Abstract
Friedreich ataxia (FRDA) is a rare multisystem, life-limiting disease and is the most common early-onset inherited ataxia in populations of European, Arab and Indian descent. In recent years, substantial progress has been made in dissecting the pathogenesis and natural history of FRDA, and several clinical trials have been initiated. A particularly notable recent achievement was the approval of the nuclear factor erythroid 2-related factor 2 activator omaveloxolone as the first disease-specific therapy for FRDA. In light of these developments, we review milestones in FRDA translational and clinical research over the past 10 years, as well as the various therapeutic strategies currently in the pipeline. We also consider the lessons that have been learned from failed trials and other setbacks. We conclude by presenting a global roadmap for future research, as outlined by the recently established Friedreich’s Ataxia Global Clinical Consortium, which covers North and South America, Europe, India, Australia and New Zealand.
Key points
-
Basic and clinical research in Friedreich ataxia (FRDA) has advanced at a fast pace, with milestones being achieved in elucidating the function of frataxin and characterizing the natural history of the disease.
-
The NRF2 activator omaveloxolone was approved as the first specific therapy for FRDA by the FDA in 2023 and the European Commission in 2024.
-
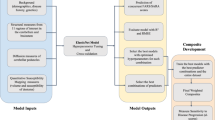
Gene therapies, agents that modulate frataxin gene expression and direct frataxin replacement strategies have also entered clinical trials.
-
The recently formed Friedreich’s Ataxia Global Clinical Consortium (FA GCC) has launched the first global natural history study to harmonize and promote clinical research in FRDA worldwide.
-
The need for more sensitive outcome measures at different stages of the disease and the characterization of cardiac evolution are among the open questions to be addressed by the global consortium.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Labuda, M. et al. Unique origin and specific ethnic distribution of the Friedreich ataxia GAA expansion. Neurology 54, 2322–2324 (2000).
Vankan, P. Prevalence gradients of Friedreich’s ataxia and R1b haplotype in Europe co-localize, suggesting a common Palaeolithic origin in the Franco-Cantabrian ice age refuge. J. Neurochem. 126, 11–20 (2013).
Koeppen, A. H. Nikolaus Friedreich and degenerative atrophy of the dorsal columns of the spinal cord. J. Neurochem. 126, 4–10 (2013).
Depienne, C. & Mandel, J. L. 30 years of repeat expansion disorders: what have we learned and what are the remaining challenges? Am. J. Hum. Genet. 108, 764–785 (2021).
Maio, N. & Rouault, T. A. Mammalian iron sulfur cluster biogenesis and human diseases. IUBMB Life 74, 705 (2022).
Boesch, S. & Indelicato, E. Approval of omaveloxolone for Friedreich ataxia. Nat. Rev. Neurol. 20, 313–314 (2024).
Campuzano, V. et al. Friedreich’s ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science 271, 1423–1427 (1996).
Savellev, A., Everett, C., Sharpe, T., Webster, Z. & Festenstein, R. DNA triplet repeats mediate heterochromatin-protein-1-sensitive variegated gene silencing. Nature 422, 909–913 (2003).
Herman, D. et al. Histone deacetylase inhibitors reverse gene silencing in Friedreich’s ataxia. Nat. Chem. Biol. 2, 551–558 (2006).
Rodden, L. N. et al. Methylated and unmethylated epialleles support variegated epigenetic silencing in Friedreich ataxia. Hum. Mol. Genet. 29, 3818–3829 (2020).
Campuzano, V. et al. Frataxin is reduced in Friedreich ataxia patients and is associated with mitochondrial membranes. Hum. Mol. Genet. 6, 1771–1780 (1997).
Galea, C. A. et al. Compound heterozygous FXN mutations and clinical outcome in Friedreich ataxia. Ann. Neurol. 79, 485–495 (2016).
Shen, M. M., Rummey, C. & Lynch, D. R. Phenotypic variation of FXN compound heterozygotes in a Friedreich ataxia cohort. Ann. Clin. Transl. Neurol. 11, 1110–1121 (2024).
Candayan, A. et al. The first biallelic missense mutation in the FXN gene in a consanguineous Turkish family with Charcot-Marie-Tooth-like phenotype. Neurogenetics 21, 73–78 (2020).
Cossée, M. et al. Inactivation of the Friedreich ataxia mouse gene leads to early embryonic lethality without iron accumulation. Hum. Mol. Genet. 9, 1219–1226 (2000).
Rummey, C. et al. Natural history of Friedreich ataxia: heterogeneity of neurologic progression and consequences for clinical trial design. Neurology 99, E1499–E1510 (2022).
Indelicato, E. et al. Onset features and time to diagnosis in Friedreich’s ataxia. Orphanet J. Rare Dis. 15, 198 (2020).
Parkinson, M. H., Boesch, S., Nachbauer, W., Mariotti, C. & Giunti, P. Clinical features of Friedreich’s ataxia: classical and atypical phenotypes. J. Neurochem. 126, 103–117 (2013).
Fahey, M. C. et al. Vestibular, saccadic and fixation abnormalities in genetically confirmed Friedreich ataxia. Brain 131, 1035–1045 (2008).
Spicker, S. et al. Fixation instability and oculomotor abnormalities in Friedreich’s ataxia. J. Neurol. 242, 517–521 (1995).
Patel, M. et al. Body mass index and height in the Friedreich Ataxia Clinical Outcome Measures Study. Neurol. Genet. 7, e638 (2021).
Simon, A. L. et al. Scoliosis in patients with Friedreich ataxia: results of a consecutive prospective series. Spine Deform. 7, 812–821 (2019).
Helliwell, T. R. et al. The pathology of the lower leg muscles in pure forefoot pes cavus. Acta Neuropathol. 89, 552–559 (1995).
Tamaroff, J. et al. Friedreich’s ataxia related diabetes: epidemiology and management practices. Diabetes Res. Clin. Pract. 186, 109828 (2022).
Fichera, M. et al. Comorbidities in Friedreich ataxia: incidence and manifestations from early to advanced disease stages. Neurol. Sci. 43, 6831–6838 (2022).
Cnop, M., Mulder, H. & Igoillo-Esteve, M. Diabetes in Friedreich ataxia. J. Neurochem. 126, 94–102 (2013).
Dürr, A. et al. Clinical and genetic abnormalities in patients with Friedreich’s ataxia. N. Engl. J. Med. 335, 1169–1175 (1996).
Reetz, K. et al. Biological and clinical characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS) cohort: a cross-sectional analysis of baseline data. Lancet Neurol. 14, 174–182 (2015).
Patel, M. et al. Progression of Friedreich ataxia: quantitative characterization over 5 years. Ann. Clin. Transl. Neurol. 3, 684–694 (2016).
Reetz, K. et al. Progression characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS): a 2 year cohort study. Lancet Neurol. 15, 1346–1354 (2016).
Rummey, C., Farmer, J. M. & Lynch, D. R. Predictors of loss of ambulation in Friedreich’s ataxia. EClinicalMedicine 18, 100213 (2020).
Sharma, R. et al. Friedreich ataxia in carriers of unstable borderline GAA triplet-repeat alleles. Ann. Neurol. 56, 898–901 (2004).
Ragno, M. et al. Broadened Friedreich’s ataxia phenotype after gene cloning: minimal GAA expansion causes late-onset spastic ataxia. Neurology 49, 1617–1620 (1997).
Indelicato, E. et al. Predictors of survival in Friedreich’s ataxia: a prospective cohort study. Mov. Disord. 39, 510–518 (2024).
Epplen, C. et al. Differential stability of the (GAA)n tract in the Friedreich ataxia (STM7) gene. Hum. Genet. 99, 834–836 (1997).
Tai, G., Yiu, E. M., Corben, L. A. & Delatycki, M. B. A longitudinal study of the Friedreich ataxia impact scale. J. Neurol. Sci. 352, 53–57 (2015).
Brandsma, R. et al. A clinical diagnostic algorithm for early onset cerebellar ataxia. Eur. J. Paediatr. Neurol. 23, 692–706 (2019).
Van de Warrenburg, B. P. C. et al. EFNS/ENS consensus on the diagnosis and management of chronic ataxias in adulthood. Eur. J. Neurol. 21, 552–562 (2014).
Fleszar, Z. et al. Short-read genome sequencing allows ‘en route’ diagnosis of patients with atypical Friedreich ataxia. J. Neurol. 270, 4112–4117 (2023).
Uppili, B. et al. Sequencing through hyperexpanded Friedreich’s ataxia-GAA repeats by nanopore technology: implications in genotype-phenotype correlation. Brain Commun. 5, fcad020 (2023).
Bidichandani, S. I., Ashizawa, T. & Patel, P. I. The GAA triplet-repeat expansion in Friedreich ataxia interferes with transcription and may be associated with an unusual DNA structure. Am. J. Hum. Genet. 62, 111–121 (1998).
Ohshima, K., Montermini, L., Wells, R. D. & Pandolfo, M. Inhibitory effects of expanded GAA·TTC triplet repeats from intron I of the Friedreich ataxia gene on transcription and replication in vivo. J. Biol. Chem. 273, 14588–14595 (1998).
Sakamoto, N. et al. Sticky DNA: self-association properties of long GAA.TTC repeats in R.R.Y triplex structures from Friedreich’s ataxia. Mol. Cell 3, 465–475 (1999).
Soragni, E. et al. Epigenetic therapy for Friedreich ataxia. Ann. Neurol. 76, 489–508 (2014).
Cavadini, P., Adamec, J., Taroni, F., Gakh, O. & Isaya, G. Two-step processing of human frataxin by mitochondrial processing peptidase. Precursor and intermediate forms are cleaved at different rates. J. Biol. Chem. 275, 41469–41475 (2000).
Schmucker, S. et al. Mammalian frataxin: an essential function for cellular viability through an interaction with a preformed ISCU/NFS1/ISD11 iron-sulfur assembly complex. PLoS ONE 6, e16199 (2011).
Pastore, A. & Puccio, H. Frataxin: a protein in search for a function. J. Neurochem. 126, 43–52 (2013).
Babcock, M. et al. Regulation of mitochondrial iron accumulation by Yfh1p, a putative homolog of frataxin. Science 276, 1709–1712 (1997).
Yoon, T. & Cowan, J. A. Iron-sulfur cluster biosynthesis. Characterization of frataxin as an iron donor for assembly of [2Fe-2S] clusters in ISU-type proteins. J. Am. Chem. Soc. 125, 6078–6084 (2003).
Adamec, J. et al. Iron-dependent self-assembly of recombinant yeast frataxin: implications for Friedreich ataxia. Am. J. Hum. Genet. 67, 549–562 (2000).
Rotig, A. et al. Aconitase and mitochondrial iron-sulphur protein deficiency in Friedreich ataxia. Nat. Genet. 17, 215–217 (1997).
Rouault, T. A. & Tong, W. H. Iron-sulfur cluster biogenesis and human disease. Trends Genet. 24, 398–407 (2008).
Fox, N. G. et al. Structure of the human frataxin-bound iron-sulfur cluster assembly complex provides insight into its activation mechanism. Nat. Commun. 10, 2210 (2019).
Schulz, V. et al. Mechanism and structural dynamics of sulfur transfer during de novo [2Fe-2S] cluster assembly on ISCU2. Nat. Commun. 15, 3269 (2024).
Gervason, S. et al. Physiologically relevant reconstitution of iron-sulfur cluster biosynthesis uncovers persulfide-processing functions of ferredoxin-2 and frataxin. Nat. Commun. 10, 3566 (2019).
Uzarska, M. A. et al. During FeS cluster biogenesis, ferredoxin and frataxin use overlapping binding sites on yeast cysteine desulfurase Nfs1. J. Biol. Chem. 298, 101570 (2022).
Steinhilper, R. et al. Two-stage binding of mitochondrial ferredoxin-2 to the core iron-sulfur cluster assembly complex. Nat. Commun. 15, 10559 (2024).
Belbellaa, B., Reutenauer, L., Messaddeq, N., Monassier, L. & Puccio, H. High levels of frataxin overexpression lead to mitochondrial and cardiac toxicity in mouse models. Mol. Ther. Methods Clin. Dev. 19, 120–138 (2020).
Huichalaf, C. et al. In vivo overexpression of frataxin causes toxicity mediated by iron-sulfur cluster deficiency. Mol. Ther. Methods Clin. Dev. 24, 367–378 (2022).
Ast, T. et al. Hypoxia rescues frataxin loss by restoring iron sulfur cluster biogenesis. Cell 177, 1507–1521.e16 (2019).
Puccio, H. et al. Mouse models for Friedreich ataxia exhibit cardiomyopathy, sensory nerve defect and Fe-S enzyme deficiency followed by intramitochondrial iron deposits. Nat. Genet. 27, 181–186 (2001).
González-Cabo, P. & Palau, F. Mitochondrial pathophysiology in Friedreich’s ataxia. J. Neurochem. 126, 53–64 (2013).
Lodi, R. et al. Deficit of in vivo mitochondrial ATP production in patients with Friedreich ataxia. Proc. Natl Acad. Sci. USA 96, 11492–11495 (1999).
Indelicato, E. et al. Skeletal muscle proteome analysis underpins multifaceted mitochondrial dysfunction in Friedreich’s ataxia. Front. Neurosci. 17, 1289027 (2023).
Indelicato, E. et al. Skeletal muscle transcriptomics dissects the pathogenesis of Friedreich’s ataxia. Hum. Mol. Genet. 32, 2241–2250 (2023).
Gurgel-Giannetti, J. et al. A novel complex neurological phenotype due to a homozygous mutation in FDX2. Brain 141, 2289–2298 (2018).
Crooks, D. R. et al. Tissue specificity of a human mitochondrial disease: differentiation-enhanced mis-splicing of the Fe-S scaffold gene ISCU renders patient cells more sensitive to oxidative stress in ISCU myopathy. J. Biol. Chem. 287, 40119–40130 (2012).
Uhlén, M. et al. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Lynch, D. R., Deutsch, E. C., Wilson, R. B. & Tennekoon, G. Unanswered questions in Friedreich ataxia. J. Child. Neurol. 27, 1223–1229 (2012).
De Biase, I. et al. Progressive GAA expansions in dorsal root ganglia of Friedreich’s ataxia patients. Ann. Neurol. 61, 55–60 (2007).
Long, A. et al. Somatic instability of the expanded GAA repeats in Friedreich’s ataxia. PLoS One 12, e0189990 (2017).
Koeppen, A. H., Becker, A. B., Qian, J., Gelman, B. B. & Mazurkiewicz, J. E. Friedreich ataxia: developmental failure of the dorsal root entry zone. J. Neuropathol. Exp. Neurol. 76, 969–977 (2017).
Koeppen, A. H. & Mazurkiewicz, J. E. Friedreich ataxia: neuropathology revised. J. Neuropathol. Exp. Neurol. 72, 78–90 (2013).
Koeppen, A. H., Ramirez, R. L., Becker, A. B. & Mazurkiewicz, J. E. Dorsal root ganglia in Friedreich ataxia: satellite cell proliferation and inflammation. Acta Neuropathol. Commun. 4, 46 (2016).
Harding, I. H. et al. Brain structure and degeneration staging in Friedreich ataxia: magnetic resonance imaging volumetrics from the ENIGMA-Ataxia working group. Ann. Neurol. 90, 570–583 (2021).
Martínez, A. C. & Anciones, B. Central motor conduction to upper and lower limbs after magnetic stimulation of the brain and peripheral nerve abnormalities in 20 patients with Friedreich’s ataxia. Acta Neurol. Scand. 85, 323–326 (1992).
Caruso, G. et al. Friedreich’s ataxia: electrophysiological and histological findings. Acta Neurol. Scand. 67, 26–40 (1983).
Rezende, T. J. R. et al. Progressive spinal cord degeneration in Friedreich’s ataxia: results from ENIGMA-Ataxia. Mov. Disord. 38, 45–56 (2023).
Joers, J. M. et al. Spinal cord magnetic resonance imaging and spectroscopy detect early-stage alterations and disease progression in Friedreich ataxia. Brain Commun. 4, fcac246 (2022).
Rezende, T. J. R. et al. Developmental and neurodegenerative damage in Friedreich’s ataxia. Eur. J. Neurol. 26, 483–489 (2019).
Ward, P. G. D. et al. Longitudinal evaluation of iron concentration and atrophy in the dentate nuclei in Friedreich ataxia. Mov. Disord. 34, 335–343 (2019).
Adanyeguh, I. M. et al. Brain MRI detects early-stage alterations and disease progression in Friedreich ataxia. Brain Commun. 5, fcad19 (2023).
Tsou, A. Y. et al. Mortality in Friedreich ataxia. J. Neurol. Sci. 307, 46–49 (2011).
Koeppen, A. H. et al. The pathogenesis of cardiomyopathy in Friedreich ataxia. PLoS ONE 10, e0116396 (2015).
Eigentler, A., Boesch, S., Schneider, R., Dechant, G. & Nat, R. Induced pluripotent stem cells from Friedreich ataxia patients fail to upregulate frataxin during in vitro differentiation to peripheral sensory neurons. Stem Cell Dev. 22, 3271–3282 (2013).
Dionisi, C. et al. Proprioceptors-enriched neuronal cultures from induced pluripotent stem cells from Friedreich ataxia patients show altered transcriptomic and proteomic profiles, abnormal neurite extension, and impaired electrophysiological properties. Brain Commun. 5, fcad007 (2023).
Lai, J. I. et al. Transcriptional profiling of isogenic Friedreich ataxia neurons and effect of an HDAC inhibitor on disease signatures. J. Biol. Chem. 294, 1846–1859 (2019).
Boesch, S. & Indelicato, E. Experimental drugs for Friedrich’s ataxia: progress and setbacks in clinical trials. Expert. Opin. Invest. Drugs 32, 967–969 (2023).
Perdomini, M., Hick, A., Puccio, H. & Pook, M. A. Animal and cellular models of Friedreich ataxia. J. Neurochem. 126, 65–79 (2013).
Rai, M. et al. HDAC inhibitors correct frataxin deficiency in a Friedreich ataxia mouse model. PLoS ONE 3, e1958 (2008).
Piguet, F. et al. Rapid and complete reversal of sensory ataxia by gene therapy in a novel model of Friedreich ataxia. Mol. Ther. 26, 1940–1952 (2018).
Perdomini, M. et al. Prevention and reversal of severe mitochondrial cardiomyopathy by gene therapy in a mouse model of Friedreich’s ataxia. Nat. Med. 20, 542–547 (2014).
Salami, C. O. et al. Stress-induced mouse model of the cardiac manifestations of Friedreich’s ataxia corrected by AAV-mediated gene therapy. Hum. Gene Ther. 31, 819–827 (2020).
Sivakumar, A. & Cherqui, S. Advantages and limitations of gene therapy and gene editing for Friedreich’s ataxia. Front. Genome Ed. 4, 903139 (2022).
Li, Y. et al. Excision of expanded GAA repeats alleviates the molecular phenotype of Friedreich’s ataxia. Mol. Ther. 23, 1055–1065 (2015).
Li, J. et al. Excision of the expanded GAA repeats corrects cardiomyopathy phenotypes of iPSC-derived Friedreich’s ataxia cardiomyocytes. Stem Cell Res. 40, 101529 (2019).
Mishra, P. et al. Gene editing improves endoplasmic reticulum-mitochondrial contacts and unfolded protein response in Friedreich’s ataxia iPSC-derived neurons. Front. Pharmacol. 15, 1323491 (2024).
Mazzara, P. G. et al. Frataxin gene editing rescues Friedreich’s ataxia pathology in dorsal root ganglia organoid-derived sensory neurons. Nat. Commun. 11, 4178 (2020).
Rocca, C. J. et al. Transplantation of wild-type mouse hematopoietic stem and progenitor cells ameliorates deficits in a mouse model of Friedreich’s ataxia. Sci. Transl. Med. 9, eaaj2347 (2017).
Reetz, K. et al. Progression characteristics of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS): a 4-year cohort study. Lancet. Neurol. 20, 362–372 (2021).
Subramony, S. H. et al. Measuring Friedreich ataxia: interrater reliability of a neurologic rating scale. Neurology 64, 1261–1262 (2005).
Schmitz-Hübsch, T. et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66, 1717–1720 (2006).
Rummey, C. et al. Psychometric properties of the Friedreich ataxia rating scale. Neurol. Genet. 5, 371 (2019).
Lynch, D. R. et al. Safety and efficacy of omaveloxolone in Friedreich ataxia (MOXIe Study). Ann. Neurol. 89, 212–225 (2021).
Lynch, D. R. et al. Propensity matched comparison of omaveloxolone treatment to Friedreich ataxia natural history data. Ann. Clin. Transl. Neurol. 11, 4–16 (2024).
Center for Drug Evaluation and Research. Clinical review(s). Application number: 216718Orig1s000. CDER https://www.accessdata.fda.gov/drugsatfda_docs/nda/2023/216718Orig1s000MedR.pdf (2023).
Gunther, K. & Lynch, D. R. Pharmacotherapeutic strategies for Friedreich ataxia: a review of the available data. Expert. Opin. Pharmacother. 25, 529–539 (2024).
Abeysekara, L. L. et al. A novel feature from instrumented utensils for clinical assessment of Friedreich ataxia. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2023, 1–4 (2023).
Corben, L. A. et al. Developing an instrumented measure of upper limb function in Friedreich ataxia. Cerebellum 20, 430–438 (2021).
Kadirvelu, B. et al. A wearable motion capture suit and machine learning predict disease progression in Friedreich’s ataxia. Nat. Med. 29, 86–94 (2023).
Németh, A. H. et al. Using smartphone sensors for ataxia trials: consensus guidance by the Ataxia Global Initiative Working Group on Digital-Motor Biomarkers. Cerebellum 23, 912–923 (2024).
Center for Drug Evaluation and Research. Patient-focused drug development: collecting comprehensive and representative input. FDA https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-collecting-comprehensive-and-representative-input (2020).
Tai, G., Corben, L. A., Yiu, E. M. & Delatycki, M. B. A longitudinal study of the SF-36 version 2 in Friedreich ataxia. Acta Neurol. Scand. 136, 41–46 (2017).
Seabury, J. et al. Friedreich’s ataxia-health index: development and validation of a novel disease-specific patient-reported outcome measure. Neurol. Clin. Pract. 13, e200180 (2023).
Seabury, J. et al. Friedreich Ataxia Caregiver-Reported Health Index: development of a novel, disease-specific caregiver-reported outcome measure. Neurol. Clin. Pract. 14, e200303 (2024).
Payne, R. M. Cardiovascular research in Friedreich ataxia: unmet needs and opportunities. JACC Basic. Transl. Sci. 7, 1267–1283 (2022).
Weidemann, F. et al. The heart in Friedreich ataxia: definition of cardiomyopathy, disease severity, and correlation with neurological symptoms. Circulation 125, 1626–1634 (2012).
Takazaki, K. A. G. et al. Pre-clinical left ventricular myocardial remodeling in patients with Friedreich’s ataxia: a cardiac MRI study. PLoS ONE 16, e0246633 (2021).
Hutchens, J. A., Johnson, T. R. & Payne, R. M. Myocardial perfusion reserve in children with Friedreich ataxia. Pediatr. Cardiol. 42, 1834–1840 (1234).
Pousset, F. et al. A 22-year follow-up study of long-term cardiac outcome and predictors of survival in Friedreich ataxia. JAMA Neurol. 72, 1334–1341 (2015).
Hewer, R. L. Study of fatal cases of Friedreich’s ataxia. Br. Med. J. 3, 649 (1968).
Mejia, E. et al. Ectopic burden via Holter monitors in Friedreich’s ataxia. Pediatr. Neurol. 117, 29 (2021).
Weidemann, F. et al. The cardiomyopathy in Friedreich’s ataxia – new biomarker for staging cardiac involvement. Int. J. Cardiol. 194, 50–57 (2015).
Indelicato, E. & Bösch, S. Emerging therapeutics for the treatment of Friedreich’s ataxia. Expert Opin. Orphan Drugs 6, 57–67 (2018).
Libri, V. et al. Epigenetic and neurological effects and safety of high-dose nicotinamide in patients with Friedreich’s ataxia: an exploratory, open-label, dose-escalation study. Lancet 384, 504–513 (2014).
Boesch, S. & Indelicato, E. Erythropoietin and Friedreich ataxia: time for a reappraisal? Front. Neurosci. 13, 386 (2019).
Gottesfeld, J. M. Molecular mechanisms and therapeutics for the GAA·TTC expansion disease Friedreich ataxia. Neurotherapeutics 16, 1032–1049 (2019).
Trantham, S. J. et al. Perspectives of the Friedreich ataxia community on gene therapy clinical trials. Mol. Ther. Methods Clin. Dev. 32, 101179 (2024).
Design Therapeutics. Design Therapeutics reports initial results from phase 1 multiple-ascending dose study of DT-216 for the treatment of Friedreich ataxia. Design Therapeutics https://investors.designtx.com/news-releases/news-release-details/design-therapeutics-reports-initial-results-phase-1-multiple (2023).
Clayton, R. et al. Safety, pharmacokinetics, and pharmacodynamics of nomlabofusp (CTI‐1601) in Friedreich’s ataxia. Ann. Clin. Transl. Neurol. 11, 540 (2024).
Larimar Therapeutics. Larimar Therapeutics: corporate deck (June 2024). Larimar Therapeutics https://investors.larimartx.com/static-files/6aaf56f2-3c60-4164-a7ea-865cdb0ae356 (2024).
Reisman, S. A. et al. Pharmacokinetics and pharmacodynamics of the novel NrF2 activator omaveloxolone in primates. Drug. Des. Devel. Ther. 13, 1259–1270 (2019).
Paupe, V. et al. Impaired nuclear Nrf2 translocation undermines the oxidative stress response in Friedreich ataxia. PLoS ONE 4, e4253 (2009).
Abeti, R., Baccaro, A., Esteras, N. & Giunti, P. Novel Nrf2-inducer prevents mitochondrial defects and oxidative stress in Friedreich’s ataxia models. Front. Cell. Neurosci. 12, 188 (2018).
Lynch, D. R. et al. Efficacy of omaveloxolone in Friedreich’s ataxia: delayed-start analysis of the MOXIe extension. Mov. Disord. 38, 313–320 (2023).
Pane, C. et al. Rationale and protocol of a double-blind, randomized, placebo-controlled trial to test the efficacy, safety, and tolerability of dimethyl fumarate in Friedreich ataxia (DMF-FA-201). Front. Neurosci. 17, 1260977 (2023).
Linker, R. A. et al. Fumaric acid esters exert neuroprotective effects in neuroinflammation via activation of the Nrf2 antioxidant pathway. Brain 134, 678–692 (2011).
Hayashi, G. et al. Dimethyl fumarate mediates Nrf2-dependent mitochondrial biogenesis in mice and humans. Hum. Mol. Genet. 26, 2864–2873 (2017).
Jasoliya, M. et al. Dimethyl fumarate dosing in humans increases frataxin expression: a potential therapy for Friedreich’s ataxia. PLoS ONE 14, e0217776 (2019).
La Rosa, P., Petrillo, S., Fiorenza, M. T., Bertini, E. S. & Piemonte, F. Ferroptosis in Friedreich’s ataxia: a metal-induced neurodegenerative disease. Biomolecules 10, 1551 (2020).
Wenzel, S. E. et al. PEBP1 wardens ferroptosis by enabling lipoxygenase generation of lipid death signals. Cell 171, 628–641.e26 (2017).
Friedreich’s Ataxia Research Alliance. Drug development pipeline. FARA https://www.curefa.org/drug-development/ (2024).
Parkinson, M. H., Schulz, J. B. & Giunti, P. Co-enzyme Q10 and idebenone use in Friedreich’s ataxia. J. Neurochem. 126, 125–141 (2013).
Boddaert, N. et al. Selective iron chelation in Friedreich ataxia: biologic and clinical implications. Blood 110, 401–408 (2007).
Pandolfo, M. et al. Deferiprone in Friedreich ataxia: a 6-month randomized controlled trial. Ann. Neurol. 76, 509–521 (2014).
Martelli, A. et al. Iron regulatory protein 1 sustains mitochondrial iron loading and function in frataxin deficiency. Cell Metab. 21, 311–323 (2015).
Grander, M. et al. Genetic determined iron starvation signature in Friedreich’s ataxia. Mov. Disord. 39, 1088–1098 (2024).
Harding, I. H. et al. Localized changes in dentate nucleus shape and magnetic susceptibility in Friedreich ataxia. Mov. Disord. 39, 1109–1118 (2024).
Patel, M. et al. Open-label pilot study of oral methylprednisolone for the treatment of patients with Friedreich ataxia. Muscle Nerve 60, 571–575 (2019).
Yiu, E. M. et al. An open-label trial in Friedreich ataxia suggests clinical benefit with high-dose resveratrol, without effect on frataxin levels. J. Neurol. 262, 1344–1353 (2015).
Lynch, D. R. et al. Randomized, double-blind, placebo-controlled study of interferon-γ 1b in Friedreich ataxia. Ann. Clin. Transl. Neurol. 6, 546–553 (2019).
Lynch, D. R. et al. Double blind trial of a deuterated form of linoleic acid (RT001) in Friedreich ataxia. J. Neurol. 270, 1615–1623 (2023).
Metz, G. et al. Rating disease progression of Friedreich’s ataxia by the International Cooperative Ataxia Rating Scale: analysis of a 603-patient database. Brain 136, 259 (2013).
Pandolfo, M. et al. Efficacy and safety of leriglitazone in patients with Friedreich ataxia: a phase 2 double-blind, randomized controlled trial (FRAMES). Neurol. Genet. 8, e200034 (2022).
Marmolino, D. et al. PGC-1α down-regulation affects the antioxidant response in Friedreich’s ataxia. PLoS ONE 5, e10025 (2010).
Rodríguez-Pascau, L. et al. PPAR gamma agonist leriglitazone improves frataxin-loss impairments in cellular and animal models of Friedreich ataxia. Neurobiol. Dis. 148, 105162 (2021).
Chevis, C. F. et al. Spinal cord atrophy correlates with disability in Friedreich’s ataxia. Cerebellum 12, 43–47 (2013).
Dogan, I. et al. Structural characteristics of the central nervous system in Friedreich ataxia: an in vivo spinal cord and brain MRI study. J. Neurol. Neurosurg. Psychiatry 90, 615–617 (2019).
Georgiou-Karistianis, N. et al. A natural history study to track brain and spinal cord changes in individuals with Friedreich’s ataxia: TRACK-FA study protocol. PLoS ONE 17, e0269649 (2022).
Lynch, D. R., Perlman, S. L. & Meier, T. A phase 3, double-blind, placebo-controlled trial of idebenone in Friedreich ataxia. Arch. Neurol. 67, 941–947 (2010).
Rummey, C., Perlman, S., Subramony, S. H., Farmer, J. & Lynch, D. R. Evaluating mFARS in pediatric Friedreich’s ataxia: insights from the FACHILD study. Ann. Clin. Transl. Neurol. 11, 1290–1300 (2024).
Roche, B. et al. Test-retest reliability of an instrumented electronic walkway system (GAITRite) for the measurement of spatio-temporal gait parameters in young patients with Friedreich’s ataxia. Gait Posture 66, 45–50 (2018).
Park, S. Y. et al. Cardiac, skeletal, and smooth muscle mitochondrial respiration: are all mitochondria created equal? Am. J. Physiol. Hear. Circ. Physiol. 307, H346 (2014).
Vorgerd, M. et al. Mitochondrial impairment of human muscle in Friedreich ataxia in vivo. Neuromuscul. Disord. 10, 430–435 (2000).
Nachbauer, W. et al. Bioenergetics of the calf muscle in Friedreich ataxia patients measured by 31P-MRS before and after treatment with recombinant human erythropoietin. PLoS ONE 8, e69229 (2013).
Sival, D. A. et al. In children with Friedreich ataxia, muscle and ataxia parameters are associated. Dev. Med. Child. Neurol. 53, 529–534 (2011).
Nachbauer, W. et al. Skeletal muscle involvement in Friedreich ataxia and potential effects of recombinant human erythropoietin administration on muscle regeneration and neovascularization. J. Neuropathol. Exp. Neurol. 71, 708–715 (2012).
Acknowledgements
E.I. and S.B. are members of the European Reference Network for Rare Neurological Diseases (ERN-RND) (project ID 739510).
Author information
Authors and Affiliations
Contributions
E.I. researched data for the article. E.I., J.F., S.P., M.R. and S.B. contributed substantially to discussion of the content. E.I., M.B.D. and M.C.F. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks G. De Michèle, J. Santos, A. Koeppen and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Indelicato, E., Delatycki, M.B., Farmer, J. et al. A global perspective on research advances and future challenges in Friedreich ataxia. Nat Rev Neurol 21, 204–215 (2025). https://doi.org/10.1038/s41582-025-01065-y
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41582-025-01065-y
This article is cited by
-
Human pluripotent stem cell models of Friedreich’s ataxia: innovations, considerations, and future perspectives
Stem Cell Research & Therapy (2026)
-
Characteristics of Adverse Events and Clinical Risks of Omaveloxolone Based on FAERS Data
The Cerebellum (2025)