Abstract
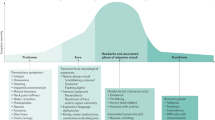
Migraine is a disabling neurological disorder that affects more than one billion people worldwide. The clinical presentation is characterized by recurrent headache attacks, which are often accompanied by photophobia, phonophobia, nausea and vomiting. Although the pathogenesis of migraine remains incompletely understood, mounting evidence suggests that specific signalling molecules are involved in the initiation and modulation of migraine attacks. These signalling molecules include pituitary adenylate cyclase-activating polypeptide (PACAP), a vasoactive peptide that is known to induce migraine attacks when administered by intravenous infusion to people with migraine. Discoveries linking PACAP to migraine pathogenesis have led to the development of drugs that target PACAP signalling, and a phase II trial has provided evidence that a monoclonal antibody against PACAP is effective for migraine prevention. In this Review, we explore the molecular and cellular mechanisms of PACAP signalling, shedding light on its role in the trigeminovascular system and migraine pathogenesis. We then discuss emerging therapeutic strategies that target PACAP signalling for the treatment of migraine and consider the research needed to translate the current knowledge into a treatment for migraine in the clinic.
Key points
-
Pituitary adenylate cyclase-activating polypeptide (PACAP) signalling has been identified as an important pathogenic contributor to migraine, supported by evidence from both animal and human studies.
-
PACAP causes vasodilation and influences immune cell recruitment and activation, which are processes implicated in the pathophysiology of migraine.
-
Intravenous infusion of PACAP can induce migraine attacks in humans, highlighting its direct role in migraine pathogenesis.
-
A monoclonal antibody against PACAP signalling has shown promise in a phase II trial for migraine prevention, indicating potential therapeutic benefits.
-
The complexity of the role that PACAP has in migraine is underscored by its interaction with multiple receptors and the trigeminovascular system; further research is needed to fully understand the therapeutic potential of targeting PACAP signalling.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Stovner, L. J. et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 17, 954–976 (2018).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017).
Ashina, M. Migraine. N. Engl. J. Med. 383, 1866–1876 (2020).
Ashina, M. et al. Migraine and the trigeminovascular system — 40 years and counting. Lancet Neurol. 18, 795–804 (2019).
Ashina, M. et al. Migraine: disease characterisation, biomarkers, and precision medicine. Lancet 397, 1496–1504 (2021).
Al-Hassany, L. et al. Future targets for migraine treatment beyond CGRP. J. Headache Pain 24, 76 (2023).
Vaudry, D. et al. Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol. Rev. 61, 283–357 (2009).
Schytz, H. W. et al. PACAP38 induces migraine-like attacks in patients with migraine without aura. Brain 132, 16–25 (2009).
Ghanizada, H. et al. PACAP27 induces migraine-like attacks in migraine patients. Cephalalgia 40, 57–67 (2020).
Ghanizada, H. et al. Effect of pituitary adenylate cyclase-activating polypeptide-27 on cerebral hemodynamics in healthy volunteers: a 3T MRI study. Peptides 121, 170134 (2019).
Ashina, M. et al. A phase 2, randomized, double-blind, placebo-controlled trial of AMG 301, a pituitary adenylate cyclase-activating polypeptide PAC1 receptor monoclonal antibody for migraine prevention. Cephalalgia 41, 33–44 (2021).
Ashina, M., Phul, R., Khodaie, M., Löf, E. & Florea, I. Monoclonal antibody to pituitary adenylate cyclase-activating peptide for migraine prevention. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2314577 (2024).
Harmar, A. J. et al. International Union of Pharmacology. XVIII. Nomenclature of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide HHS public access. Pharmacol. Rev. 50, 265–270 (1998).
Harmar, A. J. et al. Pharmacology and functions of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide: IUPHAR review 1. Br. J. Pharmacol. 166, 4–17 (2012).
Tasma, Z. et al. Characterisation of agonist signalling profiles and agonist-dependent antagonism at PACAP-responsive receptors: implications for drug discovery. Br. J. Pharmacol. 179, 435–453 (2022).
Alexander, S. P. H. et al. The concise guide to pharmacology 2021/22: G protein-coupled receptors. Br. J. Pharmacol. 178, S27–S156 (2021).
Lu, J. et al. Targeting VIP and PACAP receptor signaling: new insights into designing drugs for the PACAP subfamily of receptors. Int. J. Mol. Sci. 23, 8069 (2022).
Dautzenberg, F. M., Mevenkamp, G., Wille, S. & Hauger, R. L. N-terminal splice variants of the type I PACAP receptor: isolation, characterization and ligand binding/selectivity determinants. J. Neuroendocrinol. 11, 941–949 (1999).
Bonner, T. I. Should pharmacologists care about alternative splicing? IUPHAR review 4. Br. J. Pharmacol. 171, 1231 (2014).
Kotliar, I. B., Lorenzen, E., Schwenk, J. M., Hay, D. L. & Sakmar, T. P. Elucidating the interactome of G protein-coupled receptors and receptor activity-modifying proteins. Pharmacol. Rev. 75, 1–34 (2023).
Dickson, L. & Finlayson, K. VPAC and PAC receptors: from ligands to function. Pharmacol. Ther. 121, 294–316 (2009).
Foster, S. R. et al. Discovery of human signaling systems: pairing peptides to G protein-coupled receptors. Cell 179, 895–908 (2019).
Emery, A. C. & Eiden, L. E. Signaling through the neuropeptide GPCR PAC1 induces neuritogenesis via a single linear cAMP- and ERK-dependent pathway using a novel cAMP sensor. FASEB J. 26, 3199–3211 (2012).
Ravni, A. et al. A cAMP-dependent, protein kinase A-independent signaling pathway mediating neuritogenesis through Egr1 in PC12 cells. Mol. Pharmacol. 73, 1688–1708 (2008).
Stork, P. J. S. & Schmitt, J. M. Crosstalk between cAMP and MAP kinase signaling in the regulation of cell proliferation. Trends Cell Biol. 12, 258–266 (2002).
Guo, S., Jansen-Olesen, I., Olesen, J. & Christensen, S. L. Role of PACAP in migraine: an alternative to CGRP? Neurobiol. Dis. 176, 105946 (2023).
Wootten, D., Christopoulos, A., Marti-Solano, M., Babu, M. M. & Sexton, P. M. Mechanisms of signalling and biased agonism in G protein-coupled receptors. Nat. Rev. Mol. Cell Biol. 19, 638–653 (2018).
Yarwood, R. E. et al. Endosomal signaling of the receptor for calcitonin gene-related peptide mediates pain transmission. Proc. Natl Acad. Sci. USA 114, 12309–12314 (2017).
De Logu, F. et al. Schwann cell endosome CGRP signals elicit periorbital mechanical allodynia in mice. Nat. Commun. 13, 646 (2022).
May, V., Johnson, G. C., Hammack, S. E., Braas, K. M. & Parsons, R. L. PAC1 receptor internalization and endosomal MEK/ERK activation is essential for PACAP-mediated neuronal excitability. J. Mol. Neurosci. 71, 1536–1542 (2021).
Langer, I. Mechanisms involved in VPAC receptors activation and regulation: lessons from pharmacological and mutagenesis studies. Front. Endocrinol. 3, 129 (2012).
Alexander, T. I. et al. Novel fluorescently labeled PACAP and VIP highlight differences between peptide internalization and receptor pharmacology. ACS Pharmacol. Transl. Sci. 6, 52–64 (2023).
Walker, C. S., Sundrum, T. & Hay, D. L. PACAP receptor pharmacology and agonist bias: analysis in primary neurons and glia from the trigeminal ganglia and transfected cells. Br. J. Pharmacol. 171, 1521–1533 (2014).
Tasma, Z., Wills, P., Hay, D. L., Walker, C. S. & Christopher Walker, C. S. Agonist bias and agonist-dependent antagonism at corticotrophin releasing factor receptors. Pharmacol. Res. Perspect. 8, e00595 (2020).
Noseda, R. & Burstein, R. Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain 154, S44–S53 (2013).
Hoffmann, J., Baca, S. M. & Akerman, S. Neurovascular mechanisms of migraine and cluster headache. J. Cereb. Blood Flow Metab. 39, 573–594 (2017).
Akerman, S., Holland, P. R. & Goadsby, P. J. Diencephalic and brainstem mechanisms in migraine. Nat. Rev. Neurosci. 12, 570–584 (2011).
Goadsby, P. J. et al. Pathophysiology of migraine: a disorder of sensory processing. Physiol. Rev. 97, 553–622 (2017).
Julius, D. & Basbaum, A. I. Molecular mechanisms of nociception. Nature 413, 203–210 (2001).
Basbaum, A. I., Bautista, D. M., Scherrer, G. & Julius, D. Cellular and molecular mechanisms of pain. Cell 139, 267–284 (2009).
Zhang, Y. Z., Sjo, B., Moller, K., Håkanson, R. & Sundler, F. Pituitary adenylate cyclase activating peptide produces a marked and long-lasting depression of a C-fibre-evoked flexion reflex. Neuroscience 57, 733–737 (1993).
Uddman, R., Tajti, J., Möller, S., Sundler, F. & Edvinsson, L. Neuronal messengers and peptide receptors in the human sphenopalatine and otic ganglia. Brain Res. 826, 193–199 (1999).
Moller, K. et al. Pituitary adenylate cyclase activating peptide is a sensory neuropeptide: immunocytochemical and immunochemical evidence. Neuroscience 57, 725–732 (1993).
Chan, K. Y. et al. Pharmacological characterization of VIP and PACAP receptors in the human meningeal and coronary artery. Cephalalgia 31, 181–189 (2011).
Hou, M., Uddman, R., Tajti, J. & Edvinsson, L. Nociceptin immunoreactivity and receptor mRNA in the human trigeminal ganglion. Brain Res. 964, 179–186 (2003).
Boni, L., Ploug, K., Olesen, J., Jansen-Olesen, I. & Gupta, S. The in vivo effect of VIP, PACAP-38 and PACAP-27 and mRNA expression of their receptors in rat middle meningeal artery. Cephalalgia 29, 837–847 (2009).
Hirabayashi, T., Nakamachi, T. & Shioda, S. Discovery of PACAP and its receptors in the brain. J. Headache Pain 19, 1–8 (2018).
Akerman, S. & Goadsby, P. J. Neuronal PAC1 receptors mediate delayed activation and sensitization of trigeminocervical neurons: relevance to migraine. Sci. Transl. Med. 7, 308ra157 (2015).
Bruch, L. et al. Pituitary adenylate-cyclase-activating peptides relax human coronary arteries by activating K(ATP) and K(Ca) channels in smooth muscle cells. J. Vasc. Res. 34, 11–18 (1997).
Nelson, M. T. & Quayle, J. M. Physiological roles and properties of potassium channels in arterial smooth muscle. Am. J. Physiol. 268, 799–822 (1995).
Alexander, S. P. H. et al. Class A orphans in GtoPdb v.2023.1. IUPHAR/BPS Guide Pharmacol. https://doi.org/10.2218/GTOPDB/F16/2023.1 (2023).
Pedersen, S. H. et al. PACAP-38 and PACAP(6–38) degranulate rat meningeal mast cells via the orphan MrgB3-receptor. Front. Cell. Neurosci. 13, 1–11 (2019).
Krabbe, A. A. & Olesen, J. Headache provocation by continuous intravenous infusion of histamine. Clinical results and receptor mechanisms. Pain 8, 253–259 (1980).
Akerman, S., Williamson, D. J., Kaube, H. & Goadsby, P. J. The role of histamine in dural vessel dilation. Brain Res. 956, 96–102 (2002).
Levy, D., Burstein, R., Kainz, V., Jakubowski, M. & Strassman, A. M. Mast cell degranulation activates a pain pathway underlying migraine headache. Pain 130, 166–176 (2007).
Bhatt, D. K., Gupta, S., Olesen, J. & Jansen-Olesen, I. PACAP-38 infusion causes sustained vasodilation of the middle meningeal artery in the rat: possible involvement of mast cells. Cephalalgia 34, 877–886 (2014).
Hoffmann, J. et al. PAC1 receptor blockade reduces central nociceptive activity: new approach for primary headache? Pain 161, 1670–1681 (2020).
Kuburas, A. et al. PACAP induces light aversion in mice by an inheritable mechanism independent of CGRP. J. Neurosci. 41, 4697–4715 (2021).
Zhang, L., Zhou, Y., Yang, L., Wang, Y. & Xiao, Z. PACAP6-38 improves nitroglycerin-induced central sensitization by modulating synaptic plasticity at the trigeminal nucleus caudalis in a male rat model of chronic migraine. J. Headache Pain 24, 66 (2023).
Kuburas, A. & Russo, A. F. Shared and independent roles of CGRP and PACAP in migraine pathophysiology. J. Headache Pain 24, 34 (2023).
Ernstsen, C. et al. The PACAP pathway is independent of CGRP in mouse models of migraine: possible new drug target? Brain 145, 2450–2460 (2022).
Tuka, B. et al. Alterations in PACAP-38-like immunoreactivity in the plasma during ictal and interictal periods of migraine patients. Cephalalgia 33, 1085–1095 (2013).
Liu, J., Wang, G., Dan, Y. & Liu, X. CGRP and PACAP-38 play an important role in diagnosing pediatric migraine. J. Headache Pain 23, 1–13 (2022).
Cernuda-Morollón, E. et al. No change in interictal PACAP levels in peripheral blood in women with chronic migraine. Headache 56, 1448–1454 (2016).
Birk, S. et al. The effect of intravenous PACAP38 on cerebral hemodynamics in healthy volunteers. Regul. Pept. 140, 185–191 (2007).
Rasmussen, N. B. et al. The effect of Lu AG09222 on PACAP38- and VIP-induced vasodilation, heart rate increase, and headache in healthy subjects: an interventional, randomized, double-blind, parallel-group, placebo-controlled study. J. Headache Pain 24, 60 (2023).
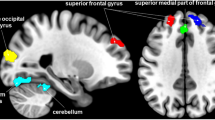
Amin, F. M. et al. Change in brain network connectivity during PACAP38-induced migraine attacks: a resting-state functional MRI study. Neurology 86, 180–187 (2016).
Guo, S., Vollesen, A. L. H., Olesen, J. & Ashina, M. Premonitory and nonheadache symptoms induced by CGRP and PACAP38 in patients with migraine. Pain 157, 2773–2781 (2016).
Katarina Frifelt Wienholtz, N. et al. Early treatment with sumatriptan prevents PACAP38-induced migraine: a randomised clinical trial. Cephalalgia 41, 731–748 (2021).
Vollesen, L. H., Guo, S., Andersen, M. R. & Ashina, M. Effect of the H1-antihistamine clemastine on PACAP38 induced migraine. Cephalalgia 39, 597–607 (2019).
Amin, F. M. et al. Investigation of the pathophysiological mechanisms of migraine attacks induced by pituitary adenylate cyclase-activating polypeptide-38. Brain 137, 779–794 (2014).
Rahmann, A. et al. Vasoactive intestinal peptide causes marked cephalic vasodilation, but does not induce migraine. Cephalalgia 28, 226–236 (2008).
Pellesi, L. et al. Effect of vasoactive intestinal polypeptide on development of migraine headaches: a randomized clinical trial. JAMA Netw. Open 4, e2118543 (2021).
Bourgault, S. et al. Novel stable PACAP analogs with potent activity towards the PAC1 receptor. Peptides 29, 919–932 (2008).
Baun, M., Pedersen, M. H. F., Olesen, J. & Jansen-Olesen, I. Dural mast cell degranulation is a putative mechanism for headache induced by PACAP-38. Cephalalgia 32, 337–345 (2012).
Lassen, L. H., Thomsen, L. L. & Olesen, J. Histamine induces migraine via the H1-receptor. Support for the NO hypothesis of migraine. Neuroreport 6, 1475–1479 (1995).
Banks, W. A., Kastin, A. J., Komaki, G. & Arimura, A. Passage of pituitary adenylate cyclase activating polypeptide 1–27 and pituitary adenylate cyclase activating polypeptide 1–38 across the blood–brain barrier. J. Pharmacol. Exp. Ther. 267, 690–696 (1993).
Guo, S. et al. Part I: pituitary adenylate cyclase-activating polypeptide-38 induced migraine-like attacks in patients with and without familial aggregation of migraine. Cephalalgia 37, 125–135 (2016).
Reglodi, D., Vaczy, A., Rubio-Beltran, E. & Maassen Van Den Brink, A. Protective effects of PACAP in ischemia. J. Headache Pain 19, 1–9 (2018).
Toth, D. et al. Protective effects of PACAP in peripheral organs. Front. Endocrinol. 11, 377 (2020).
Toth, D., Reglodi, D., Schwieters, L. & Tamas, A. Role of endocrine PACAP in age-related diseases. Front. Endocrinol. 14, 1118927 (2023).
Langer, I., Jeandriens, J., Couvineau, A., Sanmukh, S. & Latek, D. Signal transduction by VIP and PACAP receptors. Biomedicines 10, 406 (2022).
Reglodi, D. et al. PACAP deficiency as a model of aging. Geroscience 40, 437–452 (2018).
Stroth, N., Holighaus, Y., Ait-Ali, D. & Eiden, L. E. PACAP: a master regulator of neuroendocrine stress circuits and the cellular stress response. Ann. N. Y. Acad. Sci. 1220, 49–59 (2011).
Zhang, L. et al. Behavioral role of PACAP signaling reflects its selective distribution in glutamatergic and GABAergic neuronal subpopulations. eLife 10, 1–77 (2021).
Holland, P. R., Barloese, M. & Fahrenkrug, J. PACAP in hypothalamic regulation of sleep and circadian rhythm: importance for headache. J. Headache Pain 19, 20 (2018).
Uddman, R., Tajti, J., Hou, M., Sundler, F. & Edvinsson, L. Neuropeptide expression in the human trigeminal nucleus caudalis and in the cervical spinal cord C1 and C2. Cephalalgia 22, 112–116 (2002).
Tajti, J., Uddman, R. & Edvinsson, L. Neuropeptide localization in the ‘migraine generator’ region of the human brainstem. Cephalalgia 21, 96–101 (2001).
Sundrum, T. & Walker, C. S. Pituitary adenylate cyclase-activating polypeptide receptors in the trigeminovascular system: implications for migraine. Br. J. Pharmacol. 175, 4109–4120 (2018).
Mitsikostas, D. D. et al. The 5-HT1F receptor as the target of ditans in migraine — from bench to bedside. Nat. Rev. Neurol. 19, 489–505 (2023).
Pearlman, E. M. et al. Effects of lasmiditan on simulated driving performance: results of two randomized, blinded, crossover studies with placebo and active controls. Hum. Psychopharmacol. 35, e2732 (2020).
Zuchero, Y. J. Y. et al. Discovery of novel blood–brain barrier targets to enhance brain uptake of therapeutic antibodies. Neuron 89, 70–82 (2016).
Charles, A. & Pozo-Rosich, P. Targeting calcitonin gene-related peptide: a new era in migraine therapy. Lancet 394, 1765–1774 (2019).
Vollesen, A. L. H. et al. The effect of pituitary adenylate cyclase-activating peptide-38 and vasoactive intestinal peptide in cluster headache. Cephalalgia 40, 1474–1488 (2020).
Bertels, Z. et al. PACAP–PAC1 receptor inhibition is effective in opioid induced hyperalgesia and medication overuse headache models. iScience 26, 105950 (2023).
Al-Khazali, H. M. et al. Hypersensitivity to PACAP-38 in post-traumatic headache: a randomized clinical trial. Brain 147, 1312–1320 (2024).
Miyata, A. et al. Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem. Biophys. Res. Commun. 164, 567–574 (1989).
Miyata, A. et al. Isolation of a neuropeptide corresponding to the N-terminal 27 residues of the pituitary adenylate cyclase activating polypeptide with 38 residues (PACAP38). Biochem. Biophys. Res. Commun. 170, 643–648 (1990).
Pisegna, J. R. & Wank, S. A. Molecular cloning and functional expression of the pituitary adenylate cyclase-activating polypeptide type I receptor. Proc. Natl Acad. Sci. USA 90, 6345 (1993).
Lutz, E. M. et al. The VIP2 receptor: molecular characterisation of a cDNA encoding a novel receptor for vasoactive intestinal peptide. FEBS Lett. 334, 3–8 (1993).
Usdin, T. B., Bonner, T. I. & Mezey, E. Two receptors for vasoactive intestinal polypeptide with similar specificity and complementary distributions. Endocrinology 135, 2662–2680 (1994).
Zagami, A. S., Edvinsson, L. & Goadsby, P. J. Pituitary adenylate cyclase activating polypeptide and migraine. Ann. Clin. Transl. Neurol. 1, 1036–1040 (2014).
Han, X. et al. Interictal plasma pituitary adenylate cyclase-activating polypeptide levels are decreased in migraineurs but remain unchanged in patients with tension-type headache. Clin. Chim. Acta 450, 151–154 (2015).
Pérez-Pereda, S. et al. Serum CGRP, VIP, and PACAP usefulness in migraine: a case–control study in chronic migraine patients in real clinical practice. Mol. Biol. Rep. 47, 7125–7138 (2020).
Author information
Authors and Affiliations
Contributions
H.A., R.H.C. and M.A. researched data for the article and contributed to writing of the article. All authors contributed substantially to discussion of the content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
H.A. has received personal fees from AbbVie, Lundbeck, Pfizer and Teva that are unrelated to this manuscript. D.L.H. has received research support from AbbVie and Pfizer and has acted as an adviser, speaker or consultant for AbbVie, Amgen, Eli Lilly, Merck, Nxera Pharma and Teva. D.L.H. also receives funding from the NIH (RF1 NS113839). The contents of this manuscript do not represent the views of the US Government. At the time of drafting and submitting this manuscript, J.H. was employed as an academic researcher at King’s College London, UK. Since 1st May 2024, he has been employed by H. Lundbeck A/S; since this time, he has approved the manuscript but has made no changes. Prior to his employment at H. Lundbeck A/S, J.H. received honoraria for consulting activities and/or serving on advisory boards and/or as a speaker from AbbVie, Allergan, Autonomic Technologies, Cannovex, Chordate Medical, Eli Lilly, Hormosan Pharma, H. Lundbeck A/S, MD-Horizonte, Novartis, Pfizer, Sanofi and Teva. He has received personal fees for Medico-Legal work and from NEJM Journal Watch, Oxford University Press, Quintessence Publishing, Sage Publishing and Springer Healthcare. He holds stock options from Chordate Medical. He has also received research grants from Bristol Myers Squibb, the National Institute for Health and Care Research (NIHR), the Medical Research Council (MRC), the International Headache Society (IHS) and the Migraine Trust. He serves or has served as Associate Editor for Cephalalgia, Cephalalgia Reports, Frontiers in Pain Research, Journal of Headache and Facial Pain and Journal of Oral & Facial Pain. He has been an elected member of the Board of Trustees as well as the Science and Research Committee of the IHS as well as a Council Member and Treasurer of the British Association for the Study of Headache. A.F.R. has received personal fees from AbbVie, Amgen, Eli Lilly, Lundbeck, Novartis, Paragon and Schedule One Pharmaceuticals unrelated to this manuscript. A.F.R. receives funding from the NIH (R01 NS075599, RF1 NS113839 and R01 NS129573), Veterans Administration (IO1 RX003523) and Pfizer. The contents of the manuscript do not represent the views of the Veterans Administration or the US Government. M.A. has received personal fees from AbbVie, Amgen, Astra Zeneca, Eli Lilly, Escient, GlaxoSmithKline, Lundbeck, Novartis, Pfizer and Teva Pharmaceuticals unrelated to this manuscript. M.A. also serves as an associate editor of Brain and The Journal of Headache and Pain. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks L. Edvinsson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ashina, H., Christensen, R.H., Hay, D.L. et al. Pituitary adenylate cyclase-activating polypeptide signalling as a therapeutic target in migraine. Nat Rev Neurol 20, 660–670 (2024). https://doi.org/10.1038/s41582-024-01011-4
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41582-024-01011-4
This article is cited by
-
Migraine in men
The Journal of Headache and Pain (2025)
-
PACAP38-induced migraine attacks are independent of CGRP signaling: a randomized controlled trial
The Journal of Headache and Pain (2025)
-
Revisiting substance P in migraine: a methodological approach inspired by anti-CGRP and anti-PACAP success
The Journal of Headache and Pain (2025)
-
Sex difference in TRPM3 channel functioning in nociceptive and vascular systems: an emerging target for migraine therapy in females?
The Journal of Headache and Pain (2025)
-
Mechanistic intersections between migraine and major depressive disorder
The Journal of Headache and Pain (2025)