller, P., Best, W. R., Nelson, R. B. & Becktel, J. Clinical implications of sickle-cell trait and glucose-6-phosphate dehydrogenase deficiency in hospitalized Black male patients. N. Engl. J. Med. 300, 1001–1005 (1979).
Bucknor, M. D., Goo, J. S. & Coppolino, M. L. The risk of potential thromboembolic, renal and cardiac complications of sickle cell trait. Hemoglobin 38, 28–32 (2014).
Centers for Disease Control and Prevention. Data & statistics on sickle cell disease. CDC https://www.cdc.gov/ncbddd/sicklecell/data.html (2018).
Harrison, S. E., Walcott, C. M. & Warner, T. D. Knowledge and awareness of sickle cell trait among young African American adults. West. J. Nurs. Res. 39, 1222–1239 (2017).
Lim, M. Y., Ataga, K. I. & Key, N. S. Hemostatic abnormalities in sickle cell disease. Curr. Opin. Hematol. 20, 472–477 (2013).
Whelihan, M. F. et al. Thrombin generation and cell-dependent hypercoagulability in sickle cell disease. J. Thromb. Haemost. 14, 1941–1952 (2016).
Klarin, D. et al. Genetic analysis of venous thromboembolism in UK Biobank identifies the ZFPM2 locus and implicates obesity as a causal risk factor. Circ. Cardiovasc. Genet. 10, e001643 (2017).
Folsom, A. R. et al. Replication of a genetic risk score for venous thromboembolism in whites but not in African Americans. J. Thromb. Haemost. 14, 83–88 (2016).
Varki, A. Trousseau’s syndrome: multiple definitions and multiple mechanisms. Blood 110, 1723–1729 (2007).
Young, A. et al. Thrombosis and cancer. Nat. Rev. Clin. Oncol. 9, 437–449 (2012).
Horsted, F., West, J. & Grainge, M. J. Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLoS Med. 9, e1001275 (2012).
Khorana, A. A., Kuderer, N. M., Culakova, E., Lyman, G. H. & Francis, C. W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111, 4902–4907 (2008).
Martens, K. L. et al. HIGH-2-LOW risk model to predict venous thromboembolism in allogeneic transplant patients after platelet engraftment. Blood Adv. 5, 167–175 (2021).
Li, A. et al. Derivation and validation of a risk assessment model for immunomodulatory drug-associated thrombosis among patients with multiple myeloma. J. Natl Compr. Canc Netw. 17, 840–847 (2019).
Douce, D. R. et al. Risk factors for cancer-associated venous thromboembolism: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) study. J. Thromb. Haemost. 17, 2152–2159 (2019).
Lyman, G. H. et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 5, 927–974 (2021).
Chaturvedi, S. et al. Complement activity and complement regulatory gene mutations are associated with thrombosis in APS and CAPS. Blood 135, 239–251 (2020).
Lim, W. Antiphospholipid syndrome. Hematol. Am. Soc. Hematol. Educ. Program. 2013, 675–680 (2013).
Duarte-Garcia, A. et al. The epidemiology of antiphospholipid syndrome: a population-based study. Arthritis Rheumatol. 71, 1545–1552 (2019).
Abdel-Wahab, N. et al. Systematic review of observational studies reporting antiphospholipid antibodies in patients with solid tumors. Blood Adv. 4, 1746–1755 (2020).
Ortel, T. L., Erkan, D. & Kitchens, C. S. How I treat catastrophic thrombotic syndromes. Blood 126, 1285–1293 (2015).
Zöller, B., Li, X., Sundquist, J. & Sundquist, K. Autoimmune diseases and venous thromboembolism: a review of the literature. Am. J. Cardiovasc. Dis. 2, 171–183 (2012).
Zöller, B., Li, X., Sundquist, J. & Sundquist, K. Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden. Lancet 379, 244–249 (2012).
Yusuf, H. R. et al. Risk of venous thromboembolism among hospitalizations of adults with selected autoimmune diseases. J. Thromb. Thrombolysis 38, 306–313 (2014).
Nguyen, G. C. & Sam, J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am. J. Gastroenterol. 103, 2272–2280 (2008).
Romero-Diaz, J., Garcia-Sosa, I. & Sanchez-Guerrero, J. Thrombosis in systemic lupus erythematosus and other autoimmune diseases of recent onset. J. Rheumatol. 36, 68–75 (2009).
Hoisnard, L. et al. Adverse events associated with JAK inhibitors in 126,815 reports from the WHO pharmacovigilance database. Sci. Rep. 12, 7140 (2022).
Folsom, A. R., de Vries, P. S. & Cushman, M. No prospective association of a polygenic risk score for coronary artery disease with venous thromboembolism incidence. J. Thromb. Haemost. 19, 2841–2844 (2021).
Watson, H. G. & Baglin, T. P. Guidelines on travel-related venous thrombosis. Br. J. Haematol. 152, 31–34 (2011).
Ocak, G. et al. Risk of venous thrombosis in patients with chronic kidney disease: identification of high-risk groups. J. Thromb. Haemost. 11, 627–633 (2013).
Mahmoodi, B. K. et al. Association of mild to moderate chronic kidney disease with venous thromboembolism: pooled analysis of five prospective general population cohorts. Circulation 126, 1964–1971 (2012).
Tang, L., Wu, Y. Y., Lip, G. Y., Yin, P. & Hu, Y. Heart failure and risk of venous thromboembolism: a systematic review and meta-analysis. Lancet Haematol. 3, e30–e44 (2016).
Fanola, C. L. et al. Incident heart failure and long-term risk for venous thromboembolism. J. Am. Coll. Cardiol. 75, 148–158 (2020).
Enga, K. F. et al. Atrial fibrillation and future risk of venous thromboembolism: the Tromso study. J. Thromb. Haemost. 13, 10–16 (2015).
Lutsey, P. L. et al. Atrial fibrillation and venous thromboembolism: evidence of bidirectionality in the Atherosclerosis Risk in Communities Study. J. Thromb. Haemost. 16, 670–679 (2018).
Mount, H. R., Rich, M. & Putnam, M. S. Recurrent venous thromboembolism. Am. Fam. Physician 105, 377–385 (2022).
Galanaud, J. P., Monreal, M. & Kahn, S. R. Epidemiology of the post-thrombotic syndrome. Thromb. Res. 164, 100–109 (2018).
Olson, S. R., Shatzel, J. J. & DeLoughery, T. G. Asymptomatic “breakthrough” thrombosis and anticoagulant “failure”: keep calm and carry on. Res. Pract. Thromb. Haemost. 3, 498–502 (2019).
Agnelli, G. et al. Oral apixaban for the treatment of acute venous thromboembolism. N. Engl. J. Med. 369, 799–808 (2013).
Castellucci, L. A. et al. Clinical and safety outcomes associated with treatment of acute venous thromboembolism: a systematic review and meta-analysis. JAMA 312, 1122–1135 (2014).
The Hokusai-VTE Investigators Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N. Engl. J. Med. 369, 1406–1415 (2013).
The EINSTEIN Investigators Oral rivaroxaban for symptomatic venous thromboembolism. N. Engl. J. Med. 363, 2499–2510 (2010).
Prins, M. H. et al. Oral rivaroxaban versus standard therapy for the treatment of symptomatic venous thromboembolism: a pooled analysis of the EINSTEIN-DVT and PE randomized studies. Thromb. J. 11, 21 (2013).
Schulman, S. et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N. Engl. J. Med. 361, 2342–2352 (2009).
Douketis, J. D., Foster, G. A., Crowther, M. A., Prins, M. H. & Ginsberg, J. S. Clinical risk factors and timing of recurrent venous thromboembolism during the initial 3 months of anticoagulant therapy. Arch. Intern. Med. 160, 3431–3436 (2000).
Heit, J. A. The epidemiology of venous thromboembolism in the community. Arterioscler. Thromb. Vasc. Biol. 28, 370–372 (2008).
Prandoni, P. et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica 92, 199–205 (2007).
Heit, J. A. et al. Heparin and warfarin anticoagulation intensity as predictors of recurrence after deep vein thrombosis or pulmonary embolism: a population-based cohort study. Blood 118, 4992–4999 (2011).
Heit, J. A. et al. Predictors of survival after deep vein thrombosis and pulmonary embolism: a population-based, cohort study. Arch. Intern. Med. 159, 445–453 (1999).
RIETE Registry. Death within 30 days. RIETE Registry https://rieteregistry.com/graphics-interactives/dead-30-days/ (2022).
Minges, K. E., Bikdeli, B., Wang, Y., Attaran, R. R. & Krumholz, H. M. National and regional trends in deep vein thrombosis hospitalization rates, discharge disposition, and outcomes for Medicare beneficiaries. Am. J. Med. 131, 1200–1208 (2018).
Minges, K. E. et al. National trends in pulmonary embolism hospitalization rates and outcomes for adults aged ≥65 years in the United States (1999 to 2010). Am. J. Cardiol. 116, 1436–1442 (2015).
Tagalakis, V., Patenaude, V., Kahn, S. R. & Suissa, S. Incidence of and mortality from venous thromboembolism in a real-world population: the Q-VTE Study Cohort. Am. J. Med. 126, 832 e13-21 (2013).
Flinterman, L. E., van Hylckama Vlieg, A., Cannegieter, S. C. & Rosendaal, F. R. Long-term survival in a large cohort of patients with venous thrombosis: incidence and predictors. PLoS Med. 9, e1001155 (2012).
Kalayci, A. et al. Asymptomatic deep vein thrombosis is associated with an increased risk of death: insights from the APEX trial. Thromb. Haemost. 118, 2046–2052 (2018).
Spencer, F. A. et al. Venous thromboembolism and bleeding in a community setting. The Worcester Venous Thromboembolism study. Thromb. Haemost. 101, 878–885 (2009).
MacLehose, R. F. et al. Impact of oral anticoagulant choice for the secondary prevention of venous thromboembolism on the risk of inpatient bleeding. Res. Pract. Thromb. Haemost. 5, e12514 (2021).
Gomez-Outes, A., Terleira-Fernandez, A. I., Lecumberri, R., Suarez-Gea, M. L. & Vargas-Castrillon, E. Direct oral anticoagulants in the treatment of acute venous thromboembolism: a systematic review and meta-analysis. Thromb. Res. 134, 774–782 (2014).
van Es, N., Coppens, M., Schulman, S., Middeldorp, S. & Buller, H. R. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood 124, 1968–1975 (2014).
van der Hulle, T. et al. Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and meta-analysis. J. Thromb. Haemost. 12, 320–328 (2014).
Lutsey, P. L. et al. Risk of hospitalised bleeding in comparisons of oral anticoagulant options for the primary treatment of venous thromboembolism. Br. J. Haematol. 185, 903–911 (2019).
Khan SR, Mathes BM. Post-thrombotic (postphlebitic) syndrome. UpToDate https://www.uptodate.com/contents/post-thrombotic-postphlebitic-syndrome (2022).
Mohr, D. N. et al. The venous stasis syndrome after deep venous thrombosis or pulmonary embolism: a population-based study. Mayo Clin. Proc. 75, 1249–1256 (2000).
Nishimoto, Y. et al. Risk factors for post-thrombotic syndrome in patients with deep vein thrombosis: from the COMMAND VTE registry. Heart Vessel. 34, 669–677 (2019).
Dronkers, C. E. A. et al. Predicting post-thrombotic syndrome with ultrasonographic follow-up after deep vein thrombosis: a systematic review and meta-analysis. Thromb. Haemost. 118, 1428–1438 (2018).
Kahn, S. R., Galanaud, J. P., Vedantham, S. & Ginsberg, J. S. Guidance for the prevention and treatment of the post-thrombotic syndrome. J. Thromb. Thrombolysis 41, 144–153 (2016).
Gall, H. et al. The Giessen Pulmonary Hypertension Registry: survival in pulmonary hypertension subgroups. J. Heart Lung Transpl. 36, 957–967 (2017).
Galie, N. et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Respir. J. 46, 903–975 (2015).
Martinez, C., Wallenhorst, C., Teal, S., Cohen, A. T. & Peacock, A. J. Incidence and risk factors of chronic thromboembolic pulmonary hypertension following venous thromboembolism, a population-based cohort study in England. Pulm. Circ. 8, 2045894018791358 (2018).
Ende-Verhaar, Y. M. et al. Incidence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism: a contemporary view of the published literature. Eur. Respir. J. https://doi.org/10.1183/13993003.01792-2016 (2017).
Lutsey, P. L. et al. Incidence and risk factors of pulmonary hypertension after venous thromboembolism: an analysis of a large health care database. J. Am. Heart Assoc. 11, e024358 (2022).
Klok, F. A. et al. The post-PE syndrome: a new concept for chronic complications of pulmonary embolism. Blood Rev. 28, 221–226 (2014).
Braekkan, S. K. et al. Venous thromboembolism and subsequent permanent work-related disability. J. Thromb. Haemost. 14, 1978–1987 (2016).
Stefanick, M. L. et al. The relationship of cardiovascular disease to physical functioning in women surviving to age 80 and above in the Women’s Health Initiative. J. Gerontol. A Biol. Sci. Med. Sci. 71 (Suppl. 1), 42–53 (2016).
Lutsey, P. L. et al. Long-term association of venous thromboembolism with frailty, physical functioning, and quality of life: the Atherosclerosis Risk in Communities Study. J. Am. Heart Assoc. 9, e015656 (2020).
Lloyd-Jones, D. M. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613 (2010).
Vaduganathan, M., Venkataramani, A. S. & Bhatt, D. L. Moving toward global primordial prevention in cardiovascular disease: the heart of the matter. J. Am. Coll. Cardiol. 66, 1535–1537 (2015).
Claas, S. A. & Arnett, D. K. The role of healthy lifestyle in the primordial prevention of cardiovascular disease. Curr. Cardiol. Rep. 18, 56 (2016).
Yuan, S. et al. Overall and abdominal obesity in relation to venous thromboembolism. J. Thromb. Haemost. 19, 460–469 (2021).
James, S. A. Primordial prevention of cardiovascular disease among African-Americans: a social epidemiological perspective. Prev. Med. 29, S84–S89 (1999).
Evans, C. R. et al. Lifestyle moderates genetic risk of venous thromboembolism: the ARIC study. Arterioscler. Thromb. Vasc. Biol. 40, 2756–2763 (2020).
Office of the Surgeon General (US); National Heart, Lung, and Blood Institute. Surgeon General’s Call to Action to Prevent Deep Vein Thrombosis and Pulmonary Embolism (Office of the Surgeon General (US), 2008).
The Joint Commision. Specifications Manual for National Hospital Inpatient Quality Measures V5.6. The Joint Commission https://www.jointcommission.org/-/media/tjc/documents/measurement/specification-manuals/hiqr_specsman_july2019_v5_6.pdf (2019).
Schunemann, H. J. et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2, 3198–3225 (2018).
Maynard, G. Preventing hospital-associated venous thromboembolism: a guide for effective quality improvement (Agency for Healthcare Research and Quality, 2016).
Key, N. S. et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 38, 496–520 (2020).
Cushman, M. & Creager, M. A. Improving awareness and outcomes related to venous thromboembolism. JAMA 314, 1913–1914 (2015).
Wendelboe, A. M. et al. Global public awareness of venous thromboembolism. J. Thromb. Haemost. 13, 1365–1371 (2015).
Aggarwal, A. et al. Deep vein thrombosis (DVT) and pulmonary embolism (PE): awareness and prophylaxis practices reported by patients with cancer. Cancer Invest 33, 405–410 (2015).
Zöller, B., Li, X., Sundquist, J. & Sundquist, K. Socioeconomic and occupational risk factors for venous thromboembolism in Sweden: a nationwide epidemiological study. Thromb. Res. 129, 577–582 (2012).
White, R. H., Dager, W. E., Zhou, H. & Murin, S. Racial and gender differences in the incidence of recurrent venous thromboembolism. Thromb. Haemost. 96, 267–273 (2006).
Lau, B. D. et al. Eliminating health care disparities with mandatory clinical decision support: the venous thromboembolism (VTE) example. Med. Care 53, 18–24 (2015).
Aujesky, D. et al. Predictors of early hospital readmission after acute pulmonary embolism. Arch. Intern. Med. 169, 287–293 (2009).
Aujesky, D., Long, J. A., Fine, M. J. & Ibrahim, S. A. African American race was associated with an increased risk of complications following venous thromboembolism. J. Clin. Epidemiol. 60, 410–416 (2007).
Acknowledgements
We graciously acknowledge A. Folsom (University of Minnesota, USA) and M. Cushman (University of Vermont, USA) for serving as our mentors and introducing us as we began our careers in VTE epidemiology. P.L.L. is supported by the NIH National Heart, Lung, and Blood Institute award K24 HL159246.
Author information
Authors and Affiliations
Contributions
Both authors contributed substantially to all aspect of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Suzanne Cannegieter and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Review criteria
We provide a broad overview of the epidemiology and prevention of venous thromboembolism (VTE). Given the breadth of this topic, including an exhaustive review of the literature for each risk factor and VTE was not possible. Therefore, we tried to identify either a well-performed meta-analysis or a few representative studies for each risk factor. In general, we placed the most weight on randomized controlled trials (when available), followed by large, population-based, cohort studies, and then case–control studies or other designs. With regard to VTE anatomical sites, we focus on the deep veins of the legs and arms as well as of the pulmonary arterial vasculature. Alternative sites of thrombosis, such as cerebral sinus thrombosis and splanchnic vein thrombosis, are not reviewed in this article because, although having some shared risk factors, they are managed differently and often have very specific risk factors. Additionally, treatment is reviewed more extensively in various consensus statements, and a full review of treatment strategies is outside the scope of this Review.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lutsey, P.L., Zakai, N.A. Epidemiology and prevention of venous thromboembolism. Nat Rev Cardiol 20, 248–262 (2023). https://doi.org/10.1038/s41569-022-00787-6
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-022-00787-6
This article is cited by
-
GP6 polymorphisms and venous thromboembolism: a Chinese case-control study with cross-population assessment
BMC Cardiovascular Disorders (2026)
-
Triglyceride-glucose body mass index and risk of incident venous thromboembolism: a prospective cohort study from the UK Biobank
European Journal of Medical Research (2026)
-
Extended reduced versus full-dose treatment with factor Xa inhibitors in patients with venous thromboembolism: a GRADE-assessed systematic review and meta-analysis of randomized controlled trials
Naunyn-Schmiedeberg's Archives of Pharmacology (2026)
-
Antithrombotic Function of Dahuang Zhechong Pill and Its Active Ingredients: A Review
Chinese Journal of Integrative Medicine (2026)
-
Exploration of the causal relationship and mechanisms between serum albumin and venous thrombosis: a bidirectional mendelian randomization analysis and bioinformatics study
Thrombosis Journal (2025)