Abstract
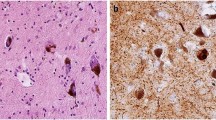
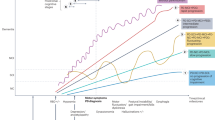
Biological definitions of neurological diseases are now becoming a reality, although still in the research phase. This development will recategorize neurological diseases, providing objective diagnostics and the promise of therapeutics that target biological mechanisms — similar to the strategy that has proven successful in tumours and other conditions. In this Perspective article, we discuss this development for dementias with dominant Lewy pathology, as the availability of biological assays for this pathology has sparked new interest in a single disease diagnosis for all individuals positive for α-synuclein. On the basis of current evidence, we argue that an α-synuclein assay alone is unlikely to be a specific criterion for a spectrum of clinical syndromes with Lewy pathology or a definitive diagnostic marker for Lewy body dementia. We advocate that one biological assay will not reflect the complex spatiotemporal features of brain pathology. Diverse sequential mechanisms underpin the highly heterogeneous phenotypes and clinicopathological processes of Lewy body dementias. Disease modification, if possible, will be most effective when it targets the early underlying mechanisms, especially those leading to aggressive phenotypes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Szeto, J. Y. Y. et al. Dementia in long-term Parkinson’s disease patients: a multicentre retrospective study. NPJ Parkinsons Dis. 6, 2 (2020).
Liu, L. et al. Characterization of de novo dementia with Lewy body with different duration of rapid eye movement sleep behavior disorder. Sleep. Med. 114, 101–108 (2024).
Chia, R. et al. Genome sequencing analysis identifies new loci associated with Lewy body dementia and provides insights into its genetic architecture. Nat. Genet. 53, 294–303 (2021).
McKeith, I. G. et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB consortium. Neurology 89, 88–100 (2017).
Aarsland, D. et al. Parkinson disease-associated cognitive impairment. Nat. Rev. Dis. Prim. 7, 47 (2021).
Pedersen, K. F., Larsen, J. P., Tysnes, O. B. & Alves, G. Natural course of mild cognitive impairment in Parkinson disease: a 5-year population-based study. Neurology 88, 767–774 (2017).
Sim, J., Li, H., Hameed, S. & Ting, S. K. S. Clinical manifestations of early-onset dementia with Lewy bodies compared with late-onset dementia with Lewy bodies and early-onset Alzheimer disease. JAMA Neurol. 79, 702–709 (2022).
Savica, R. et al. Incidence of dementia with Lewy bodies and Parkinson disease dementia. JAMA Neurol. 70, 1396–1402 (2013).
Elder, G. J., Lazar, A. S., Alfonso-Miller, P. & Taylor, J. P. Sleep disturbances in Lewy body dementia: a systematic review. Int. J. Geriatr. Psychiatry https://doi.org/10.1002/gps.5814 (2022).
Choudhury, P. et al. The temporal onset of the core features in dementia with Lewy bodies. Alzheimers Dement. 18, 591–601 (2022).
Chiu, S. Y. et al. Sex differences in dementia with Lewy bodies: focused review of available evidence and future directions. Parkinsonism Relat. Disord. 107, 105285 (2023).
McKeith, I. G. et al. Research criteria for the diagnosis of prodromal dementia with Lewy bodies. Neurology 94, 743–755 (2020).
Roos, D. S., Klein, M., Deeg, D. J. H., Doty, R. L. & Berendse, H. W. Prevalence of prodromal symptoms of Parkinson’s disease in the late middle-aged population. J. Parkinsons Dis. 12, 967–974 (2022).
Hely, M. A., Reid, W. G., Adena, M. A., Halliday, G. M. & Morris, J. G. The Sydney Multicenter Study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov. Disord. 23, 837–844 (2008).
Zhou, Z. et al. Characteristics of autonomic dysfunction in Parkinson’s disease: a large Chinese multicenter cohort study. Front. Aging Neurosci. 13, 761044 (2021).
Poewe, W. et al. Parkinson disease. Nat. Rev. Dis. Prim. 3, 17013 (2017).
Ferman, T. J. et al. Nonamnestic mild cognitive impairment progresses to dementia with Lewy bodies. Neurology 81, 2032–2038 (2013).
Pan, C. et al. Characterizing mild cognitive impairment in prodromal Parkinson’s disease: a community-based study in China. CNS Neurosci. Ther. 28, 259–268 (2022).
Speelberg, D. H. B. et al. Prodromal cognitive deficits and the risk of subsequent Parkinson’s disease. Brain Sci. 12, 199 (2022).
Kalbe, E. et al. Subtypes of mild cognitive impairment in patients with Parkinson’s disease: evidence from the LANDSCAPE study. J. Neurol. Neurosurg. Psychiatry 87, 1099–1105 (2016).
Hansen, N., Timaus, C., Bouter, C., Lange, C. & Packross, K. Delirium-onset of prodromal dementia with Lewy bodies – putative brainstem-related pathomechanism and clinical relevance. Front. Aging Neurosci. 14, 829098 (2022).
Gunawardana, C. W., Matar, E. & Lewis, S. J. G. The clinical phenotype of psychiatric-onset prodromal dementia with Lewy bodies: a scoping review. J. Neurol. 271, 606–617 (2024).
Gerakios, F. et al. Delirium is more common and associated with worse outcomes in Parkinson’s disease compared to older adult controls: results of two prospective longitudinal cohort studies. Age Ageing 53, afae046 (2024).
Berg, D. et al. Prodromal Parkinson disease subtypes – key to understanding heterogeneity. Nat. Rev. Neurol. 17, 349–361 (2021).
Patterson, L., Rushton, S. P., Attems, J., Thomas, A. J. & Morris, C. M. Degeneration of dopaminergic circuitry influences depressive symptoms in Lewy body disorders. Brain Pathol. 29, 544–557 (2019).
Pagonabarraga, J., Bejr-Kasem, H., Martinez-Horta, S. & Kulisevsky, J. Parkinson disease psychosis: from phenomenology to neurobiological mechanisms. Nat. Rev. Neurol. 20, 135–150 (2024).
Zhou, L. et al. Early- and late-onset of isolated rapid eye movement sleep behavior disorder: a retrospective cohort study. Sleep. Med. 105, 1–8 (2023).
Outeiro, T. F. et al. Dementia with Lewy bodies: an update and outlook. Mol. Neurodegener. 14, 5 (2019).
Mellergaard, C., Waldemar, G., Vogel, A. & Frederiksen, K. S. Characterising the prodromal phase in dementia with Lewy bodies. Parkinsonism Relat. Disord. 107, 105279 (2023).
Heinzel, S. et al. Update of the MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 34, 1464–1470 (2019).
Figorilli, M. et al. Considering REM sleep behavior disorder in the management of Parkinson’s disease. Nat. Sci. Sleep. 15, 333–352 (2023).
Mastenbroek, S. E. et al. Disease progression modelling reveals heterogeneity in trajectories of Lewy-type α-synuclein pathology. Nat. Commun. 15, 5133 (2024).
Jellinger, K. A. Morphological basis of Parkinson disease-associated cognitive impairment: an update. J. Neural Transm. 129, 977–999 (2022).
Parkkinen, L. et al. Disentangling the relationship between Lewy bodies and nigral neuronal loss in Parkinson’s disease. J. Parkinsons Dis. 1, 277–286 (2011).
Halliday, G., Hely, M., Reid, W. & Morris, J. The progression of pathology in longitudinally followed patients with Parkinson’s disease. Acta Neuropathol. 115, 409–415 (2008).
De Pablo-Fernandez, E., Lees, A. J., Holton, J. L. & Warner, T. T. Prognosis and neuropathologic correlation of clinical subtypes of Parkinson disease. JAMA Neurol. 76, 470–479 (2019).
Lenka, A., Hegde, S., Jhunjhunwala, K. R. & Pal, P. K. Interactions of visual hallucinations, rapid eye movement sleep behavior disorder and cognitive impairment in Parkinson’s disease: a review. Parkinsonism Relat. Disord. 22, 1–8 (2016).
Walker, L., Stefanis, L. & Attems, J. Clinical and neuropathological differences between Parkinson’s disease, Parkinson’s disease dementia and dementia with Lewy bodies – current issues and future directions. J. Neurochem. 150, 467–474 (2019).
Harding, A. J. & Halliday, G. M. Cortical Lewy body pathology in the diagnosis of dementia. Acta Neuropathol. 102, 355–363 (2001).
Adamowicz, D. H. et al. Hippocampal α-synuclein in dementia with Lewy bodies contributes to memory impairment and is consistent with spread of pathology. J. Neurosci. 37, 1675–1684 (2017).
La, C. et al. Hippocampal CA1 subfield predicts episodic memory impairment in Parkinson’s disease. Neuroimage Clin. 23, 101824 (2019).
Harding, A. J., Broe, G. A. & Halliday, G. M. Visual hallucinations in Lewy body disease relate to Lewy bodies in the temporal lobe. Brain 125, 391–403 (2002).
Yamamoto, R. et al. Investigation of Lewy pathology in the visual pathway of brains of dementia with Lewy bodies. J. Neurol. Sci. 246, 95–101 (2006).
Jellinger, K. A. Behavioral disorders in dementia with Lewy bodies: old and new knowledge. J. Neural Transm. https://doi.org/10.1007/s00702-024-02823-w (2024).
Smith, C. et al. Neuropathology of dementia in patients with Parkinson’s disease: a systematic review of autopsy studies. J. Neurol. Neurosurg. Psychiatry 90, 1234–1243 (2019).
Howlett, D. R. et al. Regional multiple pathology scores are associated with cognitive decline in Lewy body dementias. Brain Pathol. 25, 401–408 (2015).
Hansen, D. et al. Novel clinicopathological characteristics differentiate dementia with Lewy bodies from Parkinson’s disease dementia. Neuropathol. Appl. Neurobiol. 47, 143–156 (2021).
Toledo, J. B. et al. Dementia with Lewy bodies: impact of co-pathologies and implications for clinical trial design. Alzheimers Dement. 19, 318–332 (2023).
Walker, L., Simpson, H., Thomas, A. J. & Attems, J. Prevalence, distribution, and severity of cerebral amyloid angiopathy differ between Lewy body diseases and Alzheimer’s disease. Acta Neuropathol. Commun. 12, 28 (2024).
Ghebremedhin, E. et al. Inverse relationship between cerebrovascular lesions and severity of Lewy body pathology in patients with Lewy body diseases. J. Neuropathol. Exp. Neurol. 69, 442–448 (2010).
Gan, J. et al. White matter hyperintensities in cognitive impairment with Lewy body disease: a multicentre study. Eur. J. Neurol. 30, 3711–3721 (2023).
Kantarci, K. et al. FDG PET metabolic signatures distinguishing prodromal DLB and prodromal AD. Neuroimage Clin. 31, 102754 (2021).
Chin, K. S. et al. Prevalence of cerebral microbleeds in Alzheimer’s disease, dementia with Lewy bodies and Parkinson’s disease dementia: a systematic review and meta-analysis. Neurobiol. Aging 134, 74–83 (2024).
Nitchingham, A., Kumar, V., Shenkin, S., Ferguson, K. J. & Caplan, G. A. A systematic review of neuroimaging in delirium: predictors, correlates and consequences. Int. J. Geriatr. Psychiatry 33, 1458–1478 (2018).
Cummings, J. L. et al. The role of dopaminergic imaging in patients with symptoms of dopaminergic system neurodegeneration. Brain 134, 3146–3166 (2011).
Trujillo, P., Aumann, M. A. & Claassen, D. O. Neuromelanin-sensitive MRI as a promising biomarker of catecholamine function. Brain 147, 337–351 (2024).
Inagawa, Y. et al. Utility of neuromelanin-sensitive MRI in the diagnosis of dementia with Lewy bodies. PLoS ONE 19, e0309885 (2024).
Biondetti, E. et al. The spatiotemporal changes in dopamine, neuromelanin and iron characterizing Parkinson’s disease. Brain 144, 3114–3125 (2021).
Jellinger, K. A. & Korczyn, A. D. Are dementia with Lewy bodies and Parkinson’s disease dementia the same disease? BMC Med. 16, 34 (2018).
Jack, C. R. Jr. et al. Revised criteria for diagnosis and staging of Alzheimer’s disease: Alzheimer’s Association Workgroup. Alzheimers Dement. 20, 5143–5169 (2024).
Endo, H. et al. Imaging α-synuclein pathologies in animal models and patients with Parkinson’s and related diseases. Neuron 112, 2540–2557.e8 (2024).
Chopra, A. & Outeiro, T. F. Aggregation and beyond: α-synuclein-based biomarkers in synucleinopathies. Brain 147, 81–90 (2024).
Simuni, T. et al. A biological definition of neuronal α-synuclein disease: towards an integrated staging system for research. Lancet Neurol. 23, 178–190 (2024).
Siderowf, A. et al. Assessment of heterogeneity among participants in the Parkinson’s Progression Markers Initiative Cohort using α-synuclein seed amplification: a cross-sectional study. Lancet Neurol. 22, 407–417 (2023).
Bentivenga, G. M. et al. Performance of a seed amplification assay for misfolded α-synuclein in cerebrospinal fluid and brain tissue in relation to Lewy body disease stage and pathology burden. Acta Neuropathol. 147, 18 (2024).
Gomperts, S. N. et al. Imaging amyloid deposition in Lewy body diseases. Neurology 71, 903–910 (2008).
Nedelska, Z. et al. Association of longitudinal β-amyloid accumulation determined by positron emission tomography with clinical and cognitive decline in adults with probable Lewy body dementia. JAMA Netw. Open. 2, e1916439 (2019).
Petrou, M. et al. Amyloid deposition in Parkinson’s disease and cognitive impairment: a systematic review. Mov. Disord. 30, 928–935 (2015).
Donaghy, P., Thomas, A. J. & O’Brien, J. T. Amyloid PET imaging in Lewy body disorders. Am. J. Geriatr. Psychiatry 23, 23–37 (2015).
Diaz-Galvan, P. et al. β-Amyloid load on PET along the continuum of dementia with Lewy bodies. Neurology 101, e178–e188 (2023).
Gmitterova, K. et al. Cerebrospinal fluid markers analysis in the differential diagnosis of dementia with Lewy bodies and Parkinson’s disease dementia. Eur. Arch. Psychiatry Clin. Neurosci. 270, 461–470 (2020).
Katayama, T. et al. Cerebrospinal fluid levels of α-synuclein, amyloid β, tau, phosphorylated tau, and neuron-specific enolase in patients with Parkinson’s disease, dementia with Lewy bodies or other neurological disorders: their relationships with cognition and nuclear medicine imaging findings. Neurosci. Lett. 715, 134564 (2020).
Parnetti, L. et al. Cerebrospinal fluid biomarkers in Parkinson’s disease with dementia and dementia with Lewy bodies. Biol. Psychiatry 64, 850–855 (2008).
Martinez-Valbuena, I. et al. α-Synuclein molecular behavior and nigral proteomic profiling distinguish subtypes of Lewy body disorders. Acta Neuropathol. 144, 167–185 (2022).
Kon, T. et al. Molecular behavior of α-synuclein is associated with membrane transport, lipid metabolism, and ubiquitin-proteasome pathways in Lewy body disease. Int. J. Mol. Sci. 25, 2676 (2024).
Lau, D. et al. Single-molecule fingerprinting reveals different growth mechanisms in seed amplification assays for different polymorphs of α-synuclein fibrils. ACS Chem. Neurosci. 15, 3270–3285 (2024).
Frey, L. et al. On the pH-dependence of α-synuclein amyloid polymorphism and the role of secondary nucleation in seed-based amyloid propagation. Elife 12, RP93562 (2024).
Xu, C. K. et al. α-Synuclein oligomers form by secondary nucleation. Nat. Commun. 15, 7083 (2024).
Feleke, R. et al. Cross-platform transcriptional profiling identifies common and distinct molecular pathologies in Lewy body diseases. Acta Neuropathol. 142, 449–474 (2021).
Kon, T. et al. Neuronal SNCA transcription during Lewy body formation. Acta Neuropathol. Commun. 11, 185 (2023).
Hallacli, E. et al. The Parkinson’s disease protein α-synuclein is a modulator of processing bodies and mRNA stability. Cell 185, 2035–2056.e3 (2022).
Shantaraman, A. et al. Network proteomics of the Lewy body dementia brain reveals presynaptic signatures distinct from Alzheimer’s disease. Mol. Neurodegen. 19, 60 (2024).
Xu, J. et al. Identification of key genes and signaling pathways associated with dementia with Lewy bodies and Parkinson’s disease dementia using bioinformatics. Front. Neurol. 14, 1029370 (2023).
Asghar, M. et al. Mitochondrial biogenesis, telomere length and cellular senescence in Parkinson’s disease and Lewy body dementia. Sci. Rep. 12, 17578 (2022).
Larsson, V., Torisson, G. & Londos, E. Relative survival in patients with dementia with Lewy bodies and Parkinson’s disease dementia. PLoS ONE 13, e0202044 (2018).
Guerreiro, R. et al. Heritability and genetic variance of dementia with Lewy bodies. Neurobiol. Dis. 127, 492–501 (2019).
Bandres-Ciga, S., Diez-Fairen, M., Kim, J. J. & Singleton, A. B. Genetics of Parkinson’s disease: an introspection of its journey towards precision medicine. Neurobiol. Dis. 137, 104782 (2020).
Smirnov, D. S. et al. Cognitive decline profiles differ in Parkinson disease dementia and dementia with Lewy bodies. Neurology 94, e2076–e2087 (2020).
Fields, J. A. Cognitive and neuropsychiatric features in Parkinson’s and Lewy body dementias. Arch. Clin. Neuropsychol. 32, 786–801 (2017).
Geng, C., Tan, L. & Chen, C. Neuropsychiatric symptoms profile and markers of Alzheimer disease-type pathology in patients with Lewy body dementias. Brain Res. 1833, 148881 (2024).
Allan, L. M. et al. Autonomic dysfunction in dementia. J. Neurol. Neurosurg. Psychiatry 78, 671–677 (2007).
Hiorth, Y. H., Schulz, J., Pedersen, K. F., Tysnes, O. B. & Alves, G. Orthostatic hypotension and risk of mild cognitive impairment and dementia in Parkinson’s disease. Mov. Disord. Clin. Pract. 11, 1365–1372 (2024).
Wyman-Chick, K. A. et al. Differentiating prodromal dementia with Lewy bodies from prodromal Alzheimer’s disease: a pragmatic review for clinicians. Neurol. Ther. 13, 885–906 (2024).
Goetz, C. G. & Stebbins, G. T. Mortality and hallucinations in nursing home patients with advanced Parkinson’s disease. Neurology 45, 669–671 (1995).
Weil, R. S. & Reeves, S. Hallucinations in Parkinson’s disease: new insights into mechanisms and treatments. Adv. Clin. Neurosci. Rehabil. 19, ONNS5189 (2020).
Simonet, C., Schrag, A., Lees, A. J. & Noyce, A. J. The motor prodromes of Parkinson’s disease: from bedside observation to large-scale application. J. Neurol. 268, 2099–2108 (2021).
Seger, A. et al. Clinical subtypes in patients with isolated REM sleep behaviour disorder. NPJ Parkinsons Dis. 9, 155 (2023).
Postuma, R. B. & Berg, D. Advances in markers of prodromal Parkinson disease. Nat. Rev. Neurol. 12, 622–634 (2016).
Matar, E., Phillips, J. R., Martens, K. A. E., Halliday, G. M. & Lewis, S. J. G. Impaired color discrimination – a specific marker of hallucinations in Lewy body disorders. J. Geriatr. Psychiatry Neurol. 32, 257–264 (2019).
Khan, S. A. et al. Insights into the management of Lewy body dementia: a scoping review. Ann. Med. Surg. 86, 930–942 (2024).
Samudra, N. et al. Clinicopathological correlation of cerebrospinal fluid α-synuclein seed amplification assay in a behavioral neurology autopsy cohort. Alzheimers Dement. 20, 3334–3341 (2024).
Scott, G. D. et al. Fluid and tissue biomarkers of Lewy body dementia: report of an LBDA symposium. Front. Neurol. 12, 805135 (2021).
Foska, A. et al. Classical cerebrospinal fluid biomarkers in dementia with Lewy bodies. Medicina 58, 612 (2022).
Kuzkina, A. et al. Combining skin and olfactory α-synuclein seed amplification assays (SAA) – towards biomarker-driven phenotyping in synucleinopathies. NPJ Parkinsons Dis. 9, 79 (2023).
Acknowledgements
G.M.H. discloses support for the research and publication of this work from a National Health and Medical Research Council senior leadership fellowship (1176607) and Y.F. is supported by the University of Sydney (BISA-FRP2022). Both authors have been supported in part by Aligning Science Across Parkinson’s (020529 and 020505) through the Michael J. Fox Foundation for Parkinson’s Research.
Author information
Authors and Affiliations
Contributions
Both authors wrote and conceptualized the article. G.M.H. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks Nobutaka Hattori, Jaime Kulisevsky and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, Y., Halliday, G.M. Dementia with Lewy bodies and Parkinson disease dementia — the same or different and is it important?. Nat Rev Neurol 21, 394–403 (2025). https://doi.org/10.1038/s41582-025-01090-x
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41582-025-01090-x