Abstract
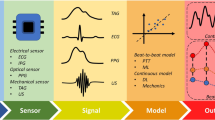
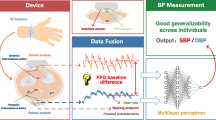
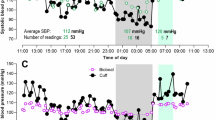
With advances in materials science and medical technology, wearable sensors have become crucial tools for the early diagnosis and continuous monitoring of numerous cardiovascular diseases, including arrhythmias, hypertension and coronary artery disease. These devices employ various sensing mechanisms, such as mechanoelectric, optoelectronic, ultrasonic and electrophysiological methods, to measure vital biosignals, including pulse rate, blood pressure and changes in heart rhythm. In this Review, we provide a comprehensive overview of the current state of wearable cardiovascular sensors, focusing particularly on those that measure blood pressure. We explore biosignal sensing principles, discuss blood pressure estimation methods (including machine learning algorithms) and summarize the latest advances in cuffless wearable blood pressure sensors. Finally, we highlight the challenges of and offer insights into potential pathways for the practical application of cuffless wearable blood pressure sensors in the medical field from both technical and clinical perspectives.
Key points
-
Wearable blood pressure (BP) sensors utilize diverse sensing methodologies, including mechanoelectric, optoelectronic, ultrasonic and electrophysiologic technologies, that facilitate continuous cardiovascular monitoring.
-
Various approaches, including pulse wave analysis, pulse wave velocity and arterial wall dynamics, as well as advanced machine learning and deep learning algorithms that build on these methods, are being explored to improve the accuracy of BP estimation in wearable cuffless BP sensors.
-
Cuffless BP sensors still face obstacles in achieving clinical-grade reliability due to issues with sensor calibration, motion artefacts and placement accuracy.
-
Further improvements in sensor materials and system integration are crucial for improving the accuracy and clinical applicability of wearable BP sensors.
-
Comprehensive clinical trials are essential to validate the performance of wearable BP sensors and ensure compliance with established medical standards for broader adoption in health-care settings.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Change history
04 July 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41569-025-01189-0
References
Lewington, S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Jones, D. W., Appel, L. J., Sheps, S. G., Roccella, E. J. & Lenfant, C. Measuring blood pressure accurately: new and persistent challenges. JAMA 289, 1027–1030 (2003).
Malik, R. et al. Relationship between blood pressure and incident cardiovascular disease: linear and nonlinear Mendelian randomization analyses. Hypertension 77, 2004–2013 (2021).
Fuchs, F. D. & Whelton, P. K. High blood pressure and cardiovascular disease. Hypertension 75, 285–292 (2020).
Wu, C. Y. et al. High blood pressure and all-cause and cardiovascular disease mortalities in community-dwelling older adults. Medicine 94, e2160 (2015).
Perera, Y., Raitt, J., Poole, K., Metcalfe, D. & Lewinsohn, A. Non-invasive versus arterial pressure monitoring in the pre-hospital critical care environment: a paired comparison of concurrently recorded measurements. Scand. J. Trauma. Resusc. Emerg. Med. 32, 77 (2024).
Bowdle, T. A. Complications of invasive monitoring. Anesthesiol. Clin. North. Am. 20, 333–350 (2002).
Quan, X. et al. Advances in non‐invasive blood pressure monitoring. Sensors 21, 4373 (2021).
Sladen, A. Complications of invasive hemodynamic monitoring in the intensive care unit. Curr. Probl. Surg. 25, 75–145 (1988).
Ramasamy, S. & Balan, A. Wearable sensors for ECG measurement: a review. Sens. Rev. 38, 412–419 (2018).
Yoo, J., Yan, L., Lee, S., Kim, H. & Yoo, H. J. A wearable ECG acquisition system with compact planar-fashionable circuit board-based shirt. IEEE Trans. Inf. Technol. Biomed. 13, 897–902 (2009).
Lyu, Q., Gong, S., Yin, J., Dyson, J. M. & Cheng, W. Soft wearable healthcare materials and devices. Adv. Healthc. Mater. 10, e2100577 (2021).
Shrivastava, S., Trung, T. Q. & Lee, N. E. Recent progress, challenges, and prospects of fully integrated mobile and wearable point-of-care testing systems for self-testing. Chem. Soc. Rev. 49, 1812–1866 (2020).
James, G. D. & Gerber, L. M. Measuring arterial blood pressure in humans: auscultatory and automatic measurement techniques for human biological field studies. Am. J. Hum. Biol. https://doi.org/10.1002/ajhb.23063 (2018).
Kario, K. Sleep and nocturnal hypertension: genes, environment, and individual profiles. J. Clin. Hypertens. 24, 1263–1265 (2022).
Tomitani, N., Hoshide, S. & Kario, K. Accurate nighttime blood pressure monitoring with less sleep disturbance. Hypertens. Res. 44, 1671–1673 (2021).
Kario, K. Nocturnal hypertension new technology and evidence. Hypertension 71, 997–1009 (2018).
Lou, M. et al. Highly wearable, breathable, and washable sensing textile for human motion and pulse monitoring. ACS Appl. Mater. Interfaces 12, 19965–19973 (2020).
Kang, X. et al. A wearable and real-time pulse wave monitoring system based on a flexible compound sensor. Biosensors 12, 133 (2022).
Huang, Y. et al. Arteriosclerosis assessment based on single-point fingertip pulse monitoring using a wearable iontronic sensor. Adv. Healthc. Mater. 12, e2301838 (2023).
Wang, J. et al. Wearable multichannel pulse condition monitoring system based on flexible pressure sensor arrays. Microsyst. Nanoeng. 8, 16 (2022).
Su, Y. et al. Muscle fibers inspired high-performance piezoelectric textiles for wearable physiological monitoring. Adv. Funct. Mater. 31, 2010962 (2021).
Kim, K. et al. Highly sensitive and wearable liquid metal-based pressure sensor for health monitoring applications: integration of a 3D-printed microbump array with the microchannel. Adv. Healthc. Mater. 9, e2000313 (2019).
Castaneda, D., Esparza, A., Ghamari, M., Soltanpur, C. & Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 4, 195–202 (2018).
Shaltis, P. A., Reisner, A. & Asada, H. H. Wearable, cuff-less PPG-based blood pressure monitor with novel height sensor. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2006, 908–911 (2006).
Davies, H. J., Williams, I., Peters, N. S. & Mandic, D. P. In-ear SpO2: a tool for wearable, unobtrusive monitoring of core blood oxygen saturation. Sensors 20, 4879 (2020).
Joo, M. G. et al. Reflection-boosted wearable ring-type pulse oximeters for SpO2 measurement with high sensitivity and low power consumption. Biosensors 13, 711 (2023).
Rodriguez-Labra, J. I., Kosik, C., Maddipatla, D., Narakathu, B. B. & Atashbar, M. Z. Development of a PPG sensor array as a wearable device for monitoring cardiovascular metrics. IEEE Sens. J. 21, 26320–26327 (2021).
Steinberg, S., Huang, A., Ono, Y. & Rajan, S. Continuous artery monitoring using a flexible and wearable single-element ultrasonic sensor. IEEE Instrum. Meas. Mag. 25, 6–11 (2022).
Huang, A., Yoshida, M., Ono, Y. & Rajan, S. Continuous measurement of arterial diameter using wearable and flexible ultrasonic sensor. 2017 IEEE Int. Ultrason. Symp. (IUS) 1–4 (IEEE, 2017).
Peng, C., Chen, M., Sim, H. K., Zhu, Y. & Jiang, X. Noninvasive and nonocclusive blood pressure monitoring via a flexible piezo-composite ultrasonic sensor. IEEE Sens. J. 21, 2642–2650 (2021).
Almohimeed, I., Agarwal, M. & Ono, Y. Wearable ultrasonic sensor using double-layer PVDF films for monitoring tissue motion. Can. Conf. Electr. Comput. Eng. https://doi.org/10.1109/CCECE.2018.8447859 (2018).
Yin, L. et al. Chest-scale self-compensated epidermal electronics for standard 6-precordial-lead ECG. NPJ Flex. Electron. 6, 29 (2022).
Zhang, S. et al. On-skin ultrathin and stretchable multifunctional sensor for smart healthcare wearables. NPJ Flex. Electron. 6, 11 (2022).
Han, N. et al. Recent progress of biomaterials-based epidermal electronics for healthcare monitoring and human–machine interaction. Biosensors 13, 393 (2023).
Park, C., Chou, P. H., Bai, Y., Matthews, R. & Hibbs, A. An ultra-wearable, wireless, low power ECG monitoring system. Proceedings of the 2006 IEEE Biomedical Circuits and Systems Conference pp 241–244 (IEEE, 2006).
Zhou, Z. B. et al. Wearable continuous blood pressure monitoring devices based on pulse wave transit time and pulse arrival time: a review. Materials 16, 2133 (2023).
Konstantinidis, D. et al. Wearable blood pressure measurement devices and new approaches in hypertension management: the digital era. J. Hum. Hypertens. 36, 945–951 (2022).
Islam, S. M. S. et al. Wearable cuffless blood pressure monitoring devices: a systematic review and meta-analysis. Eur. Hear. J. Digit. Heal. 3, 323–337 (2022).
Mukkamala, R. et al. Evaluation of the accuracy of cuffless blood pressure measurement devices: challenges and proposals. Hypertension 78, 1161–1167 (2021).
Xu, H. et al. A high-sensitivity near-infrared phototransistor based on an organic bulk heterojunction. Nanoscale 5, 11850–11855 (2013).
He, J. et al. A universal high accuracy wearable pulse monitoring system via high sensitivity and large linearity graphene pressure sensor. Nano Energy 59, 422–433 (2019).
Kang, S. et al. Highly sensitive pressure sensor based on bioinspired porous structure for real-time tactile sensing. Adv. Electron. Mater. https://doi.org/10.1002/aelm.201670065 (2016).
Li, X. et al. Ultracomfortable hierarchical nanonetwork for highly sensitive pressure sensor. ACS Nano 14, 9605–9612 (2020).
Jian, M. et al. Flexible and highly sensitive pressure sensors based on bionic hierarchical structures. Adv. Funct. Mater. https://doi.org/10.1002/adfm.201606066 (2017).
Barton, C. et al. Evaluation of a machine learning algorithm for up to 48-hour advance prediction of sepsis using six vital signs. Comput. Biol. Med. 109, 79–84 (2019).
Gultepe, E. et al. From vital signs to clinical outcomes for patients with sepsis: a machine learning basis for a clinical decision support system. J. Am. Med. Inform. Assoc. 21, 315–325 (2014).
Babu, A., Ranpariya, S., Sinha, D. K., Chatterjee, A. & Mandal, D. Deep learning enabled early predicting cardiovascular status using highly sensitive piezoelectric sensor of solution-processable nylon-11. Adv. Mater. Technol. 8, 2202021 (2023).
Slapni, Č., Ar, G., Mlakar, N. & Luštrek, M. Blood pressure estimation from photoplethysmogram using a spectro-temporal deep neural network. Sensors (Switzerland) 19, 3420 (2019).
Fang, Y. et al. Ambulatory cardiovascular monitoring via a machine-learning-assisted textile triboelectric sensor. Adv. Mater. 33, e2104178 (2021).
El-Hajj, C. & Kyriacou, P. A. A review of machine learning techniques in photoplethysmography for the non-invasive cuff-less measurement of blood pressure. Biomed. Signal. Process. Control. 58, 101870 (2020).
Homayounfar, S. Z. & Andrew, T. L. Wearable sensors for monitoring human motion: a review on mechanisms, materials, and challenges. SLAS Technol. 25, 9–24 (2020).
Park, D. Y. et al. Self‐powered real‐time arterial pulse monitoring using ultrathin epidermal piezoelectric sensors. Adv. Mater. https://doi.org/10.1002/adma.201702308 (2017).
Tian, Y., Hu, C., Peng, D. & Zhu, Z. Self-powered intelligent pulse sensor based on triboelectric nanogenerators with AI assistance. Front. Bioeng. Biotechnol. 11, 1236292 (2023).
Zhang, F. et al. A highly accurate flexible sensor system for human blood pressure and heart rate monitoring based on graphene/sponge. RSC Adv. 12, 2391–2398 (2022).
Mishra, R. B., El-Atab, N., Hussain, A. M. & Hussain, M. M. Recent progress on flexible capacitive pressure sensors: from design and materials to applications. Adv. Mater. Technol. 6, 2001023 (2021).
Sun, Q. et al. Active matrix electronic skin strain sensor based on piezopotential-powered graphene transistors. Adv. Mater. 27, 3411–3417 (2015).
Dagdeviren, C. et al. Conformable amplified lead zirconate titanate sensors with enhanced piezoelectric response for cutaneous pressure monitoring. Nat. Commun. 5, 4496 (2014).
Chu, Y. et al. Human pulse diagnosis for medical assessments using a wearable piezoelectret sensing system. Adv. Funct. Mater. 28, 1803413 (2018).
Tamura, T., Maeda, Y., Sekine, M. & Yoshida, M. Wearable photoplethysmographic sensors – past and present. Electron 3, 282–302 (2014).
Hu, H. et al. Stretchable ultrasonic transducer arrays for three-dimensional imaging on complex surfaces. Sci. Adv. 4, eaar3979 (2018).
Meziane, N., Webster, J. G., Attari, M. & Nimunkar, A. J. Dry electrodes for electrocardiography. Physiol. Meas. 34, R47–R69 (2013).
Donelan, J. M. et al. Biomechanical energy harvesting: generating electricity during walking with minimal user effort. Science 319, 807–810 (2008).
Damjanovic, D. Ferroelectric, dielectric and piezoelectric properties of ferroelectric thin films and ceramics. Rep. Prog. Phys. 61, 1267–1324 (1998).
Fu, H. & Cohen, R. E. Polarization rotation mechanism for ultrahigh electromechanical response. Nature 403, 281–283 (2000).
Tressler, J. F., Alkoy, S. & Newnham, R. E. Piezoelectric sensors and sensor materials. J. Electroceram. 2, 257–272 (1998).
Wan, C. & Bowen, C. R. Multiscale-structuring of polyvinylidene fluoride for energy harvesting: the impact of molecular-, micro- and macro-structure. J. Mater. Chem. A 5, 3091–3128 (2017).
Park, K. II et al. Highly-efficient, flexible piezoelectric PZT thin film nanogenerator on plastic substrates. Adv. Mater. 26, 2514–2520 (2014).
Kabra, H., Deore, H. A. & Patil, P. Review on advanced piezoelectric materials (BaTiO3, PZT). JETIR 6, 950–957 (2019).
Kim, M., Doh, I., Oh, E. & Cho, Y. H. Flexible piezoelectric pressure sensors fabricated from nanocomposites with enhanced dispersion and vapor permeability for precision pulse wave monitoring. ACS Appl. Nano Mater. 6, 22025–22035 (2023).
Chun, K. Y., Seo, S. & Han, C. S. A wearable all-gel multimodal cutaneous sensor enabling simultaneous single-site monitoring of cardiac-related biophysical signals. Adv. Mater. 34, e2110082 (2022).
Yang, T. et al. Hierarchically structured PVDF/ZnO core-shell nanofibers for self-powered physiological monitoring electronics. Nano Energy 72, 104706 (2020).
Tian, G. et al. Hierarchical piezoelectric composites for noninvasive continuous cardiovascular monitoring. Adv. Mater. 36, 2313612 (2024).
Xiao, X., Chen, G., Libanori, A. & Chen, J. Wearable triboelectric nanogenerators for therapeutics. Trends Chem. 3, 279–290 (2021).
Wang, Z. L., Chen, J. & Lin, L. Progress in triboelectric nanogenerators as a new energy technology and self-powered sensors. Energy Environ. Sci. 8, 2250–2282 (2015).
Wang, H. S. et al. Performance-enhanced triboelectric nanogenerator enabled by wafer-scale nanogrates of multistep pattern downscaling. Nano Energy 35, 415–423 (2017).
Lee, B. Y., Kim, S. U., Kang, S. & Lee, S. D. Transparent and flexible high power triboelectric nanogenerator with metallic nanowire-embedded tribonegative conducting polymer. Nano Energy 53, 152–159 (2018).
Jeong, C. K. et al. Topographically-designed triboelectric nanogenerator via block copolymer self-assembly. Nano Lett. 14, 7031–7038 (2014).
Kim, D. et al. Direct-laser-patterned friction layer for the output enhancement of a triboelectric nanogenerator. Nano Energy 35, 379–386 (2017).
Meng, K. et al. Kirigami-inspired pressure sensors for wearable dynamic cardiovascular monitoring. Adv. Mater. 34, e2202478 (2022).
Park, H. W. et al. Electron blocking layer-based interfacial design for highly-enhanced triboelectric nanogenerators. Nano Energy 50, 9–15 (2018).
Chai, B. et al. Conductive interlayer modulated ferroelectric nanocomposites for high performance triboelectric nanogenerator. Nano Energy 91, 106668 (2022).
Kim, D. W., Lee, J. H., You, I., Kim, J. K. & Jeong, U. Adding a stretchable deep-trap interlayer for high-performance stretchable triboelectric nanogenerators. Nano Energy 50, 192–200 (2018).
Yu, Y. & Wang, X. Chemical modification of polymer surfaces for advanced triboelectric nanogenerator development. Extrem. Mech. Lett. 9, 514–530 (2016).
Chen, G., Au, C. & Chen, J. Textile triboelectric nanogenerators for wearable pulse wave monitoring. Trends Biotechnol. 39, 1078–1092 (2021).
Dong, K. et al. A stretchable yarn embedded triboelectric nanogenerator as electronic skin for biomechanical energy harvesting and multifunctional pressure sensing. Adv. Mater. 30, e1804944 (2018).
Lin, Z. et al. Triboelectric nanogenerator enabled body sensor network for self-powered human heart-rate monitoring. ACS Nano 11, 8830–8837 (2017).
Ouyang, H. et al. Self-powered pulse sensor for antidiastole of cardiovascular disease. Adv. Mater. 29, 1703456 (2017).
Fan, W. et al. Machine-knitted washable sensor array textile for precise epidermal physiological signal monitoring. Sci. Adv. 6, eaay2840 (2020).
Yue, Y. et al. 3D hybrid porous Mxene-sponge network and its application in piezoresistive sensor. Nano Energy 50, 79–87 (2018).
Fiorillo, A. S., Critello, C. D. & Pullano, A. S. Theory, technology and applications of piezoresistive sensors: a review. Sens. Actuat. A Phys. 281, 156–175 (2018).
Choong, C. L. et al. Highly stretchable resistive pressure sensors using a conductive elastomeric composite on a micropyramid array. Adv. Mater. 26, 3451–3458 (2014).
Fang, X. et al. High‐performance MXene‐based flexible and wearable pressure sensor based on a micro‐pyramid structured active layer. Adv. Mater. Technol. 8, 2200291 (2023).
Pang, C. et al. A flexible and highly sensitive strain-gauge sensor using reversible interlocking of nanofibres. Nat. Mater. 11, 795–801 (2012).
Pan, L. et al. An ultra-sensitive resistive pressure sensor based on hollow-sphere microstructure induced elasticity in conducting polymer film. Nat. Commun. 5, 3002 (2014).
Bijender, N. et al. Noninvasive blood pressure monitoring via a flexible and wearable piezoresistive sensor. ACS Omega 9, 6355–6365 (2024).
Yao, H. et al. A flexible and highly pressure‐sensitive graphene–polyurethane sponge based on fractured microstructure design. Adv. Mater. 25, 6692–6698 (2013).
Liu, C. et al. High-performance piezoresistive flexible pressure sensor based on wrinkled microstructures prepared from discarded vinyl records and ultra-thin, transparent polyaniline films for human health monitoring. J. Mater. Chem. C. 10, 13064–13073 (2022).
Luo, R. et al. Fragmented graphene aerogel/polydimethylsiloxane sponges for wearable piezoresistive pressure sensors. ACS Appl. Nano Mater. 6, 7065–7076 (2023).
Xu, H. et al. Flexible waterproof piezoresistive pressure sensors with wide linear working range based on conductive fabrics. Nanomicro Lett. 12, 159 (2020).
Zheng, Y. et al. Conductive MXene/cotton fabric based pressure sensor with both high sensitivity and wide sensing range for human motion detection and E-skin. Chem. Eng. J. 420, 127720 (2021).
Ding, X. et al. Highly accurate wearable piezoresistive sensors without tension disturbance based on weaved conductive yarn. ACS Appl. Mater. Interfaces 12, 35638–35646 (2020).
Yang, X., Wang, Y. & Qing, X. A flexible capacitive pressure sensor based on ionic liquid. Sensors 18, 2395 (2018).
Zhang, Z. et al. Highly sensitive capacitive pressure sensor based on a micropyramid array for health and motion monitoring. Adv. Electron. Mater. 7, 2100174 (2021).
Yang, J. C. et al. Microstructured porous pyramid-based ultrahigh sensitive pressure sensor insensitive to strain and temperature. ACS Appl. Mater. Interfaces 11, 19472–19480 (2019).
Ruth, S. R. A. et al. Rational design of capacitive pressure sensors based on pyramidal microstructures for specialized monitoring of biosignals. Adv. Funct. Mater. 30, 1903100 (2020).
Ruth, S. R. A., Feig, V. R., Tran, H. & Bao, Z. Microengineering pressure sensor active layers for improved performance. Adv. Funct. Mater. 30, 2003491 (2020).
Kim, J. O. et al. Highly ordered 3D microstructure-based electronic skin capable of differentiating pressure, temperature, and proximity. ACS Appl. Mater. Interfaces 11, 1503–1511 (2019).
Wei, P., Guo, X., Qiu, X. & Yu, D. Flexible capacitive pressure sensor with sensitivity and linear measuring range enhanced based on porous composite of carbon conductive paste and polydimethylsiloxane. Nanotechnology 30, 455501 (2019).
Wang, S. et al. High sensitivity capacitive flexible pressure sensor based on PDMS double wrinkled microstructure. J. Mater. Sci. Mater. Electron. 35, 78 (2024).
Joo, Y. et al. Silver nanowire-embedded PDMS with a multiscale structure for a highly sensitive and robust flexible pressure sensor. Nanoscale 7, 6208–6215 (2015).
Bisri, S. Z., Shimizu, S., Nakano, M. & Iwasa, Y. Endeavor of iontronics: from fundamentals to applications of ion‐controlled electronics. Adv. Mater. https://doi.org/10.1002/adma.201607054 (2017).
Liu, Q. et al. Highly transparent and flexible iontronic pressure sensors based on an opaque to transparent transition. Adv. Sci. https://doi.org/10.1002/advs.202000348 (2020).
Bai, N. et al. Graded intrafillable architecture-based iontronic pressure sensor with ultra-broad-range high sensitivity. Nat. Commun. 11, 209 (2020).
Lee, G. H. et al. Multifunctional materials for implantable and wearable photonic healthcare devices. Nat. Rev. Mater. 5, 149–165 (2020).
Kim, K. B. & Baek, H. J. Photoplethysmography in wearable devices: a comprehensive review of technological advances, current challenges, and future directions. Electronics 12, 2923 (2023).
Tamura, T. Current progress of photoplethysmography and SPO2 for health monitoring. Biomed. Eng. Lett. 9, 21–36 (2019).
Lee, I. et al. Systematic review on human skin-compatible wearable photoplethysmography sensors. Appl. Sci. 11, 2313 (2021).
Lee, H. et al. Toward all-day wearable health monitoring: an ultralow-power, reflective organic pulse oximetry sensing patch. Sci. Adv. 4, eaas9530 (2018).
Khan, Y. et al. A flexible organic reflectance oximeter array. Proc. Natl Acad. Sci. USA 115, E11015–E11024 (2018).
Lochner, C. M., Khan, Y., Pierre, A. & Arias, A. C. All-organic optoelectronic sensor for pulse oximetry. Nat. Commun. 5, 5745 (2014).
Yokota, T. et al. Ultraflexible organic photonic skin. Sci. Adv. 2, e1501856 (2016).
Han, D. et al. Flexible blade-coated multicolor polymer light-emitting diodes for optoelectronic sensors. Adv. Mater. 29, 1606206 (2017).
Jinno, H. et al. Self-powered ultraflexible photonic skin for continuous bio-signal detection via air-operation-stable polymer light-emitting diodes. Nat. Commun. 12, 2234 (2021).
Xu, H. et al. Flexible organic/inorganic hybrid near‐infrared photoplethysmogram sensor for cardiovascular monitoring. Adv. Mater. https://doi.org/10.1002/adma.201700975 (2017).
Bent, B., Goldstein, B. A., Kibbe, W. A. & Dunn, J. P. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit. Med. 3, 18 (2020).
Maeda, Y., Sekine, M. & Tamura, T. Relationship between measurement site and motion artifacts in wearable reflected photoplethysmography. J. Med. Syst. 35, 969–976 (2011).
D’Orazio, J., Jarrett, S., Amaro-Ortiz, A. & Scott, T. UV radiation and the skin. Int. J. Mol. Sci. 14, 12222–12248 (2013).
Boonya-ananta, T. et al. Synthetic photoplethysmography (PPG) of the radial artery through parallelized Monte Carlo and its correlation to body mass index (BMI). Sci. Rep. 11, 2570 (2021).
Kim, J., Lee, T., Kim, J. & Ko, H. Ambient light cancellation in photoplethysmogram application using alternating sampling and charge redistribution technique. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2015, 6441–6444 (2015).
Allen, J., Frame, J. R. & Murray, A. Microvascular blood flow and skin temperature changes in the fingers following a deep inspiratory gasp. Physiol. Meas. 23, 365–373 (2002).
Chong, J. W. et al. Photoplethysmograph signal reconstruction based on a novel hybrid motion artifact detection–reduction approach. Part I: motion and noise artifact detection. Ann. Biomed. Eng. 42, 2238–2250 (2014).
Charlton, P. H. et al. An assessment of algorithms to estimate respiratory rate from the electrocardiogram and photoplethysmogram. Physiol. Meas. 37, 610–626 (2016).
Franklin, D. et al. Synchronized wearables for the detection of haemodynamic states via electrocardiography and multispectral photoplethysmography. Nat. Biomed. Eng. 7, 1229–1241 (2023).
Khan, E., Al Hossain, F., Uddin, S. Z., Alam, S. K. & Hasan, M. K. A robust heart rate monitoring scheme using photoplethysmographic signals corrupted by intense motion artifacts. IEEE Trans. Biomed. Eng. 63, 550–562 (2016).
Lee, H., Chung, H., Kim, J. W. & Lee, J. Motion artifact identification and removal from wearable reflectance photoplethysmography using piezoelectric transducer. IEEE Sens. J. 19, 3861–3870 (2019).
Wang, C. et al. Continuous monitoring of deep-tissue haemodynamics with stretchable ultrasonic phased arrays. Nat. Biomed. Eng. 5, 749–758 (2021).
Pang, D. C. & Chang, C. M. Development of a novel transparent flexible capacitive micromachined ultrasonic transducer. Sensors 17, 1443 (2017).
Kruizinga, P. et al. Compressive 3D ultrasound imaging using a single sensor. Sci. Adv. 3, e170143 (2017).
Lin, M., Hu, H., Zhou, S. & Xu, S. Soft wearable devices for deep-tissue sensing. Nat. Rev. Mater. 7, 850–869 (2022).
Wang, C. C. et al. Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Nat. Biomed. Eng. 2, 687–695 (2018).
Lin, M. et al. A fully integrated wearable ultrasound system to monitor deep tissues in moving subjects. Nat. Biotechnol. 42, 448–457 (2024).
Hu, H. et al. A wearable cardiac ultrasound imager. Nature 613, 667–675 (2023).
Sempionatto, J. R. et al. An epidermal patch for the simultaneous monitoring of haemodynamic and metabolic biomarkers. Nat. Biomed. Eng. 5, 737–748 (2021).
Hu, H. et al. Stretchable ultrasonic arrays for the three-dimensional mapping of the modulus of deep tissue. Nat. Biomed. Eng. 7, 1321–1334 (2023).
Gao, X. et al. A photoacoustic patch for three-dimensional imaging of hemoglobin and core temperature. Nat. Commun. 13, 7757 (2022).
Padala, S. K., Cabrera, J. A. & Ellenbogen, K. A. Anatomy of the cardiac conduction system. Pacing Clin. Electrophysiol. 44, 15–25 (2021).
Becker, D. E. Fundamentals of electrocardiography interpretation. Anesth. Prog. 53, 53–64 (2006).
Veeraraghavan, R., Gourdie, R. G. & Poelzing, S. Mechanisms of cardiac conduction: a history of revisions. Am. J. Physiol. Heart Circ. Physiol. 306, H619–H627 (2014).
Martis, R. J., Acharya, U. R. & Adeli, H. Current methods in electrocardiogram characterization. Comput. Biol. Med. 48, 133–149 (2014).
Homsy, J. & Podrid, P. J. in MGH Cardiology Board Review (eds Gaggin, H. & Januzzi, J., Jr.) 580–622 (Springer, 2014).
AlGhatrif, M. & Lindsay, J. A brief review: history to understand fundamentals of electrocardiography. J. Community Hosp. Intern. Med. Perspect. 2, 14383 (2012).
Lujan, M. R., Perez-Pozuelo, I. & Grandner, M. A. Past, present, and future of multisensory wearable technology to monitor sleep and circadian rhythms. Front. Digit. Heal. 3, 721919 (2021).
Searle, A. & Kirkup, L. A direct comparison of wet, dry and insulating bioelectric recording electrodes. Physiol. Meas. 21, 271–283 (2000).
Lim, C. et al. Tissue-like skin-device interface for wearable bioelectronics by using ultrasoft, mass-permeable, and low-impedance hydrogels. Sci. Adv. 7, eabd6716 (2021).
Ha, M., Lim, S. & Ko, H. Wearable and flexible sensors for user-interactive health-monitoring devices. J. Mater. Chem. B 6, 4043–4064 (2018).
Gao, W., Ota, H., Kiriya, D., Takei, K. & Javey, A. Flexible electronics toward wearable sensing. Acc. Chem. Res. 52, 523–533 (2019).
Ling, Y. et al. Disruptive, soft, wearable sensors. Adv. Mater. 32, e1904664 (2020).
Ma, Z. et al. Permeable superelastic liquid-metal fibre mat enables biocompatible and monolithic stretchable electronics. Nat. Mater. 20, 859–868 (2021).
Son, D. et al. An integrated self-healable electronic skin system fabricated via dynamic reconstruction of a nanostructured conducting network. Nat. Nanotechnol. 13, 1057–1065 (2018).
Zhang, L. et al. Fully organic compliant dry electrodes self-adhesive to skin for long-term motion-robust epidermal biopotential monitoring. Nat. Commun. 11, 4683 (2020).
Chen, X. et al. Fabric-substrated capacitive biopotential sensors enhanced by dielectric nanoparticles. Nano Res. 14, 3248–3252 (2021).
Jeong, J. W. et al. Capacitive epidermal electronics for electrically safe, long-term electrophysiological measurements. Adv. Healthc. Mater. 3, 642–648 (2014).
Liu, J., Hahn, J. O. & Mukkamala, R. Error mechanisms of the oscillometric fixed-ratio blood pressure measurement method. Ann. Biomed. Eng. 41, 587–597 (2013).
Colquhoun, D., Dunn, L. K., McMurry, T. & Thiele, R. H. The relationship between the area of peripherally-derived pressure volume loops and systemic vascular resistance. J. Clin. Monit. Comput. 27, 689–696 (2013).
Kwon, H. M. et al. Estimation of stroke volume variance from arterial blood pressure: using a 1-D convolutional neural network. Sensors 21, 5130 (2021).
Solà, J. & Delgado-Gonzalo, R. The Handbook of Cuffless Blood Pressure Monitoring: A Guide for Clinicians, Researchers, and Engineers (Springer, 2019).
Wołos, K. et al. Non-invasive assessment of stroke volume and cardiovascular parameters based on peripheral pressure waveform. PLoS Comput. Biol. 20, e1012013 (2024).
Kim, J. et al. Soft wearable pressure sensors for beat-to-beat blood pressure monitoring. Adv. Healthc. Mater. 8, e1900109 (2019).
Li, S. et al. Monitoring blood pressure and cardiac function without positioning via a deep learning–assisted strain sensor array. Sci. Adv. 9, eadh0615 (2023).
Yi, Z. et al. Piezoelectric dynamics of arterial pulse for wearable continuous blood pressure monitoring. Adv. Mater. 34, e2110291 (2022).
Yao, Y. et al. Estimation of central pulse wave velocity from radial pulse wave analysis. Comput. Methods Prog. Biomed. 219, 106781 (2022).
Mishra, B. & Thakkar, N. Cuffless blood pressure monitoring using PTT and PWV methods. Proceedings of the 2017 International Conference on Recent Innovations in Signal Processing and Embedded Systems pp 395–401 (IEEE, 2017).
Ma, Y. et al. Relation between blood pressure and pulse wave velocity for human arteries. Proc. Natl Acad. Sci. USA 115, 11144–11149 (2018).
Chung, H. U. et al. Skin-interfaced biosensors for advanced wireless physiological monitoring in neonatal and pediatric intensive-care units. Nat. Med. 26, 418–429 (2020).
Liu, C. et al. Wireless, skin‐interfaced devices for pediatric critical care: application to continuous, noninvasive blood pressure monitoring. Adv. Healthc. Mater. 10, e2100383 (2021).
Yoon, Y. Z. et al. Cuff-less blood pressure estimation using pulse waveform analysis and pulse arrival time. IEEE J. Biomed. Heal. Inform. 22, 1068–1074 (2018).
Zhang, G., Gao, M., Xu, D., Olvier, N. B. & Mukkamala, R. Pulse arrival time is not an adequate surrogate for pulse transit time as a marker of blood pressure. J. Appl. Physiol. 111, 1681–1686 (2011).
Carek, A. M., Conant, J., Joshi, A., Kang, H. & Inan, O. T. SeismoWatch: wearable cuffless blood pressure monitoring using pulse transit time. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 1, 40 (2017).
Li, H. et al. Wearable skin-like optoelectronic systems with suppression of motion artifacts for cuff-less continuous blood pressure monitor. Natl. Sci. Rev. 7, 849–862 (2020).
Meng, K. et al. Flexible weaving constructed self‐powered pressure sensor enabling continuous diagnosis of cardiovascular disease and measurement of cuffless blood pressure. Adv. Funct. Mater. 29, 1806388 (2019).
Proença, J., Muehlsteff, J., Aubert, X. & Carvalho, P. Is pulse transit time a good indicator of blood pressure changes during short physical exercise in a young population? Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2010, 598–601 (2010).
Elgendi, M. et al. The use of photoplethysmography for assessing hypertension. NPJ Digit. Med. 2, 60 (2019).
Baier, D., Teren, A., Wirkner, K., Loeffler, M. & Scholz, M. Parameters of pulse wave velocity: determinants and reference values assessed in the population-based study LIFE-Adult. Clin. Res. Cardiol. 107, 1050–1061 (2018).
Pereira, T., Correia, C. & Cardoso, J. Novel methods for pulse wave velocity measurement. J. Med. Biol. Eng. 35, 555–565 (2015).
Gao, S. C., Wittek, P., Zhao, L. & Jiang, W. J. Data-driven estimation of blood pressure using photoplethysmographic signals. Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society pp 766–769 (IEEE, 2016).
He, R. et al. Beat-to-beat ambulatory blood pressure estimation based on random forest. Proceedings of the 2016 IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks (BSN) pp 194–198 (IEEE, 2016).
Suzuki, S. & Oguri, K. Cuffless blood pressure estimation by error-correcting output coding method based on an aggregation of AdaBoost with a photoplethysmograph sensor. Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society pp 6765–6768 (IEEE, 2009).
Sideris, C., Kalantarian, H., Nemati, E. & Sarrafzadeh, M. Building continuous arterial blood pressure prediction models using recurrent networks. Proceedings of the 2016 IEEE International Conference on Smart Computing (SMARTCOMP) pp 1–5 (IEEE, 2016).
Baek, S., Jang, J. & Yoon, S. End-to-end blood pressure prediction via fully convolutional networks. IEEE Access. 7, 185458–185468 (2019).
Jeong, D. U. & Lim, K. M. Combined deep CNN–LSTM network-based multitasking learning architecture for noninvasive continuous blood pressure estimation using difference in ECG-PPG features. Sci. Rep. 11, 13539 (2021).
Ma, C. et al. KD-informer: a cuff-less continuous blood pressure waveform estimation approach based on single photoplethysmography. IEEE J. Biomed. Heal. Inform. 27, 2219–2230 (2023).
Mieloszyk, R. et al. A comparison of wearable tonometry, photoplethysmography, and electrocardiography for cuffless measurement of blood pressure in an ambulatory setting. IEEE J. Biomed. Heal. Inform. 26, 2864–2875 (2022).
Duan, K., Qian, Z., Atef, M. & Wang, G. A feature exploration methodology for learning based cuffless blood pressure measurement using photoplethysmography. Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society pp 6385–6388 (IEEE, 2016).
Kachuee, M., Kiani, M. M., Mohammadzade, H. & Shabany, M. Cuffless blood pressure estimation algorithms for continuous health-care monitoring. IEEE Trans. Biomed. Eng. 64, 859–869 (2017).
Goli, S. & Jayanthi, T. Cuff less continuous non-invasive blood pressure measurement using pulse transit time measurement. Int. J. Recent. Dev. Eng. Technol. 2, 86–91 (2014).
Mousavi, S. S. et al. Cuff-less blood pressure estimation using only the ECG signal in frequency domain. Proceedings of the 2018 8th International Conference on Computer and Knowledge Engineering (ICCKE) pp 147–152 (IEEE, 2018).
Cattivelli, F. S. & Garudadri, H. Noninvasive cuffless estimation of blood pressure from pulse arrival time and heart rate with adaptive calibration. Proceedings of the 2009 Sixth International Workshop on Wearable and Implantable Body Sensor Networks pp 114–119 (IEEE, 2009).
Zhang, B., Ren, H., Huang, G., Cheng, Y. & Hu, C. Predicting blood pressure from physiological index data using the SVR algorithm 08 information and computing sciences 0801 artificial intelligence and image processing. BMC Bioinforma. 20, 109 (2019).
Yi, C., Jian, C. & Wenqiang, J. Continuous blood pressure measurement based on photoplethysmography. Proceedings of the 2019 14th IEEE International Conference on Electronic Measurement and Instruments (ICEMI) pp 1656–1663 (2019).
Khalid, S. G., Zhang, J., Chen, F. & Zheng, D. Blood pressure estimation using photoplethysmography only: comparison between different machine learning approaches. J. Healthc. Eng. 2018, 1548647 (2018).
Krizhevsky, A., Sutskever, I. & Hinton, G. E. ImageNet classification with deep convolutional neural networks. Commun. ACM 60, 84–90 (2017).
Hattiya, T., Dittakan, K. & Musikasuwan, S. Diabetic retinopathy detection using convolutional neural network: a comparative study on different architectures. Eng. Access. 7, 50–60 (2021).
Liu, Z. et al. A ConvNet for the 2020s. Proceedings of the 2022 IEEE/CVF Conference on Computer Vision and Pattern Pattern Recognition pp 11966–11976 (IEEE, 2022).
Woo, S. et al. ConvNeXt V2: co-designing and scaling ConvNets with masked autoencoders. Proceedings of the 2023 IEEE/CVF Conference on Computer Vision and Pattern Recognition pp 16133–16142 (IEEE, 2023).
Dosovitskiy, A. et al. An image Is worth 16×16 words: transformers for image recognition at scale. ICLR 2021 — 9th Int. Conf. Learn. Represent. (ICLR, 2021).
Arnab, A. et al. ViViT: a video vision transformer. Proceedings of the IEEE/CVF International Conference on Compute Vision (ICCV) pp 6816–6826 (IEEE, 2021).
Radford, A. Improving language understanding by generative pre-training. Homol. Homotopy Appl. 9, 399–438 (2018).
Raffel, C. et al. Exploring the limits of transfer learning with a unified text-to-text transformer. J. Mach. Learn. Res. 21, 1–67 (2020).
OpenAI. GPT-4 technical report. Preprint at arXiv http://arxiv.org/pdf/2303.08774 (2023).
Devlin, J., Chang, M. W., Lee, K. & Toutanova, K. in Proceedings of the 2019 Conference of the North American Chapter of the Association for Computational Linguistics: Human Language Technologies Vol. 1 (eds Burstein, J., Doran, C. & Solorio, T.) 4171–4186 (Association for Computational Linguistics, 2019).
Abdel-hamid, O. et al. Convolutional neural networks for speech recognition. IEEE/ACM Trans. Audio Speech Lang. Process. 22, 1533–1545 (2014).
Sainath, T. N. et al. Deep convolutional neural networks for large-scale speech tasks. Neural Netw. 64, 39–48 (2015).
Dong, L., Xu, S. & Xu, B. Speech-transformer: a no-recurrence sequence-to-sequence model for speech recognition. Proceedings of the IEEE International Conference on Acoustics Speech and Signal Processing (ICASSP) pp 5884–5888 (IEEE, 2018).
Baldi, P. Autoencoders, unsupervised learning, and deep architectures. PMLR 27, 37–49 (2012).
Li, X., Wu, S. & Wang, L. Blood pressure prediction via recurrent models with contextual layer. WWW'17: Proceedings of the 26th International Conference on World Wide Web pp 685–693 (International World Wide Web Conferences, 2017).
Li, Y. H., Harfiya, L. N., Purwandari, K. & Lin, Y. D. Real-time cuffless continuous blood pressure estimation using deep learning model. Sensors 20, 1–19 (2020).
Hochreiter, S. & Schmidhuber, J. Long short-term memory. Neural Comput. 9, 1735–1780 (1997).
Hüsken, M. & Stagge, P. Recurrent neural networks for time series classification. Neurocomputing 50, 223–235 (2003).
Su, P. et al. Long-term blood pressure prediction with deep recurrent neural networks. Proceedings of the 2018 IEEE EMBS International Conference on Biomedical and Health Informatics pp 323–328 (IEEE, 2018).
Mao, S. & Sejdic, E. A review of recurrent neural network-based methods in computational physiology. IEEE Trans. Neural Netw. Learn. Syst. 34, 6983–7003 (2023).
Senturk, U., Yucedag, I. & Polat, K. Repetitive neural network (RNN) based blood pressure estimation using PPG and ECG signals. Proceedings of the 2018 2nd International Symposium on Multidisciplinary Studies and Innovative Technologies (ISMSIT) pp 1–4 (2018).
Park, S. R. & Lee, J. W. in Proceedings of the 18th Annual Conference of the International Speech Communication Association: Interspeech 2017 (ed. Lacerda, F.) 1993–1997 (ISCA, 2017).
Shimazaki, S., Kawanaka, H., Ishikawa, H., Inoue, K. & Oguri, K. Cuffless blood pressure estimation from only the waveform of photoplethysmography using CNN. Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) pp 5042–5045 (IEEE, 2019).
Eom, H. et al. End-to-end deep learning architecture for continuous blood pressure estimation using attention mechanism. Sensors 20, 2338 (2020).
Esmaelpoor, J., Hassan, M. & Kadkhodamohammadi, A. A multistage deep neural network model for blood pressure estimation using photoplethysmogram signals. Comput. Biol. Med. 120, 103719 (2020).
Shi, Y., Yuan, W., Hu, S. & Lou, Y. Convolutional quasi-recurrent network for real-time speech enhancement. J. Xidian Univ. 49, 183–190 (2022).
Zihlmann, M., Perekrestenko, D. & Tschannen, M. Convolutional recurrent neural networks for electrocardiogram classification. Comput. Cardiol. 44, 1–4 (2017).
Keren, G. & Schuller, B. Convolutional RNN: an enhanced model for extracting features from sequential data. Proceedings of the International Joint Conference on Neural Networks (IJCNN) pp 3412–3419 (IEEE, 2016).
Mohiuddin, K. et al. Retention is all you need. CIKM '23: Proceedings of the 32nd ACM International Conference on Information and Knowledge Management.pp 4752–4758 (Association for Computing Machinery, 2023).
Celler, B. G., Le, P. N., Argha, A. & Ambikairajah, E. Blood pressure estimation using time domain features of auscultatory waveforms and GMM-HMM classification approach. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2019, 208–211 (2019).
Sadrawi, M. et al. Genetic deep convolutional autoencoder applied for generative continuous arterial blood pressure via photoplethysmography. Sensors 20, 3829 (2020).
Taniguchi, H. et al. in Medical Image Computing and Computer-Assisted Intervention – MICCAI 2015 (eds Navab, N., Hornegger, J, Wells, M. W. & Frangi, A. F) 209–217 (Springer, 2015).
Athaya, T. & Choi, S. An estimation method of continuous non-invasive arterial blood pressure waveform using photoplethysmography: a U-net architecture-based approach. Sensors 21, 1867 (2021).
Mahmud, S. et al. A shallow U-net architecture for reliably predicting blood pressure (BP) from photoplethysmogram (PPG) and electrocardiogram (ECG) signals. Sensors 22, 919 (2022).
Mehrabadi, M. A., Aqajari, S. A. H., Zargari, A. H. A., Dutt, N. & Rahmani, A. M. Novel blood pressure waveform reconstruction from photoplethysmography using cycle generative adversarial networks. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2022, 1906–1909 (2022).
Min, S. et al. Clinical validation of a wearable piezoelectric blood‐pressure sensor for continuous health monitoring. Adv. Mater. 35, e2301627 (2023).
Zhou, S. et al. Clinical validation of a wearable ultrasound sensor of blood pressure. Nat. Biomed. Eng. https://doi.org/10.1038/s41551-024-01279-3 (2024).
Kouz, K., Scheeren, T. W. L., De Backer, D. & Saugel, B. Pulse wave analysis to estimate cardiac output. Anesthesiology 134, 119–126 (2021).
Qiu, S., Yan, B. P. Y. & Zhao, N. Stroke-volume-allocation model enabling wearable sensors for vascular age and cardiovascular disease assessment. NPJ Flex. Electron. 8, 24 (2024).
Pollreisz, D. & TaheriNejad, N. Detection and removal of motion artifacts in PPG signals. Mob. Netw. Appl. 27, 728–738 (2022).
Sayer, G. et al. Continuous monitoring of blood pressure using a wrist-worn cuffless device. Am. J. Hypertens. 35, 407–413 (2022).
Trudeau, L. Central blood pressure as an index of antihypertensive control: determinants and potential value. Can. J. Cardiol. 30, S23–S28 (2014).
Kim, J. S., Kim, D. W., Jung, H. T. & Choi, J. W. Controlled lithium dendrite growth by a synergistic effect of multilayered graphene coating and an electrolyte additive. Chem. Mater. 27, 2780–2787 (2015).
Deng, R. & He, T. Flexible solid-state lithium-ion batteries: materials and structures. Energies 16, 4549 (2023).
Gljušćić, P., Zelenika, S., Blažević, D. & Kamenar, E. Kinetic energy harvesting for wearable medical sensors. Sensors 19, 4922 (2019).
Mo, X. et al. Piezoelectrets for wearable energy harvesters and sensors. Nano Energy 65, 104033 (2019).
Zou, Y., Raveendran, V. & Chen, J. Wearable triboelectric nanogenerators for biomechanical energy harvesting. Nano Energy 77, 105303 (2020).
Nozariasbmarz, A. et al. Review of wearable thermoelectric energy harvesting: from body temperature to electronic systems. Appl. Energy 258, 114069 (2020).
Wang, Y. et al. Self-powered wearable pressure sensing system for continuous healthcare monitoring enabled by flexible thin-film thermoelectric generator. Nano Energy 73, 104773 (2020).
Oh, Y. S. et al. Battery-free, wireless soft sensors for continuous multi-site measurements of pressure and temperature from patients at risk for pressure injuries. Nat. Commun. 12, 5008 (2021).
Lin, R. et al. Wireless battery-free body sensor networks using near-field-enabled clothing. Nat. Commun. 11, 444 (2020).
Ouyang, W. et al. A wireless and battery-less implant for multimodal closed-loop neuromodulation in small animals. Nat. Biomed. Eng. 7, 1252–1269 (2023).
Li, J. et al. Thin, soft, wearable system for continuous wireless monitoring of artery blood pressure. Nat. Commun. 14, 5009 (2023).
Ge, Y. et al. Contactless WiFi sensing and monitoring for future healthcare - emerging trends, challenges, and opportunities. IEEE Rev. Biomed. Eng. 16, 171–191 (2023).
Enriko, I. K. A. & Gustiyana, F. N. Wi-Fi HaLow: literature review about potential use of technology in agriculture and smart cities in Indonesia. Proceedings of the 2024 International Conference on Green Energy, Computing and Sustainable Technology (GECOST) pp 277–281 (IEEE, 2024).
Yoo, J. Y. et al. Wireless broadband acousto-mechanical sensing system for continuous physiological monitoring. Nat. Med. 29, 3137–3148 (2023).
Bai, L., Ciravegna, F., Bond, R. & Mulvenna, M. A low cost indoor positioning system using bluetooth low energy. IEEE Access. 8, 136858–136871 (2020).
Selvan, S., Zaman, M., Gobbi, R. & Wong, H. Y. Recent advances in the design and development of radio frequency-based energy harvester for powering wireless sensors: a review. J. Electromagn. Waves Appl. 32, 2110–2134 (2018).
Kwon, K. et al. A battery-less wireless implant for the continuous monitoring of vascular pressure, flow rate and temperature. Nat. Biomed. Eng. 7, 1215–1228 (2023).
Boutry, C. M. et al. Biodegradable and flexible arterial-pulse sensor for the wireless monitoring of blood flow. Nat. Biomed. Eng. 3, 47–57 (2019).
Smuck, M., Odonkor, C. A., Wilt, J. K., Schmidt, N. & Swiernik, M. A. The emerging clinical role of wearables: factors for successful implementation in healthcare. NPJ Digit. Med. 4, 45 (2021).
Stergiou, G. S. et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. Hypertension 71, 368–374 (2018).
Acknowledgements
The authors receive support from the National Research Foundation of Korea (NRF) by grants funded by the Korean government (MSIT; RS-2024-00406240 and RS-2023-00273231).
Author information
Authors and Affiliations
Contributions
S.M., J.A., J.H.L. and J.H.K. researched data for the article; S.M., J.A., J.H.L. and S.H.E. wrote the manuscript; S.M., J.A., J.H.L., H.-S.A. and J.-Y.H. contributed to the discussion of its content; and K.J.L., D.J.J., C.D.Y., S.X. and J.A.R. reviewed or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interest.
Peer review
Peer review information
Nature Reviews Cardiology thanks Alberto Avolio and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Min, S., An, J., Lee, J.H. et al. Wearable blood pressure sensors for cardiovascular monitoring and machine learning algorithms for blood pressure estimation. Nat Rev Cardiol 22, 629–648 (2025). https://doi.org/10.1038/s41569-025-01127-0
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41569-025-01127-0
This article is cited by
-
Mechanomedicine
Nature Reviews Bioengineering (2026)
-
Artificial Intelligence-Enhanced Wearable Blood Pressure Monitoring in Resource-Limited Settings: A Co-Design of Sensors, Model, and Deployment
Nano-Micro Letters (2026)
-
Hypertension in 2025: are we ready for bold precision public health approaches worldwide?
Nature Reviews Cardiology (2025)
-
A textile-based alignment-free electrophysiological sensing sleeve for comprehensive cardiovascular monitoring
Microsystems & Nanoengineering (2025)
-
Enhancing long-term adherence in elderly stroke rehabilitation through a digital health approach based on multimodal feedback and personalized intervention
Scientific Reports (2025)