Abstract
The global incidence of thyroid cancer has risen sharply since the 1980s, whereas thyroid cancer mortality rates have remained relatively stable. Much of the increase in incidence can be attributed to overdiagnosis of small and indolent papillary thyroid cancers, which has largely been driven by widespread (and sometimes inappropriate) use of imaging studies, especially thyroid and neck ultrasonography. To a lesser extent, increases in the incidence rate of advanced-stage thyroid cancer over the past four decades have also contributed to the observed trends. This Review describes changes in the incidence of thyroid cancer over the past 40 years, outlines well-known and potential risk factors, including obesity and environmental exposures, and explores strategies to address the public-health issues of overdiagnosis and the consequent overtreatment of thyroid cancer.
Key points
-
Between 1980 and 2017, global thyroid cancer incidence rates increased while mortality rates remained relatively stable.
-
Radiation exposure is the only well-established modifiable risk factor for thyroid cancer.
-
Emerging data suggest that obesity and environmental exposures might also contribute to thyroid cancer development.
-
Overdiagnosis of small indolent thyroid cancers, largely driven by increased use of thyroid ultrasonography, accounts for much of the global rise in thyroid cancer incidence.
-
Multilevel interventions are necessary to address the public-health issue of thyroid cancer overdiagnosis and subsequent overtreatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ferlay, J. et al. Global cancer observatory: cancer today. International Agency for Research on Cancer https://gco.iarc.who.int/media/globocan/factsheets/populations/900-world-fact-sheet.pdf (2024).
Pizzato, M. et al. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 10, 264–272 (2022).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
SEER. Cancer stat facts: thyroid cancer. National Cancer Institute Surveillance, Epidemiology, and End Results Program https://seer.cancer.gov/statfacts/html/thyro.html (2025).
Page, L. L. et al. Prevalence of cancer survivors diagnosed during adolescence and young adulthood in the United States. J. Natl. Cancer Inst. 117, 529–536 (2024).
National Cancer Institute. Adolescents and young adults with cancer. National Cancer Institute https://www.cancer.gov/types/aya (2025).
Tran, T. V. et al. All-cause and cause-specific mortality among low-risk differentiated thyroid cancer survivors in the United States. Thyroid 34, 215–224 (2024).
Li, M., Dal Maso, L., Pizzato, M. & Vaccarella, S. Evolving epidemiological patterns of thyroid cancer and estimates of overdiagnosis in 2013–17 in 63 countries worldwide: a population-based study. Lancet Diabetes Endocrinol. 12, 824–836 (2024).
Davies, L. & Welch, H. G. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295, 2164–2167 (2006).
Lim, H., Devesa, S. S., Sosa, J. A., Check, D. & Kitahara, C. M. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA 317, 1338–1348 (2017).
Vaccarella, S. et al. Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. N. Engl. J. Med. 375, 614–617 (2016).
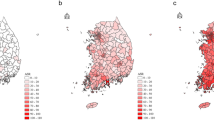
Ahn, H. S., Kim, H. J. & Welch, H. G. Korea’s thyroid-cancer “epidemic” — screening and overdiagnosis. N. Engl. J. Med. 371, 1765–1767 (2014).
Haymart, M. R., Reyes-Gastelum, D., Caoili, E., Norton, E. C. & Banerjee, M. The relationship between imaging and thyroid cancer diagnosis and survival. Oncologist 25, 765–771 (2020).
Dal Maso, L. et al. Incidence of thyroid cancer in Italy, 1991–2005: time trends and age-period-cohort effects. Ann. Oncol. 22, 957–963 (2011).
Haymart, M. R., Banerjee, M., Reyes-Gastelum, D., Caoili, E. & Norton, E. C. Thyroid ultrasound and the increase in diagnosis of low-risk thyroid cancer. J. Clin. Endocrinol. Metab. 104, 785–792 (2019).
Li, M., Dal Maso, L. & Vaccarella, S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 8, 468–470 (2020).
Pandeya, N. et al. Increasing thyroid cancer incidence in Queensland, Australia 1982–2008 — true increase or overdiagnosis? Clin. Endocrinol. 84, 257–264 (2016).
Cosme, I., Figueiredo, A., Pinheiro, S. & Leite, V. Incidentally vs. non-incidentally diagnosed papillary thyroid carcinoma: are there differences? Eur. Thyroid. J. 13, e240106 (2024).
Straume, T. High-energy gamma rays in Hiroshima and Nagasaki: implications for risk and WR. Health Phys. 69, 954–956 (1995).
Imaizumi, M. et al. Radiation dose–response relationships for thyroid nodules and autoimmune thyroid diseases in Hiroshima and Nagasaki atomic bomb survivors 55–58 years after radiation exposure. JAMA 295, 1011–1022 (2006).
Parker, L. N., Belsky, J. L., Yamamoto, T., Kawamoto, S. & Keehn, R. J. Thyroid carcinoma after exposure to atomic radiation. A continuing survey of a fixed population, Hiroshima and Nagasaki, 1958–1971. Ann. Intern. Med. 80, 600–604 (1974).
Morton, L. M. et al. Radiation-related genomic profile of papillary thyroid carcinoma after the Chernobyl accident. Science 372, eabg2538 (2021).
Pacini, F. et al. Post-Chernobyl thyroid carcinoma in Belarus children and adolescents: comparison with naturally occurring thyroid carcinoma in Italy and France. J. Clin. Endocrinol. Metab. 82, 3563–3569 (1997).
Shibata, Y., Yamashita, S., Masyakin, V. B., Panasyuk, G. D. & Nagataki, S. 15 years after Chernobyl: new evidence of thyroid cancer. Lancet 358, 1965–1966 (2001).
Kazakov, V. S., Demidchik, E. P. & Astakhova, L. N. Thyroid cancer after Chernobyl. Nature 359, 21 (1992).
Zablotska, L. B. et al. Thyroid cancer risk in Belarus among children and adolescents exposed to radioiodine after the Chornobyl accident. Br. J. Cancer 104, 181–187 (2011).
Cardis, E. & Hatch, M. The Chernobyl accident — an epidemiological perspective. Clin. Oncol. 23, 251–260 (2011).
Hatch, M., Ron, E., Bouville, A., Zablotska, L. & Howe, G. The Chernobyl disaster: cancer following the accident at the Chernobyl nuclear power plant. Epidemiol. Rev. 27, 56–66 (2005).
Suzuki, S. et al. Comprehensive survey results of childhood thyroid ultrasound examinations in Fukushima in the first four years after the Fukushima Daiichi nuclear power plant accident. Thyroid 26, 843–851 (2016).
Tsuda, T., Tokinobu, A., Yamamoto, E. & Suzuki, E. Thyroid cancer detection by ultrasound among residents ages 18 years and younger in Fukushima, Japan: 2011 to 2014. Epidemiology 27, 316–322 (2016).
Bhatti, P. et al. Risk of second primary thyroid cancer after radiotherapy for a childhood cancer in a large cohort study: an update from the childhood cancer survivor study. Radiat. Res. 174, 741–752 (2010).
Schneider, A. B., Ron, E., Lubin, J., Stovall, M. & Gierlowski, T. C. Dose–response relationships for radiation-induced thyroid cancer and thyroid nodules: evidence for the prolonged effects of radiation on the thyroid. J. Clin. Endocrinol. Metab. 77, 362–369 (1993).
Martella, M., Lenzi, J. & Gianino, M. M. Diagnostic technology: trends of use and availability in a 10-year period (2011–2020) among sixteen OECD countries. Healthcare 11, 2078 (2023).
Smith-Bindman, R. et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 307, 2400–2409 (2012).
National Council on Radiation Protection and Measurements. NCRP Report No. 160: Ionizing Radiation Exposure of the Population of the United States https://ncrponline.org/publications/reports/ncrp-report-160/ (NCRP, 2025).
Chang, L. A. et al. Thyroid radiation dose to patients from diagnostic radiology procedures over eight decades: 1930–2010. Health Phys. 113, 458–473 (2017).
Han, M. A. & Kim, J. H. Diagnostic X-ray exposure and thyroid cancer risk: systematic review and meta-analysis. Thyroid 28, 220–228 (2018).
Kitahara, C. M. et al. Occupational radiation exposure and thyroid cancer incidence in a cohort of U.S. radiologic technologists, 1983–2013. Int. J. Cancer 143, 2145–2149 (2018).
Mirkatouli, N. B., Hirota, S. & Yoshinaga, S. Thyroid cancer risk after radiation exposure in adults — systematic review and meta-analysis. J. Radiat. Res. 64, 893–903 (2023).
Smith-Bindman, R. et al. Projected lifetime cancer risks from current computed tomography imaging. JAMA Intern. Med. 85, 710–719 (2025).
Zimmermann, M. B. & Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 3, 286–295 (2015).
Feldt-Rasmussen, U. Iodine and cancer. Thyroid 11, 483–486 (2001).
Zimmermann, M. B. & Galetti, V. Iodine intake as a risk factor for thyroid cancer: a comprehensive review of animal and human studies. Thyroid. Res. 8, 8 (2015).
Mitro, S. D. et al. Iodine deficiency and thyroid cancer trends in three regions of Thailand, 1990–2009. Cancer Epidemiol. 43, 92–99 (2016).
Blomberg, M., Feldt-Rasmussen, U., Andersen, K. K. & Kjaer, S. K. Thyroid cancer in Denmark 1943–2008, before and after iodine supplementation. Int. J. Cancer 131, 2360–2366 (2012).
Pettersson, B., Coleman, M. P., Ron, E. & Adami, H. O. Iodine supplementation in Sweden and regional trends in thyroid cancer incidence by histopathologic type. Int. J. Cancer 65, 13–19 (1996).
Poljak, N. K. et al. Iodine intake and epidemiological characteristics of thyroid cancer: comparison between inland and littoral Croatia. Acta Clin. Croat. 50, 329–339 (2011).
World Health Organization. Controlling the global obesity epidemic. WHO https://www.who.int/activities/controlling-the-global-obesity-epidemic (2025).
International Agency for Research on Cancer. Cancer attributable to obesity. IARC https://gco.iarc.who.int/causes/obesity/home (2025).
Kitahara, C. M., Pfeiffer, R. M., Sosa, J. A. & Shiels, M. S. Impact of overweight and obesity on US papillary thyroid cancer incidence trends (1995–2015). J. Natl. Cancer Inst. 112, 810–817 (2020).
Kwon, H., Han, K. D. & Park, C. Y. Weight change is significantly associated with risk of thyroid cancer: a nationwide population-based cohort study. Sci. Rep. 9, 1546 (2019).
Fussey, J. M. et al. Does obesity cause thyroid cancer? A Mendelian randomization study. J. Clin. Endocrinol. Metab. 105, e2398–e2407 (2020).
Kitahara, C. M. et al. Anthropometric factors and thyroid cancer risk by histological subtype: pooled analysis of 22 prospective studies. Thyroid 26, 306–318 (2016).
Youssef, M. R. et al. Obesity and the prevention of thyroid cancer: impact of body mass index and weight change on developing thyroid cancer — pooled results of 24 million cohorts. Oral. Oncol. 112, 105085 (2021).
Franchini, F. et al. Obesity and thyroid cancer risk: an update. Int. J. Environ. Res. Public. Health 19, 1116 (2022).
Cecchini, M. Use of healthcare services and expenditure in the US in 2025: the effect of obesity and morbid obesity. PLoS ONE 13, e0206703 (2018).
Betts, K. S. Unwelcome guest: PBDEs in indoor dust. Environ. Health Perspect. 116, A202–A208 (2008).
Hoffman, K. et al. Exposure to flame retardant chemicals and occurrence and severity of papillary thyroid cancer: a case–control study. Environ. Int. 107, 235–242 (2017).
Omidakhsh, N. et al. Thyroid cancer and pesticide use in a central California agricultural area: a case control study. J. Clin. Endocrinol. Metab. 107, e3574–e3582 (2022).
Jacome, C. S. et al. Physical examination of the thyroid: accuracy in detecting thyroid nodules and frequency of additional findings. Endocr. Pract. 30, 31–35 (2024).
Guth, S., Theune, U., Aberle, J., Galach, A. & Bamberger, C. M. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur. J. Clin. Invest. 39, 699–706 (2009).
Van den Bruel, A. et al. Regional variation in thyroid cancer incidence in Belgium is associated with variation in thyroid imaging and thyroid disease management. J. Clin. Endocrinol. Metab. 98, 4063–4071 (2013).
Lincango-Naranjo, E. et al. Triggers of thyroid cancer diagnosis: a systematic review and meta-analysis. Endocrine 72, 644–659 (2021).
Miranda-Filho, A. et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 9, 225–234 (2021).
Jung, K. W. et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res. Treat. 44, 11–24 (2012).
Park, S. et al. Association between screening and the thyroid cancer “epidemic” in South Korea: evidence from a nationwide study. BMJ 355, i5745 (2016).
Chen, D. W. et al. Physician-reported misuse of thyroid ultrasonography. JAMA Surg. 155, 984–986 (2020).
Acosta, G. J., Singh Ospina, N. & Brito, J. P. Overuse of thyroid ultrasound. Curr. Opin. Endocrinol. Diabetes Obes. 30, 225–230 (2023).
Edwards, M. K. et al. Inappropriate use of thyroid ultrasound: a systematic review and meta-analysis. Endocrine 74, 263–269 (2021).
Soto Jacome, C. et al. Drivers of thyroid ultrasound use: a retrospective observational study. Endocr. Pract. 29, 948–954 (2023).
Davies, L. & Welch, H. G. Current thyroid cancer trends in the United States. JAMA Otolaryngol. Head. Neck Surg. 140, 317–322 (2014).
Esfandiari, N. H. et al. Factors associated with diagnosis and treatment of thyroid microcarcinomas. J. Clin. Endocrinol. Metab. 104, 6060–6068 (2019).
Yoon, D. Y. et al. The prevalence and significance of incidental thyroid nodules identified on computed tomography. J. Comput. Assist. Tomogr. 32, 810–815 (2008).
Hagenimana, N., Dallaire, J., Vallee, E. & Belzile, M. Thyroid incidentalomas on 18FDG-PET/CT: a metabolico-pathological correlation. J. Otolaryngol. Head. Neck Surg. 46, 22 (2017).
Drake, T., Gravely, A., Westanmo, A. & Billington, C. Prevalence of thyroid incidentalomas from 1995 to 2016: a single-center, retrospective cohort study. J. Endocr. Soc. 4, bvz027 (2020).
Hoang, J. K., Riofrio, A., Bashir, M. R., Kranz, P. G. & Eastwood, J. D. High variability in radiologists’ reporting practices for incidental thyroid nodules detected on CT and MRI. AJNR Am. J. Neuroradiol. 35, 1190–1194 (2014).
Drake, T., Gravely, A., Ensrud, K. & Billington, C. J. Reporting of incidental thyroid nodules on chest computed tomography and the impact on nodule evaluation: a retrospective cohort study. Thyroid 32, 1529–1534 (2022).
Germano, A., Schmitt, W., Almeida, P., Mateus-Marques, R. & Leite, V. Ultrasound requested by general practitioners or for symptoms unrelated to the thyroid gland may explain higher prevalence of thyroid nodules in females. Clin. Imaging 50, 289–293 (2018).
Sosa, J. A., Hanna, J. W., Robinson, K. A. & Lanman, R. B. Increases in thyroid nodule fine-needle aspirations, operations, and diagnoses of thyroid cancer in the United States. Surgery 154, 1420–1426 (2013).
Lee, K. L. et al. The use of fine needle aspiration and trends in incidence of thyroid cancer in Taiwan. J. Chin. Med. Assoc. 81, 164–169 (2018).
Leenhardt, L. et al. Advances in diagnostic practices affect thyroid cancer incidence in France. Eur. J. Endocrinol. 150, 133–139 (2004).
Cho, Y. J., Kim, D. Y., Park, E. C. & Han, K. T. Thyroid fine-needle aspiration biopsy positively correlates with increased diagnosis of thyroid cancer in South Korean patients. BMC Cancer 17, 114 (2017).
Furuya-Kanamori, L., Bell, K. J. L., Clark, J., Glasziou, P. & Doi, S. A. R. Prevalence of differentiated thyroid cancer in autopsy studies over six decades: a meta-analysis. J. Clin. Oncol. 34, 3672–3679 (2016).
Harach, H. R., Franssila, K. O. & Wasenius, V. M. Occult papillary carcinoma of the thyroid. A “normal” finding in Finland. A systematic autopsy study. Cancer 56, 531–538 (1985).
Moleti, M., Sturniolo, G., Di Mauro, M., Russo, M. & Vermiglio, F. Female reproductive factors and differentiated thyroid cancer. Front. Endocrinol. 8, 111 (2017).
Rahbari, R., Zhang, L. & Kebebew, E. Thyroid cancer gender disparity. Future Oncol. 6, 1771–1779 (2010).
Peterson, E., De, P. & Nuttall, R. BMI, diet and female reproductive factors as risks for thyroid cancer: a systematic review. PLoS One 7, e29177 (2012).
Bertakis, K. D. & Azari, R. Patient gender differences in the prediction of medical expenditures. J. Women’s Health 19, 1925–1932 (2010).
LeClair, K. et al. Evaluation of gender inequity in thyroid cancer diagnosis: differences by sex in US thyroid cancer incidence compared with a meta-analysis of subclinical thyroid cancer rates at autopsy. JAMA Intern. Med. 181, 1351–1358 (2021).
Jegerlehner, S. et al. Overdiagnosis and overtreatment of thyroid cancer: a population-based temporal trend study. PLoS One 12, e0179387 (2017).
Papaleontiou, M., Hughes, D. T., Guo, C., Banerjee, M. & Haymart, M. R. Population-based assessment of complications following surgery for thyroid cancer. J. Clin. Endocrinol. Metab. 102, 2543–2551 (2017).
Lin, J. S., Bowles, E. J. A., Williams, S. B. & Morrison, C. C. Screening for thyroid cancer: updated evidence report and systematic review for the US preventive services task force. JAMA 317, 1888–1903 (2017).
US Preventive Services Task Force Screening for thyroid cancer: US preventive services task force recommendation statement. JAMA 317, 1882–1887 (2017).
Choosing wisely recommendations. American Family Physician https://www.aafp.org/pubs/afp/collections/choosing-wisely/141.html (2025).
Recommendations. Choosing Wisely Australia https://www.choosingwisely.org.au/recommendations/esa1 (2025).
Chen, D. W., Lang, B. H. H., McLeod, D. S. A., Newbold, K. & Haymart, M. R. Thyroid cancer. Lancet 401, 1531–1544 (2023).
Ahn, H. S. & Welch, H. G. South Korea’s thyroid-cancer “epidemic” — turning the tide. N. Engl. J. Med. 373, 2389–2390 (2015).
Kang, E., Ju, H., Kim, S. & Choi, J. Contents analysis of thyroid cancer-related information uploaded to YouTube by physicians in Korea: endorsing thyroid cancer screening, potentially leading to overdiagnosis. BMC Public Health 24, 942 (2024).
Haugen, B. R. et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26, 1–133 (2016).
Yi, K. H. The revised 2016 Korean thyroid association guidelines for thyroid nodules and cancers: differences from the 2015 American Thyroid Association guidelines. Endocrinol. Metab. 31, 373–378 (2016).
Tessler, F. N. et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS committee. J. Am. Coll. Radiol. 14, 587–595 (2017).
Russ, G. et al. European thyroid association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur. Thyroid. J. 6, 225–237 (2017).
Ha, E. J. et al. 2021 Korean thyroid imaging reporting and data system and imaging-based management of thyroid nodules: Korean society of thyroid radiology consensus statement and recommendations. Korean J. Radiol. 22, 2094–2123 (2021).
Dixon, P. R. et al. The role of disease label in patient perceptions and treatment decisions in the setting of low-risk malignant neoplasms. JAMA Oncol. 5, 817–823 (2019).
Nickel, B. et al. Association of preferences for papillary thyroid cancer treatment with disease terminology: a discrete choice experiment. JAMA Otolaryngol. Head. Neck Surg. 144, 887–896 (2018).
Imai, T., Kitano, H., Sugitani, I. & Wada, N. in Treatment of Thyroid Tumor (eds. Takami, H. et al.) 119–122 (Springer, 2013).
Filetti, S. et al. Thyroid cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 30, 1856–1883 (2019).
Sugitani, I. et al. Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: consensus statements from the Japan association of endocrine surgery task force on management for papillary thyroid microcarcinoma. Thyroid 31, 183–192 (2021).
Sawka, A. M. et al. Decision-making in surgery or active surveillance for low risk papillary thyroid cancer during the COVID-19 pandemic. Cancers 13, 371 (2021).
Sawka, A. M. et al. A quantitative analysis examining patients’ choice of active surveillance or surgery for managing low-risk papillary thyroid cancer. Thyroid 32, 255–262 (2022).
Sawka, A. M. et al. A prospective mixed-methods study of decision-making on surgery or active surveillance for low-risk papillary thyroid cancer. Thyroid 30, 999–1007 (2020).
Chou, R. et al. Active surveillance versus thyroid surgery for differentiated thyroid cancer: a systematic review. Thyroid 32, 351–367 (2022).
Perros, P. et al. Guidelines for the management of thyroid cancer. Clin. Endocrinol. 81, 1–122 (2014).
Kandil, E., Krishnan, B., Noureldine, S. I., Yao, L. & Tufano, R. P. Hemithyroidectomy: a meta-analysis of postoperative need for hormone replacement and complications. ORL J. Otorhinolaryngol. Relat. Spec. 75, 6–17 (2013).
Verloop, H. et al. Risk of hypothyroidism following hemithyroidectomy: systematic review and meta-analysis of prognostic studies. J. Clin. Endocrinol. Metab. 97, 2243–2255 (2012).
Haddad, R. I. et al. Thyroid carcinoma, version 2.2022, NCCN clinical practice guidelines in oncology. J. Natl Compr. Cancer Netw. 20, 925–951 (2022).
James, B. C., Timsina, L., Graham, R., Angelos, P. & Haggstrom, D. A. Changes in total thyroidectomy versus thyroid lobectomy for papillary thyroid cancer during the past 15 years. Surgery 166, 41–47 (2019).
Kim, S. K. et al. Total thyroidectomy versus lobectomy in conventional papillary thyroid microcarcinoma: analysis of 8,676 patients at a single institution. Surgery 161, 485–492 (2017).
Colombo, C. et al. Total thyroidectomy versus lobectomy for thyroid cancer: single-center data and literature review. Ann. Surg. Oncol. 28, 4334–4344 (2021).
Rosko, A. J. et al. Surgeons’ attitudes on total thyroidectomy vs lobectomy for management of papillary thyroid microcarcinoma. JAMA Otolaryngol. Head. Neck Surg. 147, 667–669 (2021).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Valeriano Leite and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, D.W., Haymart, M.R. Unravelling the rise in thyroid cancer incidence and addressing overdiagnosis. Nat Rev Endocrinol 22, 10–20 (2026). https://doi.org/10.1038/s41574-025-01168-y
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41574-025-01168-y