Abstract
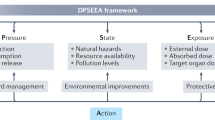
Cardiovascular disease is the leading cause of morbidity and mortality worldwide, with a substantial amount of health-care resources targeted towards its diagnosis and management. Environmental sustainability in cardiovascular care can have an important role in reducing greenhouse gas emissions and pollution and could be beneficial for improving health metrics and societal well-being and minimizing the cost of health care. In this Review, we discuss the motivations and frameworks for sustainable cardiovascular care with an emphasis on the reduction of the climate-related and environmental effects of cardiovascular care. We also provide an overview of greenhouse gas emissions related to the provision of health care, including their measurement and quantification, carbon accounting, carbon disclosures and climate effects. The principles of life-cycle assessment, waste prevention and circular economics in health care are discussed, and the emissions associated with various sectors of cardiovascular care as well as the rationale for prevention as a powerful approach to reduce these emissions are presented. Finally, we highlight the challenges in environmental sustainability and future directions as applicable to cardiovascular practice.
Key points
-
Cardiovascular health and environmental health are interlinked; sustainable cardiovascular care is crucial for reducing emissions and pollution while improving outcomes.
-
Cardiovascular care has a large environmental footprint owing to high energy use and waste from devices and procedures; this footprint needs further quantification.
-
Strategies such as energy efficiency, renewable energy, waste reduction, disease prevention, innovation and circular economy principles can reduce carbon emissions and costs.
-
Lack of transparency and regulatory levers hampers current sustainability efforts, but frameworks for disclosures, target setting and reporting emissions are emerging.
-
Health-care leaders should measure emissions, set reduction targets, redesign care and engage stakeholders to transition towards sustainable models that improve value, outcomes and planetary health.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Change history
16 May 2025
In the version of the article initially published, the Acknowledgements section was missing and has now been added to the HTML and PDF versions of the article.
References
Rajagopalan, S. & Landrigan, P. J. Pollution and the heart. N. Engl. J. Med. 385, 1881–1892 (2021).
Romanello, M. et al. The 2023 report of the Lancet Countdown on health and climate change: the imperative for a health-centred response in a world facing irreversible harms. Lancet 402, 2346–2394 (2023).
Lenzen, M. et al. The environmental footprint of health care: a global assessment. Lancet Planet. Health 4, e271–e279 (2020).
Rajagopalan, S., Pronovost, P. & Al-Kindi, S. Implementing a sustainability framework in healthcare: a three-lens framework. Healthcare 11, 1867 (2023).
Dzau, V. J., Levine, R., Barrett, G. & Witty, A. Decarbonizing the U.S. health sector — a call to action. N. Engl. J. Med. 385, 2117–2119 (2021).
Whitmee, S. et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation–Lancet Commission on planetary health. Lancet 386, 1973–2028 (2015).
Myers, S. S. Planetary health: protecting human health on a rapidly changing planet. Lancet 390, 2860–2868 (2017).
Swinburn, B. A. et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 393, 791–846 (2019).
Marina, R. et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet 400, 1619–1654 (2022).
United Nations. Sustainability. UN https://www.un.org/en/academic-impact/sustainability.
Purvis, B., Mao, Y. & Robinson, D. Three pillars of sustainability: in search of conceptual origins. Sustain. Sci. 14, 681–695 (2018).
Adams, G., Entwistle, D., Hochman, R. & Lassiter, W. III. Opinion: embracing sustainability makes good business sense. Modern Healthcare https://www.modernhealthcare.com/opinion/opinion-embracing-sustainability-makes-good-business-sense-greg-adams-rod-hochman-wright-lassiter? (2023).
Yadav, M., Aneja, R. & Ahmed, W. Do clean energy transition, environment degradation, and energy efficiency influence health expenditure: empirical evidence from emerging countries. J. Clean. Prod. 428, 139355 (2023).
Ani, V. A. Powering primary healthcare centres with clean energy sources. Renew. Energy Environ. Sustain. 6, 7 (2021).
George, D. R. & Ethridge, A. E. Hospital-based community gardens as a strategic partner in addressing community health needs. Am. J. Public Health 113, 939–942 (2023).
Khan, M. R. Polluter-pays-principle: the cardinal instrument for addressing climate change. Laws 4, 638–653 (2015).
Rabin, A. S. & Pinsky, E. G. Reducing health care’s climate impact — mission critical or extra credit? N. Engl. J. Med. 389, 583–585 (2023).
Pichler, P.-P., Jaccard, I. S., Weisz, U. & Weisz, H. International comparison of health care carbon footprints. Environ. Res. Lett. https://doi.org/10.1088/1748-9326/ab19e1 (2019).
Eckelman, M. J. et al. Health care pollution and public health damage in the United States: an update. Health Aff. 39, 2071–2079 (2020).
Tennison, I. et al. Health care’s response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet. Health 5, e84–e92 (2021).
The World Bank. Current health expenditure (% of GDP). World Bank https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?most_recent_value_desc=true (2024).
Eckelman, M. J. & Sherman, J. D. Estimated global disease burden from us health care sector greenhouse gas emissions. Am. J. Public Health 108, S120–S122 (2018).
Eckelman, M. J. & Sherman, J. Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE 11, e0157014 (2016).
SduHealth. Reducing the use of natural resources in health and social care, 2018 report. SduHealth https://www.sduhealth.org.uk/documents/Policy (2018).
United Nations Framework Convention for Climate Change. Background. UNFCCC https://unfccc.int/ (accessed 10 July 2024).
Matthews, H. S., Hendrickson, C. T. & Matthews, D. Life Cycle Assessment: Quantitative Approaches for Decisions that Matter, 2014 (LCA Textbook, 2019).
McAlister, S., Morton, R. L. & Barratt, A. Incorporating carbon into health care: adding carbon emissions to health technology assessments. Lancet Planet. Health 6, e993–e999 (2022).
US Environmental Protection Agency. US environmentally-extended input–output (USEEIO) models. EPA https://www.epa.gov/land-research/us-environmentally-extended-input-output-useeio-models (2023).
Senay, E., Cort, T., Perkison, W., Laestadius, J. G. & Sherman, J. D. What can hospitals learn from the Coca-Cola company? Health care sustainability reporting. NEJM Catal. Innov. Care Deliv. https://doi.org/10.1056/cat.21.0362 (2022).
Senay, E. & Landrigan, P. J. Assessment of environmental sustainability and corporate social responsibility reporting by large health care organizations. JAMA Netw. Open 1, e180975 (2018).
Health Care Without Harm. Climate and health resources. Health Care Without Harm https://healthcareclimateaction.org/resources (2023).
National Academy of Medicine. Action collaborative on decarbonizing the U.S. health sector. NAM https://nam.edu/programs/climate-change-and-human-health/action-collaborative-on-decarbonizing-the-u-s-health-sector/ (2024).
American Hospitals Association. Sustainability roadmap for healthcare. AHA https://www.aha.org/sustainability (2023).
Science Based Targets. Foundations of science-based target setting. Version 1.0 April 2019. Science Based Targets https://sciencebasedtargets.org/resources/files/foundations-of-SBT-setting.pdf (2019).
TNFD. The Taskforce on nature-related financial disclosures (TNFD). TNFD https://tnfd.global/ (accessed 14 December 2023).
Health and Human Services. Health sector commitments to emissions reduction and resilience. HHS https://www.hhs.gov/climate-change-health-equity-environmental-justice/climate-change-health-equity/actions/health-sector-pledge/index.html (accessed 25 February 2024).
The Joint Commission. Sustainable healthcare certification. The Joint Commission https://www.jointcommission.org/what-we-offer/certification/certifications-by-setting/hospital-certifications/sustainable-healthcare-certification/ (accessed 24 February 2024).
World Health Organization. Global spending on health: rising to the pandemic’s challenges. WHO https://www.who.int/publications/i/item/9789240064911 (2023).
CMS. United States national health expenditure data. CMS https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/historical (accessed 22 December 2023).
Birger, M. et al. Spending on cardiovascular disease and cardiovascular risk factors in the United States: 1996 to 2016. Circulation 144, 271–282 (2021).
Szirt, R. et al. Environmental sustainability in the cardiac catheter laboratory. Heart Lung Circ. 32, 11–15 (2023).
Ahmed, B. Reducing cath lab’s carbon footprint: is it time, and can it be done? J. Soc. Cardiovasc. Angiogr. Interv. 1, 100371 (2022).
Doshi, H. et al. Potentially recyclable material during cardiac catheterizations and coronary interventions: curbing the carbon footprint in the cath lab. J. Am. Coll. Cardiol. 81, 2333 (2023).
Reed, G. W., Tushman, M. L. & Kapadia, S. R. Operational efficiency and effective management in the catheterization laboratory: JACC review topic of the week. J. Am. Coll. Cardiol. 72, 2507–2517 (2018).
Farrelly, J. S. et al. Surgical tray optimization as a simple means to decrease perioperative costs. J. Surg. Res. 220, 320–326 (2017).
Kapoor, A. et al. Guidance on reuse of cardio-vascular catheters and devices in India: a consensus document. Indian Heart J. 69, 357–363 (2017).
Mansour, M. et al. The impact of first procedure success rate on the economics of atrial fibrillation ablation. JACC Clin. Electrophysiol. 3, 129–138 (2017).
Mond, H. G. & Proclemer, A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009 — a World Society of Arrhythmia’s project. Pacing Clin. Electrophysiol. 34, 1013–1027 (2011).
Ditac, G. et al. Carbon footprint of atrial fibrillation catheter ablation. Europace 25, 331–340 (2023).
Perez Diaz, P. et al. Carbon footprint as a marker of environmental impact in patients included in a remote monitoring pacemaker programme. Eur. Heart J. 42, ehab724.0409 (2021).
Bawa, D. et al. Impact of remote cardiac monitoring on greenhouse gas emissions. JACC Adv. 2, 100286 (2023).
Boussuge-Roze, J. et al. Current practices and expectations to reduce environmental impact of electrophysiology catheters: results from an EHRA/LIRYC European physician survey. Europace 24, 1300–1306 (2022).
Schulte, A., Maga, D. & Thonemann, N. Combining life cycle assessment and circularity assessment to analyze environmental impacts of the medical remanufacturing of electrophysiology catheters. Sustainability 13, 898 (2021).
Sacher, F. et al. Position paper on sustainability in cardiac pacing and electrophysiology from the Working Group of Cardiac Pacing and Electrophysiology of the French Society of Cardiology. Arch. Cardiovasc. Dis. 117, 224–231 (2024).
McGain, F., Muret, J., Lawson, C. & Sherman, J. D. Environmental sustainability in anaesthesia and critical care. Br. J. Anaesth. 125, 680–692 (2020).
McGain, F., McAlister, S., McGavin, A. & Story, D. The financial and environmental costs of reusable and single-use plastic anaesthetic drug trays. Anaesth. Intensive Care 38, 538–544 (2010).
Overcash, M. A comparison of reusable and disposable perioperative textiles: sustainability state-of-the-art 2012. Anesth. Analg. 114, 1055–1066 (2012).
MacNeill, A. J., Lillywhite, R. & Brown, C. J. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet. Health 1, e381–e388 (2017).
Grinberg, D. et al. Eco-audit of conventional heart surgery procedures. Eur. J. Cardiothorac. Surg. 60, 1325–1331 (2021).
McGain, F. et al. The carbon footprint of treating patients with septic shock in the intensive care unit. Crit. Care Resusc. 20, 304–312 (2018).
Wormer, B. A. et al. The green operating room: simple changes to reduce cost and our carbon footprint. Am. Surg. 79, 666–671 (2013).
Rizan, C. et al. The carbon footprint of surgical operations: a systematic review. Ann. Surg. 272, 986–995 (2020).
Thiel, C. L., Woods, N. C. & Bilec, M. M. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am. J. Public Health 108, S158–S164 (2018).
Malik, A., Lenzen, M., McAlister, S. & McGain, F. The carbon footprint of Australian health care. Lancet Planet. Health 2, e27–e35 (2018).
Kouropoulos, G. P. A predictive model for the estimation of carbon dioxide emissions of magnetic resonance imaging (MRI) units and computed tomography (CT) scanners. J. Urban Environ. Eng. 12, 172–187 (2018).
Ciampi, Q. et al. Reshaping of Italian echocardiographic laboratories activities during the second wave of COVID-19 pandemic and expectations for the post-pandemic era. J. Clin. Med. 10, 3466 (2021).
Marwick, T. H. & Buonocore, J. Environmental impact of cardiac imaging tests for the diagnosis of coronary artery disease. Heart 97, 1128–1131 (2011).
McAlister, S. et al. The carbon footprint of hospital diagnostic imaging in Australia. Lancet Reg. Health West. Pac. 24, 100459 (2022).
Brünjes, R. & Hofmann, T. Anthropogenic gadolinium in freshwater and drinking water systems. Water Res. 182, 115966 (2020).
De Paula Marteleto, T. & Enzweiler, J. Anthropogenic gadolinium as a tracer of raw sewage in surface water. Environ. Earth Sci. 80, 607 (2021).
Dekker, H. M., Stroomberg, G. J. & Prokop, M. Tackling the increasing contamination of the water supply by iodinated contrast media. Insights Imaging 13, 30 (2022).
PubChem. Compound summary: sulfur hexafluoride. NCBI https://pubchem.ncbi.nlm.nih.gov/compound/17358 (2024).
PubChem. Compound summary: perflutren. NCBI https://pubchem.ncbi.nlm.nih.gov/compound/Perflutren (2024).
Nasir, K. & Khan, S. U. Power of zero as gatekeeper for stable chest pain patients: minimizing losses and maximizing gains. J. Am. Coll. Cardiol. 80, 1978–1980 (2022).
Dacones, I., Cave, C., Furie, G. L., Ogden, C. A. & Slutzman, J. E. Patient transport greenhouse gas emissions from outpatient care at an integrated health care system in the Northwestern United States, 2015–2020. J. Clim. Change Health 3, 100024 (2021).
Goetz, C., Rotman, S. R., Hartoularos, G. & Bishop, T. F. The effect of charge display on cost of care and physician practice behaviors: a systematic review. J. Gen. Intern. Med. 30, 835–842 (2015).
Bhopal, A. & Norheim, O. F. Fair pathways to net-zero healthcare. Nat. Med. 29, 1078–1084 (2023).
Kaplan, S., Sadler, B., Little, K., Franz, C. & Orris, P. Can sustainable hospitals help bend the health care cost curve? Issue Brief (Commonw. Fund) 29, 1–14 (2012).
Hall, K. D., Guo, J., Dore, M. & Chow, C. C. The progressive increase of food waste in America and its environmental impact. PLoS ONE 4, e7940 (2009).
Practice Greenhealth. Food waste: making the case. Practice Greenhealth https://practicegreenhealth.org/topics/food/food-waste-making-case (2023).
Williams, P. & Walton, K. Plate waste in hospitals and strategies for change. e-SPEN 6, e235–e241 (2011).
Cook, N., Goodwin, D., Porter, J. & Collins, J. Food and food‐related waste management strategies in hospital food services: a systematic review. Nutr. Dietetics 80, 116–142 (2023).
American Medical Association. Healthy food options in hospitals. AMA https://policysearch.ama-assn.org/policyfinder/detail/Healthy%20Food%20Options%20in%20Hospitals%20H-150.949?uri=%2FAMADoc%2FHOD.xml-0-627.xml (2023).
WHO European Office for the Prevention and Control of Noncommunicable Diseases. Plant-based diets and their impact on health, sustainability and the environment: a review of the evidence. WHO https://www.who.int/europe/publications/i/item/WHO-EURO-2021-4007-43766-61591 (2021).
Willett, W. et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 393, 447–492 (2019).
Zhong, J., Bourges-Sevenier, B., Francesco, P. & Rajagopalan, S. Planting a seed for sustainable hospital menus. Eur. Heart J. 45, 152–153 (2024).
Batool, T., Neven, A., Vanrompay, Y., Adnan, M. & Dendale, P. There is a silver lining: carbon footprint reduction by holding Preventive Cardiology conference 2020 virtually. Eur. J. Prev. Cardiol. 28, zwab061.224 (2021).
Health care, circular economy principles and sustainable well being. Sustainable Healthcare Coalition https://shcoalition.org/healthcare-circular-economy-principles-and-sustainable-wellbeing/ (accessed 18 December 2023).
Landrigan, P. J. et al. The Minderoo–Monaco commission on plastics and human health. Ann. Glob. Health 89, 23 (2023).
US Environmental Protection Agency. National overview: facts and figures on materials, wastes and recycling. EPA https://www.epa.gov/facts-and-figures-about-materials-waste-and-recycling/national-overview-facts-and-figures-materials (2022).
Ellen MacArthur Foundation. Circular economy of cities. City governments and their role in enabling a circular economy transition. Ellen MacArthur Foundation http://www.ellenmacarthurfoundation.org/our-work/activities/circular-economy-in-cities (2019).
Lucertini, G. & Musco, F. Circular urban metabolism framework. One Earth 2, 138–142 (2020).
Frugal innovation: why low cost doesn’t have to mean low impact. Nature 624, 8 (2023).
Brown, C., Bhatti, Y. & Harris, M. Environmental sustainability in healthcare systems: role of frugal innovation. BMJ 383, e076381 (2023).
Ellen MacArthur Foundation. The big food redesign. Regenerating nature with the circular economy. Ellen MacArthur Foundation https://emf.thirdlight.com/file/24/ycO8Ejgyc.pr_Qnyc9Zryd4xjP/The%20big%20food%20redesign%20study.pdf (2021).
Ellen MacArthur Foundation and ARUP. City governments and their role in enabling a circular economy transition: an overview of urban policy levers. Ellen MacArthur Foundation https://emf.thirdlight.com/link/lg3ap956qxbi-66omej/@/#id=0 (2019).
Global road map for health care decarbonization. A navigational tool for achieving zero emissions with climate resilience and health equity. Health Care Climate Action healthcareclimateaction.org/roadmap (2021).
Sinn, H.-W. The Green Paradox: A Supply-Side Approach to Global Warming (MIT Press, 2012).
Delmas, M. A. & Colgan, D. The Green Bundle: Pairing the Market with the Planet (Stanford Univ. Press, 2018).
Repenning, N. & Sterman, J. Capability traps and self-confirming attribution errors in the dynamics of process improvment. Admin. Sci. Q. https://doi.org/10.2307/3094806 (2002).
Repenning, N. & Sterman, J. Nobody ever gets credit for fixing problems that never happened: creating and sustaining process improvement. Calif. Manag. Rev. 43, 64–88 (2021).
US Environmental Protection Agency. The benefits and costs of the Clean Air Act from 1990 to 2020, final report, Rev A. EPA https://www.epa.gov/sites/production/files/2015-07/documents/fullreport_rev_a.pdf (2011).
Drabo, E. F. et al. A social-return-on-investment analysis of bon secours hospital’s ‘housing for health’ affordable housing program. Health Aff. 40, 513–520 (2021).
Shafquat, A. et al. Reprocessing cardiac electrophysiology catheters: recommendations of pak hrs task force and review of literature. Pak. Heart J. 55, 213–217 (2022).
Mkoko, P., Barole, N., Solomon, K. & Chin, A. Feasibility and safety of interventional electrophysiology and catheter ablation in the South African public sector: challenges and opportunities for comprehensive cardiac electrophysiology in South Africa. J. Arrhythm. 38, 1042–1048 (2022).
Browne, K. F., Maldonado, R., Telatnik, M., Vlietstra, R. E. & Brenner, A. S. Initial experience with reuse of coronary angioplasty catheters in the United States. J. Am. Coll. Cardiol. 30, 1735–1740 (1997).
Selvaraj, R. J. et al. Reuse of pacemakers, defibrillators and cardiac resynchronisation devices. Heart Asia 9, 30–33 (2017).
Sinha, S. K. et al. Worldwide pacemaker and defibrillator reuse: systematic review and meta-analysis of contemporary trials. Pacing Clin. Electrophysiol. 41, 1500–1507 (2018).
Marchese, D. This pioneering economist says our obsession with growth must end. The New York Times (17 July 2022).
Aronson, J. et al. The road to sustainability must bridge three great divides. Ann. N. Y. Acad. Sci. 1185, 225–236 (2010).
Mitić, P., Fedajev, A., Radulescu, M. & Rehman, A. The relationship between CO2 emissions, economic growth, available energy, and employment in SEE countries. Environ. Sci. Pollut. Res. 30, 16140–16155 (2023).
Rajagopalan, S. & Landrigan, P. J. The inflation reduction act — implications for climate change, air pollution, and health. Lancet Reg. Health Am. 23, 100522 (2023).
European Commission. The European green deal: striving to be the first climate-neutral continent. European Commission https://commission.europa.eu/strategy-and-policy/priorities-2019-2024/european-green-deal_en (2024).
IPCC. Fourth assessment report. IPCC https://www.ipcc.ch/assessment-report/ar4/ (2007).
IPCC. Fifth assessment report. IPCC https://www.ipcc.ch/assessment-report/ar5/ (2014).
Devlin-Hegedus, J. A., McGain, F., Harris, R. D. & Sherman, J. D. Action guidance for addressing pollution from inhalational anaesthetics. Anaesthesia 77, 1023–1029 (2022).
Acknowledgements
Work in the laboratory of A.B. was supported in part by NIH Grant #P42 ES023716.
Author information
Authors and Affiliations
Contributions
S.R. and S.A.-K. researched data for the article. S.R., S.M., R.D.P., R.D.B., K.N., M.J.N., P.L. and S.A.-K. substantially contributed to the discussion of content. S.R. and S.A.-K. wrote the article. All authors reviewed/edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
C.V.S. is a salaried employee of Mazzetti. J.R.C. is a salaried employee of Eaton Corporation. K.H.B. is a salaried employee of the American Society for Health Care Engineering of the American Hospital Association. The views represented here are solely those of the authors and do not necessarily reflect the views of the authors’ employers. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Francis Bessiere and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rajagopalan, S., McAlister, S., Jay, J. et al. Environmental sustainability in cardiovascular practice: current challenges and future directions. Nat Rev Cardiol 22, 241–254 (2025). https://doi.org/10.1038/s41569-024-01077-z
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41569-024-01077-z
This article is cited by
-
Planetary Health: At the Crossroads of CVD Prevention
Current Cardiology Reports (2025)
-
A Body Shape Index as a Simple Anthropometric Marker for the Risk of Cardiovascular Events
Current Cardiology Reports (2025)
-
Climate conscious pharmacy practice: a qualitative interview study with pharmacists in the context of respiratory health care
International Journal of Clinical Pharmacy (2025)