Abstract
Type 2 diabetes mellitus (T2DM) is a major global health concern. Medical nutrition therapy has a key role in T2DM management, with dietary interventions being central to improving glycaemic control and overall metabolic health. Growing evidence suggests that certain dietary strategies can exert direct metabolic benefits independent of weight reduction. The Mediterranean diet has consistently demonstrated metabolic and cardiovascular benefits, along with improved glycaemic control, even in the absence of substantial weight reduction. Low-energy and very-low-energy diets, characterized by moderate to severe caloric restriction, respectively, have also been associated with improvements in cardiometabolic markers and glycaemic regulation. Ketogenic diets promote nutritional ketosis and have shown benefits on glycaemic control, insulin sensitivity and other metabolic outcomes, often preceding substantial weight loss. Intermittent fasting strategies, such as alternate-day fasting or the 5:2 model, and time-restricted eating, have likewise been linked to enhanced glycaemic control and favourable metabolic and cardiovascular effects, although their long-term efficacy and safety require further investigation. This Review aims to provide an evidence-based synthesis of the main nutritional strategies used in the treatment of T2DM, with a focus on their underlying mechanisms, clinical efficacy and potential for sustainable long-term implementation.
Key points
-
Personalized medical nutrition therapy is a cornerstone of type 2 diabetes mellitus (T2DM) management, with evidence supporting its role in improving glycaemic control and insulin sensitivity and in reducing diabetes mellitus-related complications in individuals both with and without obesity.
-
The Mediterranean diet exerts beneficial effects on glycaemic control, systemic inflammation and oxidative stress via several bioactive compounds such as polyphenols and omega-3 fatty acids as well as by promoting gut microbiota health and diversity.
-
Low-energy and very-low-energy diets can induce substantial weight loss and lead to T2DM remission, particularly when implemented early in the disease course.
-
Ketogenic diets, including very-low-energy ketogenic therapies, improve glycaemic outcomes and reduce insulin resistance by inducing nutritional ketosis; however, they vary in composition and require individualized use due to potential safety concerns.
-
Intermittent fasting approaches, such as 5:2 fasting and alternate-day fasting, and time-restricted eating, show promising results for weight loss, glycaemic control and medication reduction in T2DM. Their effectiveness can be enhanced when aligned with circadian rhythms.
-
Research on integrating medical nutrition therapy with pharmacological treatments such as incretin-based therapies could provide comprehensive solutions for T2DM management.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Standl, E., Khunti, K., Hansen, T. B. & Schnell, O. The global epidemics of diabetes in the 21st century: current situation and perspectives. Eur. J. Prev. Cardiol. 26, 7–14 (2019).
Davies, M. J. et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 65, 1925–1966 (2022).
Powers, M. A. et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care and Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. J. Acad. Nutr. Diet. 121, 773–788.e9 (2021).
Lingvay, I., Sumithran, P., Cohen, R. V. & le Roux, C. W. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet 399, 394–405 (2022).
Guasch-Ferre, M. & Willett, W. C. The Mediterranean diet and health: a comprehensive overview. J. Intern. Med. 290, 549–566 (2021).
Estruch, R. & Ros, E. The role of the Mediterranean diet on weight loss and obesity-related diseases. Rev. Endocr. Metab. Disord. 21, 315–327 (2020).
Billingsley, H. E. & Carbone, S. The antioxidant potential of the Mediterranean diet in patients at high cardiovascular risk: an in-depth review of the PREDIMED. Nutr. Diabetes 8, 13 (2018).
Sellahewa, L., Khan, C., Lakkunarajah, S. & Idris, I. A systematic review of evidence on the use of very low calorie diets in people with diabetes. Curr. Diabetes Rev. 13, 35–46 (2017).
Juray, S., Axen, K. V. & Trasino, S. E. Remission of type 2 diabetes with very low-calorie diets — a narrative review. Nutrients 13, 2086 (2021).
Casanueva, F. F. et al. Ketogenic diets as treatment of obesity and type 2 diabetes mellitus. Rev. Endocr. Metab. Disord. 21, 381–397 (2020).
Barrea, L. et al. A new nomenclature for the very low-calorie ketogenic diet (VLCKD): very low-energy ketogenic therapy (VLEKT). Ketodiets and nutraceuticals expert panels: “KetoNut”, Italian society of nutraceuticals (SINut) and the Italian association of dietetics and clinical nutrition (ADI). Curr. Nutr. Rep. 13, 552–556 (2024).
Trimboli, P., Castellana, M., Bellido, D. & Casanueva, F. F. Confusion in the nomenclature of ketogenic diets blurs evidence. Rev. Endocr. Metab. Disord. 21, 1–3 (2020).
Castellana, M. et al. Efficacy and safety of very low calorie ketogenic diet (VLCKD) in patients with overweight and obesity: a systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 21, 5–16 (2020).
Muscogiuri, G. et al. European guidelines for obesity management in adults with a very low-calorie ketogenic diet: a systematic review and meta-analysis. Obes. Facts 14, 222–245 (2021).
Kim, E. R. et al. Short term isocaloric ketogenic diet modulates NLRP3 inflammasome via B-hydroxybutyrate and fibroblast growth factor 21. Front. Immunol. 13, 843520 (2022).
Rosenbaum, M. et al. Glucose and lipid homeostasis and inflammation in humans following an isocaloric ketogenic diet. Obesity 27, 971–981 (2019).
Borgundvaag, E., Mak, J. & Kramer, C. K. Metabolic impact of intermittent fasting in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of interventional studies. J. Clin. Endocrinol. Metab. 106, 902–911 (2021).
Esposito, K. et al. A journey into a Mediterranean diet and type 2 diabetes: a systematic review with meta-analyses. BMJ Open 5, e008222 (2015).
Schwingshackl, L., Missbach, B., Konig, J. & Hoffmann, G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr. 18, 1292–1299 (2015).
Esposito, K. et al. Which diet for prevention of type 2 diabetes? A meta-analysis of prospective studies. Endocrine 47, 107–116 (2014).
Huo, R. et al. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur. J. Clin. Nutr. 69, 1200–1208 (2015).
Panagiotakos, D. B. et al. The association between adherence to the Mediterranean diet and fasting indices of glucose homoeostasis: the ATTICA Study. J. Am. Coll. Nutr. 26, 32–38 (2007).
Estruch, R. et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann. Intern. Med. 145, 1–11 (2006).
Toobert, D. J. et al. Biologic and quality-of-life outcomes from the Mediterranean lifestyle program: a randomized clinical trial. Diabetes Care 26, 2288–2293 (2003).
Elhayany, A., Lustman, A., Abel, R., Attal-Singer, J. & Vinker, S. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes. Metab. 12, 204–209 (2010).
Rathmann, W., Kostev, K. & Haastert, B. Glycemic durability of monotherapy for diabetes. N. Engl. J. Med. 356, 1378–1379 (2007).
Esposito, K. et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann. Intern. Med. 151, 306–314 (2009).
Song, Y., Cook, N. R., Albert, C. M., Van Denburgh, M. & Manson, J. E. Effects of vitamins C and E and β-carotene on the risk of type 2 diabetes in women at high risk of cardiovascular disease: a randomized controlled trial. Am. J. Clin. Nutr. 90, 429–437 (2009).
Itsiopoulos, C. et al. Can the Mediterranean diet lower HbA1c in type 2 diabetes? Results from a randomized cross-over study. Nutr. Metab. Cardiovasc. Dis. 21, 740–747 (2011).
Zamora-Ros, R. et al. Mediterranean diet and non enzymatic antioxidant capacity in the PREDIMED study: evidence for a mechanism of antioxidant tuning. Nutr. Metab. Cardiovasc. Dis. 23, 1167–1174 (2013).
Maiorino, M. I. et al. Mediterranean diet cools down the inflammatory milieu in type 2 diabetes: the MEDITA randomized controlled trial. Endocrine 54, 634–641 (2016).
Ceriello, A. et al. The protective effect of the Mediterranean diet on endothelial resistance to GLP-1 in type 2 diabetes: a preliminary report. Cardiovasc. Diabetol. 13, 140 (2014).
Eid, H. M. et al. Stimulation of AMP-activated protein kinase and enhancement of basal glucose uptake in muscle cells by quercetin and quercetin glycosides, active principles of the antidiabetic medicinal plant Vaccinium vitis-idaea. Mol. Nutr. Food Res. 54, 991–1003 (2010).
Dhanya, R., Arya, A. D., Nisha, P. & Jayamurthy, P. Quercetin, a lead compound against type 2 diabetes ameliorates glucose uptake via AMPK pathway in skeletal muscle cell line. Front. Pharmacol. 8, 336 (2017).
Tuck, K. L. & Hayball, P. J. Major phenolic compounds in olive oil: metabolism and health effects. J. Nutr. Biochem. 13, 636–644 (2002).
Torres-Pena, J. D. et al. Mediterranean diet improves endothelial function in patients with diabetes and prediabetes: a report from the CORDIOPREV study. Atherosclerosis 269, 50–56 (2018).
Berger, M. M. et al. Three short perioperative infusions of n-3 PUFAs reduce systemic inflammation induced by cardiopulmonary bypass surgery: a randomized controlled trial. Am. J. Clin. Nutr. 97, 246–254 (2013).
Maedler, K., Oberholzer, J., Bucher, P., Spinas, G. A. & Donath, M. Y. Monounsaturated fatty acids prevent the deleterious effects of palmitate and high glucose on human pancreatic β-cell turnover and function. Diabetes 52, 726–733 (2003).
Carpentier, Y. A., Portois, L. & Malaisse, W. J. n-3 fatty acids and the metabolic syndrome. Am. J. Clin. Nutr. 83, 1499S–1504S (2006).
Beauchamp, G. K. et al. Phytochemistry: ibuprofen-like activity in extra-virgin olive oil. Nature 437, 45–46 (2005).
Oh, D. Y. et al. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 142, 687–698 (2010).
Yan, Y. et al. Omega-3 fatty acids prevent inflammation and metabolic disorder through inhibition of NLRP3 inflammasome activation. Immunity 38, 1154–1163 (2013).
Di Mauro, A. et al. The Mediterranean diet increases glucagon-like peptide 1 and oxyntomodulin compared with a vegetarian diet in patients with type 2 diabetes: a randomized controlled cross-over trial. Diabetes Metab. Res. Rev. 37, e3406 (2021).
Huber, H., Schieren, A., Holst, J. J. & Simon, M. C. Dietary impact on fasting and stimulated GLP-1 secretion in different metabolic conditions — a narrative review. Am. J. Clin. Nutr. 119, 599–627 (2024).
Rodriguez, P. J. et al. Semaglutide vs tirzepatide for weight loss in adults with overweight or obesity. JAMA Intern. Med. 184, 1056–1064 (2024).
Nie, C., He, T., Zhang, W., Zhang, G. & Ma, X. Branched chain amino acids: beyond nutrition metabolism. Int. J. Mol. Sci. 19, 954 (2018).
Guasch-Ferre, M. et al. Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care 39, 833–846 (2016).
Ruiz-Canela, M. et al. Plasma branched chain/aromatic amino acids, enriched Mediterranean diet and risk of type 2 diabetes: case-cohort study within the PREDIMED Trial. Diabetologia 61, 1560–1571 (2018).
Larsen, N. et al. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS ONE 5, e9085 (2010).
Karlsson, F. H. et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498, 99–103 (2013).
Sato, J. et al. Gut dysbiosis and detection of “live gut bacteria” in blood of Japanese patients with type 2 diabetes. Diabetes Care 37, 2343–2350 (2014).
Qin, J. et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490, 55–60 (2012).
Florkowski, M., Abiona, E., Frank, K. M. & Brichacek, A. L. Obesity-associated inflammation countered by a Mediterranean diet: the role of gut-derived metabolites. Front. Nutr. 11, 1392666 (2024).
Sanz, Y. et al. The gut microbiome connects nutrition and human health. Nat. Rev. Gastroenterol. Hepatol. 22, 534–555 (2025).
Zhao, L. et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science 359, 1151–1156 (2018).
McCreight, L. J., Bailey, C. J. & Pearson, E. R. Metformin and the gastrointestinal tract. Diabetologia 59, 426–435 (2016).
Zhu, C. et al. Human gut microbiome composition and tryptophan metabolites were changed differently by fast food and Mediterranean diet in 4 days: a pilot study. Nutr. Res. 77, 62–72 (2020).
Churuangsuk, C. et al. Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia 65, 14–36 (2022).
Lean, M. E. et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391, 541–551 (2018).
Lean, M. E. J. et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 7, 344–355 (2019).
Lim, E. L. et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54, 2506–2514 (2011).
Mraz, M. et al. The effect of very-low-calorie diet on mRNA expression of inflammation-related genes in subcutaneous adipose tissue and peripheral monocytes of obese patients with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 96, E606–E613 (2011).
Lean, M. E. et al. 5-year follow-up of the randomised diabetes remission clinical trial (DiRECT) of continued support for weight loss maintenance in the UK: an extension study. Lancet Diabetes Endocrinol. 12, 233–246 (2024).
Caprio, M. et al. Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: systematic review and consensus statement from the Italian Society of Endocrinology (SIE). J. Endocrinol. Invest. 42, 1365–1386 (2019).
Ghasemi, P. et al. Impact of very low carbohydrate ketogenic diets on cardiovascular risk factors among patients with type 2 diabetes; GRADE-assessed systematic review and meta-analysis of clinical trials. Nutr. Metab. 21, 50 (2024).
Barrea, L. et al. Very low-calorie ketogenic diet (VLCKD): an antihypertensive nutritional approach. J. Transl. Med. 21, 128 (2023).
Barrea, L. et al. VLCKD: a real time safety study in obesity. J. Transl. Med. 20, 23 (2022).
Moriconi, E., Camajani, E., Fabbri, A., Lenzi, A. & Caprio, M. Very-low-calorie ketogenic diet as a safe and valuable tool for long-term glycemic management in patients with obesity and type 2 diabetes. Nutrients 13, 758 (2021).
Muscogiuri, G. et al. Weight loss, changes in body composition and inflammatory status after a very low-energy ketogenic therapy (VLEKT): does gender matter? J. Transl. Med. 22, 949 (2024).
Correa, L. L. et al. Severe type 2 diabetes (T2D) remission using a very low-calorie ketogenic diet (VLCKD). Endocrinol. Diabetes Metab. Case Rep. 2022, 22-0295 (2022).
Yuan, X. et al. Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2DM: a systematic review and meta-analysis. Nutr. Diabetes 10, 38 (2020).
Abdul-Ghani, M. A., Jayyousi, A., DeFronzo, R. A., Asaad, N. & Al-Suwaidi, J. Insulin resistance the link between T2DM and CVD: basic mechanisms and clinical implications. Curr. Vasc. Pharmacol. 17, 153–163 (2019).
Farres, J. et al. Revealing the molecular relationship between type 2 diabetes and the metabolic changes induced by a very-low-carbohydrate low-fat ketogenic diet. Nutr. Metab. 7, 88 (2010).
Okuda, T., Fukui, A. & Morita, N. Altered expression of O-GlcNAc-modified proteins in a mouse model whose glycemic status is controlled by a low carbohydrate ketogenic diet. Glycoconj. J. 30, 781–789 (2013).
Yang, Z. et al. Effects of low-carbohydrate diet and ketogenic diet on glucose and lipid metabolism in type 2 diabetic mice. Nutrition 89, 111230 (2021).
Zhang, Q. et al. Treatment of diabetic mice with a combination of ketogenic diet and aerobic exercise via modulations of PPARs gene programs. PPAR Res. 2018, 4827643 (2018).
Youm, Y. H. et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat. Med. 21, 263–269 (2015).
Patel, S. & Santani, D. Role of NF-kappa B in the pathogenesis of diabetes and its associated complications. Pharmacol. Rep. 61, 595–603 (2009).
Jamshed, H. et al. Early time-restricted feeding improves 24-hour glucose levels and affects markers of the circadian clock, aging, and autophagy in humans. Nutrients 11, 1234 (2019).
American Diabetes Association. Lifestyle management: standards of medical care in diabetes–2019. Diabetes Care 42, S46–S60 (2019).
Blau, J. E., Tella, S. H., Taylor, S. I. & Rother, K. I. Ketoacidosis associated with SGLT2 inhibitor treatment: analysis of FAERS data. Diabetes Metab. Res. Rev. 33, e2924 (2017).
Parry-Strong, A. et al. Very low carbohydrate (ketogenic) diets in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Obes. Metab. 24, 2431–2442 (2022).
Albosta, M. & Bakke, J. Intermittent fasting: is there a role in the treatment of diabetes? A review of the literature and guide for primary care physicians. Clin. Diabetes Endocrinol. 7, 3 (2021).
Carter, S., Clifton, P. M. & Keogh, J. B. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Netw. Open 1, e180756 (2018).
Corley, B. T. et al. Intermittent fasting in type 2 diabetes mellitus and the risk of hypoglycaemia: a randomized controlled trial. Diabet. Med. 35, 588–594 (2018).
Li, C. et al. Effects of a one-week fasting therapy in patients with type-2 diabetes mellitus and metabolic syndrome — a randomized controlled explorative study. Exp. Clin. Endocrinol. Diabetes 125, 618–624 (2017).
Arnason, T. G., Bowen, M. W. & Mansell, K. D. Effects of intermittent fasting on health markers in those with type 2 diabetes: a pilot study. World J. Diabetes 8, 154–164 (2017).
Kahleova, H. et al. Eating two larger meals a day (breakfast and lunch) is more effective than six smaller meals in a reduced-energy regimen for patients with type 2 diabetes: a randomised crossover study. Diabetologia 57, 1552–1560 (2014).
Pavlou, V. et al. Effect of time-restricted eating on weight loss in adults with type 2 diabetes: a randomized clinical trial. JAMA Netw. Open 6, e2339337 (2023).
Lowe, D. A. et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern. Med. 180, 1491–1499 (2020).
Rebello, C. J. et al. From starvation to time-restricted eating: a review of fasting physiology. Int. J. Obes. 49, 43–48 (2024).
Storoschuk, K. L. et al. Impact of fasting on the AMPK and PGC-1α axis in rodent and human skeletal muscle: a systematic review. Metabolism 152, 155768 (2024).
Vendelbo, M. H. et al. Fasting increases human skeletal muscle net phenylalanine release and this is associated with decreased mTOR signaling. PLoS ONE 9, e102031 (2014).
Liu, Z. et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat. Commun. 11, 855 (2020).
Perez-Gerdel, T., Camargo, M., Alvarado, M. & Ramirez, J. D. Impact of intermittent fasting on the gut microbiota: a systematic review. Adv. Biol. 7, e2200337 (2023).
Palmnas-Bedard, M. S. A. et al. The human gut microbiota and glucose metabolism: a scoping review of key bacteria and the potential role of SCFAs. Am. J. Clin. Nutr. 116, 862–874 (2022).
Stratton, M. T. et al. Physiological responses to acute fasting: implications for intermittent fasting programs. Nutr. Rev. 80, 439–452 (2022).
Zauner, C. et al. Resting energy expenditure in short-term starvation is increased as a result of an increase in serum norepinephrine. Am. J. Clin. Nutr. 71, 1511–1515 (2000).
Longo, V. D. & Panda, S. Fasting, circadian rhythms, and time-restricted feeding in healthy lifespan. Cell Metab. 23, 1048–1059 (2016).
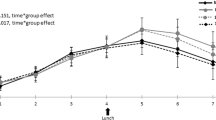
Chamorro, R. et al. Meal timing across the day modulates daily energy intake in adult patients with type 2 diabetes. Eur. J. Clin. Nutr. 76, 1470–1477 (2022).
Jakubowicz, D. et al. Reduction in glycated hemoglobin and daily insulin dose alongside circadian clock upregulation in patients with type 2 diabetes consuming a three-meal diet: a randomized clinical trial. Diabetes Care 42, 2171–2180 (2019).
Jakubowicz, D. et al. High-energy breakfast with low-energy dinner decreases overall daily hyperglycaemia in type 2 diabetic patients: a randomised clinical trial. Diabetologia 58, 912–919 (2015).
Cross, L. V. & Thomas, J. R. Safety and efficacy of dietary supplements for diabetes. Diabetes Spectr. 34, 67–72 (2021).
Ansar, H., Mazloom, Z., Kazemi, F. & Hejazi, N. Effect of alpha-lipoic acid on blood glucose, insulin resistance and glutathione peroxidase of type 2 diabetic patients. Saudi Med. J. 32, 584–588 (2011).
Ziegler, D. et al. Efficacy and safety of antioxidant treatment with α-lipoic acid over 4 years in diabetic polyneuropathy: the NATHAN 1 trial. Diabetes Care 34, 2054–2060 (2011).
Segermann, J., Hotze, A., Ulrich, H. & Rao, G. S. Effect of alpha-lipoic acid on the peripheral conversion of thyroxine to triiodothyronine and on serum lipid-, protein- and glucose levels. Arzneimittelforschung 41, 1294–1298 (1991).
Yin, R. V., Lee, N. C., Hirpara, H. & Phung, O. J. The effect of bitter melon (Mormordica charantia) in patients with diabetes mellitus: a systematic review and meta-analysis. Nutr. Diabetes 4, e145 (2014).
Dans, A. M. et al. The effect of Momordica charantia capsule preparation on glycemic control in type 2 diabetes mellitus needs further studies. J. Clin. Epidemiol. 60, 554–559 (2007).
Lan, J. et al. Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. J. Ethnopharmacol. 161, 69–81 (2015).
Guo, Y., Chen, Y., Tan, Z. R., Klaassen, C. D. & Zhou, H. H. Repeated administration of berberine inhibits cytochromes P450 in humans. Eur. J. Clin. Pharmacol. 68, 213–217 (2012).
Rad, S. Z. K., Rameshrad, M. & Hosseinzadeh, H. Toxicology effects of Berberis vulgaris (barberry) and its active constituent, berberine: a review. Iran. J. Basic Med. Sci. 20, 516–529 (2017).
Balk, E. M., Tatsioni, A., Lichtenstein, A. H., Lau, J. & Pittas, A. G. Effect of chromium supplementation on glucose metabolism and lipids: a systematic review of randomized controlled trials. Diabetes Care 30, 2154–2163 (2007).
Cerulli, J., Grabe, D. W., Gauthier, I., Malone, M. & McGoldrick, M. D. Chromium picolinate toxicity. Ann. Pharmacother. 32, 428–431 (1998).
Allen, R. W., Schwartzman, E., Baker, W. L., Coleman, C. I. & Phung, O. J. Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis. Ann. Fam. Med. 11, 452–459 (2013).
Gong, J. et al. Effect of fenugreek on hyperglycaemia and hyperlipidemia in diabetes and prediabetes: a meta-analysis. J. Ethnopharmacol. 194, 260–268 (2016).
Talukdar, J. R. et al. Effects of inulin-type fructans supplementation on cardiovascular disease risk factors: a protocol for a systematic review and meta-analysis of randomised controlled trials. BMJ Open 12, e058875 (2022).
Choi, S., Oh, D. S. & Jerng, U. M. A systematic review of the pharmacokinetic and pharmacodynamic interactions of herbal medicine with warfarin. PLoS ONE 12, e0182794 (2017).
Palinkas, L. A., Wingard, D. L. & Barrett-Connor, E. Chronic illness and depressive symptoms in the elderly: a population-based study. J. Clin. Epidemiol. 43, 1131–1141 (1990).
Bacardi-Gascon, M., Duenas-Mena, D. & Jimenez-Cruz, A. Lowering effect on postprandial glycemic response of nopales added to Mexican breakfasts. Diabetes Care 30, 1264–1265 (2007).
Onakpoya, I. J., O’Sullivan, J. & Heneghan, C. J. The effect of cactus pear (Opuntia ficus-indica) on body weight and cardiovascular risk factors: a systematic review and meta-analysis of randomized clinical trials. Nutrition 31, 640–646 (2015).
U.S. Food & Drug Administration. Information for Consumers on Using Dietary Supplements https://www.fda.gov/food/information-consumers-using-dietary-supplements/questions-and-answers-dietary-supplements (2024).
Petroni, M. L. et al. Nutrition in patients with type 2 diabetes: present knowledge and remaining challenges. Nutrients 13, 2748 (2021).
Grosso, G. et al. Anti-inflammatory nutrients and obesity-associated metabolic-inflammation: state of the art and future direction. Nutrients 14, 1137 (2022).
Gill, L. E., Bartels, S. J. & Batsis, J. A. Weight management in older adults. Curr. Obes. Rep. 4, 379–388 (2015).
Lewgood, J. et al. Efficacy of dietary and supplementation interventions for individuals with type 2 diabetes. Nutrients 13, 2378 (2021).
Norris, S. L. et al. Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type 2 diabetes: a meta-analysis. Am. J. Med. 117, 762–774 (2004).
Evert, A. B. et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care 42, 731–754 (2019).
Nauck, M. A., Quast, D. R., Wefers, J. & Meier, J. J. GLP-1 receptor agonists in the treatment of type 2 diabetes — state-of-the-art. Mol. Metab. 46, 101102 (2021).
Mather, K. J. et al. Effects of tirzepatide vs semaglutide on β-cell function, insulin sensitivity, and glucose control during a meal test. J. Clin. Endocrinol. Metab. 109, 3046–3054 (2024).
Heise, T. et al. Tirzepatide reduces appetite, energy intake, and fat mass in people with type 2 diabetes. Diabetes Care 46, 998–1004 (2023).
Brown, A. et al. “From evidence to practice” — insights from the multidisciplinary team on the optimal integration of GLP-1 receptor agonists in obesity management services. Nutr. Bull. 49, 257–263 (2024).
Anyiam, O. et al. Metabolic effects of very-low calorie diet, semaglutide, or combination of the two, in individuals with type 2 diabetes mellitus. Clin. Nutr. 43, 1907–1913 (2024).
Schiavo, L. et al. Preliminary evidence suggests that a 12-week treatment with tirzepatide plus low-energy ketogenic therapy is more effective than its combination with a low-calorie diet in preserving fat-free mass, muscle strength, and resting metabolic rate in patients with obesity. Nutrients 17, 1216 (2025).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article. L.V. researched data for the article. L.B. and L.V. wrote the article. L.B., A.C., L.J.M. and G.M. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barrea, L., Verde, L., Colao, A. et al. Medical nutrition therapy for the management of type 2 diabetes mellitus. Nat Rev Endocrinol 21, 769–782 (2025). https://doi.org/10.1038/s41574-025-01161-5
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41574-025-01161-5
This article is cited by
-
Nutrition and longevity – diet in centenarians
Journal of Translational Medicine (2026)