Abstract
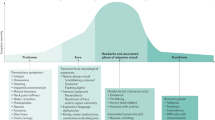
Migraine with aura is characterized by recurrent attacks of visual and, occasionally, sensory, language and/or motor disturbances, typically followed by headache. Migraine with aura can be associated with allodynia and vascular and psychiatric comorbidities. The electrophysiological cause of the aura is cortical spreading depolarization, a wave of depolarization that propagates slowly across the cortical surface, producing reversible metabolic and electrochemical perturbations. In this Review, we focus on the relationship of spreading depolarization with migraine aura and migraine headache. Abundant evidence causally links spreading depolarization to the headache phase of migraine with aura, as it can activate trigeminal nociceptors, produce dural and cortical inflammation, and induce trigeminal pain behaviour in rodents. In experimental models, migraine prophylaxis reduces susceptibility to spreading depolarization, and abortive treatments abrogate trigeminal pain behaviour that is induced by spreading depolarization. Although questions remain about the role of spreading depolarization in migraine with aura and models of spreading depolarization need to be refined, the cumulative evidence suggests that spreading depolarization is a putative target for therapeutic intervention in migraine. Elucidating the mechanisms by which spreading depolarization can induce trigeminal pain could facilitate drug discovery, and models of spreading depolarization could be effective screening platforms for migraine therapies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017).
Stovner, L. J. et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 17, 954–976 (2018).
Bonafede, M. et al. Direct and indirect healthcare resource utilization and costs among migraine patients in the United States. Headache 58, 700–714 (2018).
Burch, R., Rizzoli, P. & Loder, E. The prevalence and impact of migraine and severe headache in the United States: figures and trends from government health studies. Headache 58, 496–505 (2018).
Burch, R. C., Buse, D. C. & Lipton, R. B. Migraine: epidemiology, burden, and comorbidity. Neurol. Clin. 37, 631–649 (2019).
Lipton, R. B. et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 68, 343–349 (2007).
Headache classification committee of the international headache society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia https://doi.org/10.1177/0333102417738202 (2018).
Andress-Rothrock, D., King, W. & Rothrock, J. An analysis of migraine triggers in a clinic-based population. Headache 50, 1366–1370 (2010).
Lipton, R. B. et al. Identifying natural subgroups of migraine based on comorbidity and concomitant condition profiles: results of the chronic migraine epidemiology and outcomes (CaMEO) study. Headache 58, 933–947 (2018).
Leao, A. A. P. Spreading depression of activity in cerebral cortex. J. Neurophysiol. 7, 359–390 (1944).
Lashley, K. S. Patterns of cerebral integration indicated by the scotomas of migraine. Arch. Neurol. Psychiatry 46, 331–339 (1941).
Leao, A. A. P. & Morison, R. S. Propagation of spreading cortical depression. J. Neurophysiol. 8, 33–45 (1945).
Hadjikhani, N. et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc. Natl Acad. Sci. USA 98, 4687–4692 (2001).
Moskowitz, M. A., Nozaki, K. & Kraig, R. P. Neocortical spreading depression provokes the expression of c-fos protein-like immunoreactivity within trigeminal nucleus caudalis via trigeminovascular mechanisms. J. Neurosci. 13, 1167–1177 (1993).
Zhang, X. et al. Activation of central trigeminovascular neurons by cortical spreading depression. Ann. Neurol. 69, 855–865 (2011).
Melo-Carrillo, A. et al. Selective inhibition of trigeminovascular neurons by fremanezumab: a humanized monoclonal anti-CGRP antibody. J. Neurosci. 37, 7149–7163 (2017).
Zhang, X. et al. Activation of meningeal nociceptors by cortical spreading depression: implications for migraine with aura. J. Neurosci. 30, 8807–8814 (2010).
Filiz, A. et al. CGRP receptor antagonist MK-8825 attenuates cortical spreading depression induced pain behavior. Cephalalgia 39, 354–365 (2019).
Cottier, K. E. et al. Loss of blood–brain barrier integrity in a Kcl-induced model of episodic headache enhances CNS drug delivery. eNeuro https://doi.org/10.1523/ENEURO.0116-18.2018 (2018).
Harriott, A. M. et al. Optogenetic spreading depression elicits trigeminal pain and anxiety behavior. Ann. Neurol. 89, 99–110 (2021).
Rodgers, C. I., Armstrong, G. A. & Robertson, R. M. Coma in response to environmental stress in the locust: a model for cortical spreading depression. J. Insect Physiol. 56, 980–990 (2010).
Andersen, M. K., Willot, Q. & MacMillan, H. A. A neurophysiological limit and its biogeographic correlations: cold-induced spreading depolarization in tropical butterflies. J. Exp. Biol. 226, jeb246313 (2023).
Robertson, R. M., Dawson-Scully, K. D. & Andrew, R. D. Neural shutdown under stress: an evolutionary perspective on spreading depolarization. J. Neurophysiol. 123, 885–895 (2020).
Gorji, A. et al. Spreading depression in human neocortical slices. Brain Res. 906, 74–83 (2001).
Strong, A. J. et al. Spreading and synchronous depressions of cortical activity in acutely injured human brain. Stroke 33, 2738–2743 (2002).
McLeod, G. A., Josephson, C. B., Engbers, J. D. T., Cooke, L. J. & Wiebe, S. Mapping the migraine: intracranial recording of cortical spreading depression in migraine with aura. Headache 65, 658–665 (2025).
Rasmussen, B. K. & Olesen, J. Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 12, 221–228 (1992).
Buse, D. C. et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) study. Headache 53, 1278–1299 (2013).
Lipton, R. B. et al. Cutaneous allodynia in the migraine population. Ann. Neurol. 63, 148–158 (2008).
Lovati, C. et al. Allodynia in different forms of migraine. Neurol. Sci. 28, S220–S221 (2007).
Burstein, R., Yarnitsky, D., Goor-Aryeh, I., Ransil, B. J. & Bajwa, Z. H. An association between migraine and cutaneous allodynia. Ann. Neurol. 47, 614–624 (2000).
LoPinto, C., Young, W. B. & Ashkenazi, A. Comparison of dynamic (brush) and static (pressure) mechanical allodynia in migraine. Cephalalgia 26, 852–856 (2006).
Oedegaard, K. J. et al. Migraine with and without aura: association with depression and anxiety disorder in a population-based study. The HUNT study. Cephalalgia 26, 1–6 (2006).
Kim, K. M. et al. Prevalence and impact of visual aura in migraine and probable migraine: a population study. Sci. Rep. 12, 426 (2022).
Lipton, R. B. et al. Allodynia is associated with initial and sustained response to acute migraine treatment: results from the American Migraine Prevalence and Prevention study. Headache 57, 1026–1040 (2017).
Viana, M. et al. Clinical features of migraine aura: results from a prospective diary-aided study. Cephalalgia 37, 979–989 (2017).
Russell, M. B. & Olesen, J. A nosographic analysis of the migraine aura in a general population. Brain 119, 355–361 (1996).
Hansen, J. M., Goadsby, P. J. & Charles, A. C. Variability of clinical features in attacks of migraine with aura. Cephalalgia 36, 216–224 (2016).
Airy, H. On a distinct form of transient hemiopsia. Philos. Trans. R. Soc. Lond. 160, 247–264 (1870).
Viana, M., Tronvik, E. A., Do, T. P., Zecca, C. & Hougaard, A. Clinical features of visual migraine aura: a systematic review. J. Headache Pain 20, 64 (2019).
Petrusic, I., Pavlovski, V., Vucinic, D. & Jancic, J. Features of migraine aura in teenagers. J. Headache Pain 15, 87 (2014).
Kelman, L. The aura: a tertiary care study of 952 migraine patients. Cephalalgia 24, 728–734 (2004).
Ahmed, M. A., Donaldson, S., Akor, F., Cahill, D. & Akilani, R. Olfactory hallucination in childhood primary headaches: case series. Cephalalgia 35, 234–239 (2015).
Henkin, R. I., Potolicchio, S. J. & Levy, L. M. Olfactory hallucinations without clinical motor activity: a comparison of unirhinal with birhinal phantosmia. Brain Sci. 3, 1483–1553 (2013).
Barrett, C. F., van den Maagdenberg, A., Frants, R. R. & Ferrari, M. D. Familial hemiplegic migraine. Adv. Genet. 63, 57–83 (2008).
Sutherland, H. G., Jenkins, B. & Griffiths, L. R. Genetics of migraine: complexity, implications, and potential clinical applications. Lancet Neurol. 23, 429–446 (2024).
Gosalia, H., Karsan, N. & Goadsby, P. J. Genetic mechanisms of migraine: insights from monogenic migraine mutations. Int. J. Mol. Sci. 24, 12697 (2023).
Pietrobon, D. & Moskowitz, M. A. Pathophysiology of migraine. Annu. Rev. Physiol. 75, 365–391 (2013).
Terwindt, G. M., Ophoff, R. A., Haan, J., Frants, R. R. & Ferrari, M. D. Familial hemiplegic migraine: a clinical comparison of families linked and unlinked to chromosome 19.DMG RG. Cephalalgia 16, 153–155 (1996).
Joutel, A. et al. A gene for familial hemiplegic migraine maps to chromosome 19. Nat. Genet. 5, 40–45 (1993).
Hartings, J. A. et al. The continuum of spreading depolarizations in acute cortical lesion development: examining Leao’s legacy. J. Cereb. Blood Flow Metab. https://doi.org/10.1177/0271678X16654495 (2016).
Pietrobon, D. & Moskowitz, M. A. Chaos and commotion in the wake of cortical spreading depression and spreading depolarizations. Nat. Rev. Neurosci. 15, 379–393 (2014).
Somjen, G. G. Mechanisms of spreading depression and hypoxic spreading depression-like depolarization. Physiol. Rev. 81, 1065–1096 (2001).
Ayata, C. & Lauritzen, M. Spreading depression, spreading depolarizations, and the cerebral vasculature. Physiol. Rev. 95, 953–993 (2015).
Dreier, J. P. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat. Med. 17, 439–447 (2011).
Eikermann-Haerter, K. et al. Abnormal synaptic Ca2+ homeostasis and morphology in cortical neurons of familial hemiplegic migraine type 1 mutant mice. Ann. Neurol. 78, 193–210 (2015).
Peters, O., Schipke, C. G., Hashimoto, Y. & Kettenmann, H. Different mechanisms promote astrocyte Ca2+ waves and spreading depression in the mouse neocortex. J. Neurosci. 23, 9888–9896 (2003).
Fabricius, M., Jensen, L. H. & Lauritzen, M. Microdialysis of interstitial amino acids during spreading depression and anoxic depolarization in rat neocortex. Brain Res. 612, 61–69 (1993).
Lindquist, B. E. & Shuttleworth, C. W. Adenosine receptor activation is responsible for prolonged depression of synaptic transmission after spreading depolarization in brain slices. Neuroscience 223, 365–376 (2012).
Seidel, J. L., Escartin, C., Ayata, C., Bonvento, G. & Shuttleworth, C. W. Multifaceted roles for astrocytes in spreading depolarization: a target for limiting spreading depolarization in acute brain injury? Glia 64, 5–20 (2016).
Grafstein, B. Subverting the hegemony of the synapse: complicity of neurons, astrocytes, and vasculature in spreading depression and pathology of the cerebral cortex. Brain Res. Rev. 66, 123–132 (2010).
Grafstein, B. Locus of propagation of spreading cortical depression. J. Neurophysiol. 19, 308–316 (1956).
Hansen, A. J. & Zeuthen, T. Extracellular ion concentrations during spreading depression and ischemia in the rat brain cortex. Acta Physiol. Scand. 113, 437–445 (1981).
Obrenovitch, T. P. & Zilkha, E. High extracellular potassium, and not extracellular glutamate, is required for the propagation of spreading depression. J. Neurophysiol. 73, 2107–2114 (1995).
Marrannes, R., Willems, R., De Prins, E. & Wauquier, A. Evidence for a role of the N-methyl-d-aspartate (NMDA) receptor in cortical spreading depression in the rat. Brain Res. 457, 226–240 (1988).
Masvidal-Codina, E. et al. Characterization of optogenetically-induced cortical spreading depression in awake mice using graphene micro-transistor arrays. J. Neural Eng. https://doi.org/10.1088/1741-2552/abecf3 (2021).
Crivellaro, G. et al. Specific activation of GluN1-N2B NMDA receptors underlies facilitation of cortical spreading depression in a genetic mouse model of migraine with reduced astrocytic glutamate clearance. Neurobiol. Dis. 156, 105419 (2021).
Mody, I., Lambert, J. D. & Heinemann, U. Low extracellular magnesium induces epileptiform activity and spreading depression in rat hippocampal slices. J. Neurophysiol. 57, 869–888 (1987).
Santos, E. et al. Radial, spiral and reverberating waves of spreading depolarization occur in the gyrencephalic brain. Neuroimage 99, 244–255 (2014).
Santos, E., Sanchez-Porras, R., Sakowitz, O. W., Dreier, J. P. & Dahlem, M. A. Heterogeneous propagation of spreading depolarizations in the lissencephalic and gyrencephalic brain. J. Cereb. Blood Flow Metab. 37, 2639–2643 (2017).
Cain, S. M. et al. In vivo imaging reveals that pregabalin inhibits cortical spreading depression and propagation to subcortical brain structures. Proc. Natl Acad. Sci. USA 114, 2401–2406 (2017).
Vinogradova, L. V., Koroleva, V. I. & Bures, J. Re-entry waves of Leao’s spreading depression between neocortex and caudate nucleus. Brain Res. 538, 161–164 (1991).
Bures, J., Buresova, O., Fifkova, E. & Rabending, G. Reversible deafferentation of cerebral cortex by thalamic spreading depression. Exp. Neurol. 12, 55–67 (1965).
Yuzawa, I. et al. Cortical spreading depression impairs oxygen delivery and metabolism in mice. J. Cereb. Blood Flow Metab. 32, 376–386 (2012).
Ayata, C. et al. Pronounced hypoperfusion during spreading depression in mouse cortex. J. Cereb. Blood Flow Metab. 24, 1172–1182 (2004).
Ostergaard, L. et al. Neurovascular coupling during cortical spreading depolarization and -depression. Stroke 46, 1392–1401 (2015).
Ayata, C. Spreading depression and neurovascular coupling. Stroke 44, S87–S89 (2013).
Sadeghian, H. et al. Spreading depolarizations trigger caveolin-1-dependent endothelial transcytosis. Ann. Neurol. 84, 409–423 (2018).
Cha, Y. H., Millett, D., Kane, M., Jen, J. & Baloh, R. Adult-onset hemiplegic migraine with cortical enhancement and oedema. Cephalalgia 27, 1166–1170 (2007).
Dreier, J. P. et al. Opening of the blood–brain barrier preceding cortical edema in a severe attack of FHM type II. Neurology 64, 2145–2147 (2005).
Kors, E. E. et al. Delayed cerebral edema and fatal coma after minor head trauma: role of the CACNA1A calcium channel subunit gene and relationship with familial hemiplegic migraine. Ann. Neurol. 49, 753–760 (2001).
Hougaard, A. et al. Increased brainstem perfusion, but no blood–brain barrier disruption, during attacks of migraine with aura. Brain 140, 1633–1642 (2017).
Amin, F. M. et al. Intact blood–brain barrier during spontaneous attacks of migraine without aura: a 3T DCE-MRI study. Eur. J. Neurol. 24, 1116–1124 (2017).
Schain, A. J., Melo-Carrillo, A., Strassman, A. M. & Burstein, R. Cortical spreading depression closes paravascular space and impairs glymphatic flow: implications for migraine headache. J. Neurosci. 37, 2904–2915 (2017).
Takizawa, T. et al. Non-invasively triggered spreading depolarizations induce a rapid pro-inflammatory response in cerebral cortex. J. Cereb. Blood Flow Metab. https://doi.org/10.1177/0271678X19859381 (2019).
Dell'Orco, M. et al. Repetitive spreading depolarization induces gene expression changes related to synaptic plasticity and neuroprotective pathways. Front. Cell. Neurosci. 14, 1292661 (2023).
Caggiano, A. O. & Kraig, R. P. Eicosanoids and nitric oxide influence induction of reactive gliosis from spreading depression in microglia but not astrocytes. J. Comp. Neurol. 369, 93–108 (1996).
Kraig, R. P., Dong, L. M., Thisted, R. & Jaeger, C. B. Spreading depression increases immunohistochemical staining of glial fibrillary acidic protein. J. Neurosci. 11, 2187–2198 (1991).
Escartin, C. et al. Reactive astrocyte nomenclature, definitions, and future directions. Nat. Neurosci. 24, 312–325 (2021).
Yang, L. et al. Human and mouse trigeminal ganglia cell atlas implicates multiple cell types in migraine. Neuron 110, 1806–1821 e1808 (2022).
Sukhotinsky, I. et al. Chronic daily cortical spreading depressions suppress spreading depression susceptibility. Cephalalgia 31, 1601–1608 (2011).
Nedergaard, M. & Hansen, A. J. Spreading depression is not associated with neuronal injury in the normal brain. Brain Res. 449, 395–398 (1988).
Dreier, J. P. et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: review and recommendations of the COSBID research group. J. Cereb. Blood Flow Metab. 37, 1595–1625 (2017).
Suryavanshi, P., Reinhart, K. M., Shuttleworth, C. W. & Brennan, K. C. Action potentials are critical for the propagation of focally elicited spreading depolarizations. J. Neurosci. 42, 2371–2383 (2022).
Eikermann-Haerter, K., Can, A. & Ayata, C. Pharmacological targeting of spreading depression in migraine. Expert Rev. Neurother. 12, 297–306 (2012).
Takizawa, T. et al. Non-invasively triggered spreading depolarizations induce a rapid pro-inflammatory response in cerebral cortex. J. Cereb. Blood Flow Metab. 40, 1117–1131 (2020).
Tang, C. et al. Cortical spreading depolarisation-induced facial hyperalgesia, photophobia and hypomotility are ameliorated by sumatriptan and olcegepant. Sci. Rep. 10, 11408 (2020).
Milner, P. M. Note on a possible correspondence between the scotomas of migraine and spreading depression of Leao. Electroencephalogr. Clin. Neurophysiol. 10, 705 (1958).
Olesen, J., Larsen, B. & Lauritzen, M. Focal hyperemia followed by spreading oligemia and impaired activation of rCBF in classic migraine. Ann. Neurol. 9, 344–352 (1981).
Lauritzen, M., Olsen, T. S., Lassen, N. A. & Paulson, O. B. Regulation of regional cerebral blood flow during and between migraine attacks. Ann. Neurol. 14, 569–572 (1983).
Lauritzen, M., Skyhoj Olsen, T., Lassen, N. A. & Paulson, O. B. Changes in regional cerebral blood flow during the course of classic migraine attacks. Ann. Neurol. 13, 633–641 (1983).
O’Brien, M. D. Cerebral-cortex-perfusion rates in migraine. Lancet 1, 1036 (1967).
Dreier, J. P. & Reiffurth, C. The stroke-migraine depolarization continuum. Neuron 86, 902–922 (2015).
Bowyer, S. M., Aurora, K. S., Moran, J. E., Tepley, N. & Welch, K. M. Magnetoencephalographic fields from patients with spontaneous and induced migraine aura. Ann. Neurol. 50, 582–587 (2001).
Barkley, G. L. et al. Magnetoencephalographic studies of migraine. Headache 30, 428–434 (1990).
Bowyer, S. M. et al. Analysis of MEG signals of spreading cortical depression with propagation constrained to a rectangular cortical strip. II. Gyrencephalic swine model. Brain Res. 843, 79–86 (1999).
Wijesinghe, R. S. & Tepley, N. A four sphere model for calculating the magnetic field associated with spreading cortical depression. Brain Topogr. 9, 191–202 (1997).
Bolay, H., Vuralli, D. & Goadsby, P. J. Aura and Head pain: relationship and gaps in the translational models. J. Headache Pain 20, 94 (2019).
Bahra, A., Matharu, M. S., Buchel, C., Frackowiak, R. S. & Goadsby, P. J. Brainstem activation specific to migraine headache. Lancet 357, 1016–1017 (2001).
Weiller, C. et al. Brain stem activation in spontaneous human migraine attacks. Nat. Med. 1, 658–660 (1995).
Schulte, L. H. & May, A. Of generators, networks and migraine attacks. Curr. Opin. Neurol. 30, 241–245 (2017).
Thomsen, A. V. et al. Clinical features of migraine with aura: a REFORM study. J. Headache Pain 25, 22 (2024).
Hansen, J. M. et al. Migraine headache is present in the aura phase: a prospective study. Neurology 79, 2044–2049 (2012).
Eriksen, M. K., Thomsen, L. L. & Olesen, J. Sensitivity and specificity of the new international diagnostic criteria for migraine with aura. J. Neurol. Neurosurg. Psychiatry 76, 212–217 (2005).
Arngrim, N. et al. Heterogenous migraine aura symptoms correlate with visual cortex functional magnetic resonance imaging responses. Ann. Neurol. 82, 925–939 (2017).
Olesen, J. et al. Timing and topography of cerebral blood flow, aura, and headache during migraine attacks. Ann. Neurol. 28, 791–798 (1990).
Lambert, G. A., Truong, L. & Zagami, A. S. Effect of cortical spreading depression on basal and evoked traffic in the trigeminovascular sensory system. Cephalalgia 31, 1439–1451 (2011).
Burstein, R., Strassman, A. & Moskowitz, M. Can cortical spreading depression activate central trigeminovascular neurons without peripheral input? Pitfalls of a new concept. Cephalalgia 32, 509–511 (2012).
Zhao, J. & Levy, D. Cortical spreading depression promotes persistent mechanical sensitization of intracranial meningeal afferents: implications for the intracranial mechanosensitivity of migraine. eNeuro https://doi.org/10.1523/ENEURO.0287-16.2016 (2016).
Fioravanti, B. et al. Evaluation of cutaneous allodynia following induction of cortical spreading depression in freely moving rats. Cephalalgia 31, 1090–1100 (2011).
Han, S. M. et al. Prevalence and characteristics of cutaneous allodynia in probable migraine. Sci. Rep. 11, 2467 (2021).
Langford, D. J. et al. Coding of facial expressions of pain in the laboratory mouse. Nat. Methods 7, 447–449 (2010).
Strassman, A. M. et al. Atogepant — an orally-administered CGRP antagonist — attenuates activation of meningeal nociceptors by CSD. Cephalalgia 42, 933–943 (2022).
Melo-Carrillo, A. et al. Combined onabotulinumtoxinA/atogepant treatment blocks activation/sensitization of high-threshold and wide-dynamic range neurons. Cephalalgia 41, 17–32 (2021).
Melo-Carrillo, A. et al. Fremanezumab-A humanized monoclonal anti-CGRP antibody-inhibits thinly myelinated (aδ) but not unmyelinated (C) meningeal nociceptors. J. Neurosci. 37, 10587–10596 (2017).
Cresta, E., Bellotti, A., Rinaldi, G., Corbelli, I. & Sarchielli, P. Effect of anti-CGRP-targeted therapy on migraine aura: results of an observational case series study. CNS Neurosci. Ther. 30, e14595 (2024).
Melo-Carrillo, A., Schain, A. J., Stratton, J., Strassman, A. M. & Burstein, R. Fremanezumab and its isotype slow propagation rate and shorten cortical recovery period but do not prevent occurrence of cortical spreading depression in rats with compromised blood–brain barrier. Pain 161, 1037–1043 (2020).
Levy, D. & Moskowitz, M. A. Meningeal mechanisms and the migraine connection. Annu. Rev. Neurosci. 46, 39–58 (2023).
Schain, A. J., Melo-Carrillo, A., Ashina, S., Strassman, A. M. & Burstein, R. Celecoxib reduces cortical spreading depression-induced macrophage activation and dilatation of dural but not pial arteries in rodents: implications for mechanism of action in terminating migraine attacks. Pain 161, 1019–1026 (2020).
Melo-Carrillo, A. et al. Exploring the effects of extracranial injections of botulinum toxin type A on prolonged intracranial meningeal nociceptors responses to cortical spreading depression in female rats. Cephalalgia 39, 1358–1365 (2019).
Ailani, J., Burch, R. C., Robbins, M. S. & Board of Directors of the American Headache Society The American Headache Society consensus statement: update on integrating new migraine treatments into clinical practice. Headache 61, 1021–1039 (2021).
Mathew, N. T., Kailasam, J., Meadors, L., Chernyschev, O. & Gentry, P. Intravenous valproate sodium (depacon) aborts migraine rapidly: a preliminary report. Headache 40, 720–723 (2000).
Edwards, K. R., Norton, J. & Behnke, M. Comparison of intravenous valproate versus intramuscular dihydroergotamine and metoclopramide for acute treatment of migraine headache. Headache 41, 976–980 (2001).
Bakhshayesh, B., Seyed Saadat, S. M., Rezania, K., Hatamian, H. & Hossieninezhad, M. A randomized open-label study of sodium valproate vs sumatriptan and metoclopramide for prolonged migraine headache. Am. J. Emerg. Med. 31, 540–544 (2013).
Tepe, N. et al. The thalamic reticular nucleus is activated by cortical spreading depression in freely moving rats: prevention by acute valproate administration. Eur. J. Neurosci. 41, 120–128 (2015).
Fontaine, D. et al. Dural and pial pain-sensitive structures in humans: new inputs from awake craniotomies. Brain 141, 1040–1048 (2018).
Ray, B. W. H. Experimental studies on headache: pain-sensitive structures of the head and their significance in headache. Arch. Surg. 41, 813–856 (1940).
Lauritzen, M., Hansen, A. J., Kronborg, D. & Wieloch, T. Cortical spreading depression is associated with arachidonic acid accumulation and preservation of energy charge. J. Cereb. Blood Flow Metab. 10, 115–122 (1990).
Rustenhoven, J. et al. Functional characterization of the dural sinuses as a neuroimmune interface. Cell 184, 1000–1016.e1027 (2021).
Kaag Rasmussen, M. et al. Trigeminal ganglion neurons are directly activated by influx of CSF solutes in a migraine model. Science 385, 80–86 (2024).
Harriott, A. M. & Orlova, Y. Anatomy and physiology of headache. Semin. Neurol. 42, 459–473 (2022).
Eftekhari, S., Warfvinge, K., Blixt, F. W. & Edvinsson, L. Differentiation of nerve fibers storing CGRP and CGRP receptors in the peripheral trigeminovascular system. J. Pain 14, 1289–1303 (2013).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 28, 183–187 (1990).
Gallai, V. et al. Vasoactive peptide levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalalgia 15, 384–390 (1995).
O’Shaughnessy, C. T. & Connor, H. E. Investigation of the role of tachykinin NK1, NK2 receptors and CGRP receptors in neurogenic plasma protein extravasation in dura mater. Eur. J. Pharmacol. 263, 193–198 (1994).
Markowitz, S., Saito, K. & Moskowitz, M. A. Neurogenically mediated leakage of plasma protein occurs from blood vessels in dura mater but not brain. J. Neurosci. 7, 4129–4136 (1987).
Lee, W. S., Moussaoui, S. M. & Moskowitz, M. A. Blockade by oral or parenteral RPR 100893 (a non-peptide NK1 receptor antagonist) of neurogenic plasma protein extravasation within guinea-pig dura mater and conjunctiva. Br. J. Pharmacol. 112, 920–924 (1994).
Goldstein, D. J. et al. Ineffectiveness of neurokinin-1 antagonist in acute migraine: a crossover study. Cephalalgia 17, 785–790 (1997).
Roon, K. I. et al. No acute antimigraine efficacy of CP-122,288, a highly potent inhibitor of neurogenic inflammation: results of two randomized, double-blind, placebo-controlled clinical trials. Ann. Neurol. 47, 238–241 (2000).
Lee, W. S. & Moskowitz, M. A. Conformationally restricted sumatriptan analogues, CP-122,288 and CP-122,638 exhibit enhanced potency against neurogenic inflammation in dura mater. Brain Res. 626, 303–305 (1993).
Moskowitz, M. A., Reinhard, J. F. Jr., Romero, J., Melamed, E. & Pettibone, D. J. Neurotransmitters and the fifth cranial nerve: is there a relation to the headache phase of migraine? Lancet 2, 883–885 (1979).
Edvinsson, L., Haanes, K. A. & Warfvinge, K. Does inflammation have a role in migraine? Nat. Rev. Neurol. 15, 483–490 (2019).
Charles, A., Nwaobi, S. E. & Goadsby, P. Inflammation in migraine…or not…: a critical evaluation of the evidence. Headache 61, 1575–1578 (2021).
Dimitriadou, V., Buzzi, M. G., Moskowitz, M. A. & Theoharides, T. C. Trigeminal sensory fiber stimulation induces morphological changes reflecting secretion in rat dura mater mast cells. Neuroscience 44, 97–112 (1991).
Levy, D., Burstein, R., Kainz, V., Jakubowski, M. & Strassman, A. M. Mast cell degranulation activates a pain pathway underlying migraine headache. Pain 130, 166–176 (2007).
McIlvried, L. A., Cruz, J. A., Borghesi, L. A. & Gold, M. S. Sex-, stress-, and sympathetic post-ganglionic-dependent changes in identity and proportions of immune cells in the dura. Cephalalgia 37, 36–48 (2017).
Dimlich, R. V., Keller, J. T., Strauss, T. A. & Fritts, M. J. Linear arrays of homogeneous mast cells in the dura mater of the rat. J. Neurocytol. 20, 485–503 (1991).
McMenamin, P. G. Distribution and phenotype of dendritic cells and resident tissue macrophages in the dura mater, leptomeninges, and choroid plexus of the rat brain as demonstrated in wholemount preparations. J. Comp. Neurol. 405, 553–562 (1999).
Zhang, X. C., Strassman, A. M., Burstein, R. & Levy, D. Sensitization and activation of intracranial meningeal nociceptors by mast cell mediators. J. Pharmacol. Exp. Ther. 322, 806–812 (2007).
Rozniecki, J. J., Dimitriadou, V., Lambracht-Hall, M., Pang, X. & Theoharides, T. C. Morphological and functional demonstration of rat dura mater mast cell–neuron interactions in vitro and in vivo. Brain Res. 849, 1–15 (1999).
Ottosson, A. & Edvinsson, L. Release of histamine from dural mast cells by substance P and calcitonin gene-related peptide. Cephalalgia 17, 166–174 (1997).
Bolay, H. et al. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat. Med. 8, 136–142 (2002).
Schain, A. J., Melo-Carrillo, A., Stratton, J., Strassman, A. M. & Burstein, R. CSD-induced arterial dilatation and plasma protein extravasation are unaffected by fremanezumab: implications for CGRP’s role in migraine with aura. J. Neurosci. 39, 6001–6011 (2019).
Williamson, D. J., Hargreaves, R. J., Hill, R. G. & Shepheard, S. L. Intravital microscope studies on the effects of neurokinin agonists and calcitonin gene-related peptide on dural vessel diameter in the anaesthetized rat. Cephalalgia 17, 518–524 (1997).
Schain, A. J. et al. Activation of pial and dural macrophages and dendritic cells by cortical spreading depression. Ann. Neurol. 83, 508–521 (2018).
Karatas, H. et al. Spreading depression triggers headache by activating neuronal Panx1 channels. Science 339, 1092–1095 (2013).
Pelegrin, P. & Surprenant, A. Pannexin-1 mediates large pore formation and interleukin-1β release by the ATP-gated P2X7 receptor. EMBO J. 25, 5071–5082 (2006).
Chen, S. P. et al. Inhibition of the P2X7–PANX1 complex suppresses spreading depolarization and neuroinflammation. Brain 140, 1643–1656 (2017).
Zhao, J., Harrison, S. & Levy, D. Meningeal P2X7 signaling mediates migraine-related intracranial mechanical hypersensitivity. J. Neurosci. 43, 5975–5985 (2023).
Sword, J., Croom, D., Wang, P. L., Thompson, R. J. & Kirov, S. A. Neuronal pannexin-1 channels are not molecular routes of water influx during spreading depolarization-induced dendritic beading. J. Cereb. Blood Flow Metab. 37, 1626–1633 (2017).
Chen, P. Y. et al. Neuronal NLRP3 inflammasome mediates spreading depolarization-evoked trigeminovascular activation. Brain 146, 2989–3002 (2023).
Takizawa, T. et al. High-mobility group box 1 is an important mediator of microglial activation induced by cortical spreading depression. J. Cereb. Blood Flow Metab. 37, 890–901 (2017).
Albrecht, D. S. et al. Imaging of neuroinflammation in migraine with aura: a [11C]PBR28 PET/MRI study. Neurology 92, e2038–e2050 (2019).
Hadjikhani, N. et al. Extra-axial inflammatory signal in parameninges in migraine with visual aura. Ann. Neurol. 87, 939–949 (2020).
Klass, A., Sánchez-Porras, R. & Santos, E. Systematic review of the pharmacological agents that have been tested against spreading depolarizations. J. Cereb. Blood Flow Metab. 38, 1149–1179 (2018).
Ayata, C., Jin, H., Kudo, C., Dalkara, T. & Moskowitz, M. A. Suppression of cortical spreading depression in migraine prophylaxis. Ann. Neurol. 59, 652–661 (2006).
Hoffmann, U., Dilekoz, E., Kudo, C. & Ayata, C. Oxcarbazepine does not suppress cortical spreading depression. Cephalalgia 31, 537–542 (2011).
Bogdanov, V. B. et al. Migraine preventive drugs differentially affect cortical spreading depression in rat. Neurobiol. Dis. 41, 430–435 (2011).
Richter, F., Mikulik, O., Ebersberger, A. & Schaible, H. G. Noradrenergic agonists and antagonists influence migration of cortical spreading depression in rat-a possible mechanism of migraine prophylaxis and prevention of postischemic neuronal damage. J. Cereb. Blood Flow Metab. 25, 1225–1235 (2005).
Unekawa, M., Tomita, Y., Toriumi, H. & Suzuki, N. Suppressive effect of chronic peroral topiramate on potassium-induced cortical spreading depression in rats. Cephalalgia 32, 518–527 (2012).
Akerman, S. & Goadsby, P. J. Topiramate inhibits cortical spreading depression in rat and cat: impact in migraine aura. Neuroreport 16, 1383–1387 (2005).
Silberstein, S. et al. Oxcarbazepine in migraine headache: a double-blind, randomized, placebo-controlled study. Neurology 70, 548–555 (2008).
Parker, P. D. et al. Non-canonical glutamate signaling in a genetic model of migraine with aura. Neuron 109, 611–628 e618 (2021).
Reinhart, K. M. & Shuttleworth, C. W. Ketamine reduces deleterious consequences of spreading depolarizations. Exp. Neurol. 305, 121–128 (2018).
Vitale, M., Tottene, A., Zarin Zadeh, M., Brennan, K. C. & Pietrobon, D. Mechanisms of initiation of cortical spreading depression. J. Headache Pain 24, 105 (2023).
Chung, D. Y. et al. Determinants of optogenetic cortical spreading depolarizations. Cereb. Cortex 29, 1150–1161 (2019).
Hertle, D. N. et al. Effect of analgesics and sedatives on the occurrence of spreading depolarizations accompanying acute brain injury. Brain 135, 2390–2398 (2012).
Sanchez-Porras, R. et al. The effect of ketamine on optical and electrical characteristics of spreading depolarizations in gyrencephalic swine cortex. Neuropharmacology 84, 52–61 (2014).
Carlson, A. P., Abbas, M., Alunday, R. L., Qeadan, F. & Shuttleworth, C. W. Spreading depolarization in acute brain injury inhibited by ketamine: a prospective, randomized, multiple crossover trial. J. Neurosurg. 130, 1–7 (2018).
Hoydonckx, Y., McKechnie, T., Peer, M., Englesakis, M. & Kumar, P. A systematic review of the efficacy of ketamine for craniofacial pain. Can. J. Pain 7, 2210167 (2023).
Afridi, S. K., Giffin, N. J., Kaube, H. & Goadsby, P. J. A randomized controlled trial of intranasal ketamine in migraine with prolonged aura. Neurology 80, 642–647 (2013).
Etchison, A. R. et al. Low-dose ketamine does not improve migraine in the emergency department: a randomized placebo-controlled trial. West. J. Emerg. Med. 19, 952–960 (2018).
Benish, T. et al. The THINK (Treatment of Headache with Intranasal Ketamine) trial: a randomized controlled trial comparing intranasal ketamine with intravenous metoclopramide. J. Emerg. Med. 56, 248–257 e241 (2019).
Coste, J., Voisin, D. L., Luccarini, P. & Dallel, R. A role for wind-up in trigeminal sensory processing: intensity coding of nociceptive stimuli in the rat. Cephalalgia 28, 631–639 (2008).
Eide, P. K. Wind-up and the NMDA receptor complex from a clinical perspective. Eur. J. Pain 4, 5–15 (2000).
Parsons, C. G., Stoffler, A. & Danysz, W. Memantine: a NMDA receptor antagonist that improves memory by restoration of homeostasis in the glutamatergic system-too little activation is bad, too much is even worse. Neuropharmacology 53, 699–723 (2007).
Peeters, M. et al. Effects of pan- and subtype-selective N-methyl-d-aspartate receptor antagonists on cortical spreading depression in the rat: therapeutic potential for migraine. J. Pharmacol. Exp. Ther. 321, 564–572 (2007).
Reinhart, K. M., Humphrey, A., Brennan, K. C., Carlson, A. P. & Shuttleworth, C. W. Memantine improves recovery after spreading depolarization in brain slices and can be considered for future clinical trials. Neurocrit. Care 35, 135–145 (2021).
Noruzzadeh, R. et al. Memantine for prophylactic treatment of migraine without aura: a randomized double-blind placebo-controlled study. Headache 56, 95–103 (2016).
Shanmugam, S., Karunaikadal, K., Varadarajan, S. & Krishnan, M. Memantine ameliorates migraine headache. Ann. Indian Acad. Neurol. 22, 286–290 (2019).
Zhou, T., Tang, Y. & Zhu, H. Effectiveness and safety of memantine for headache: a meta-analysis of randomized controlled studies. Clin. Neuropharmacol. 45, 40–44 (2022).
Peikert, A., Wilimzig, C. & Kohne-Volland, R. Prophylaxis of migraine with oral magnesium: results from a prospective, multi-center, placebo-controlled and double-blind randomized study. Cephalalgia 16, 257–263 (1996).
Wang, F. et al. Oral magnesium oxide prophylaxis of frequent migrainous headache in children: a randomized, double-blind, placebo-controlled trial. Headache 43, 601–610 (2003).
van der Hel, W. S., van den Bergh, W. M., Nicolay, K., Tulleken, K. A. & Dijkhuizen, R. M. Suppression of cortical spreading depressions after magnesium treatment in the rat. Neuroreport 9, 2179–2182 (1998).
Hallak, M., Berman, R. F., Irtenkauf, S. M., Evans, M. I. & Cotton, D. B. Peripheral magnesium sulfate enters the brain and increases the threshold for hippocampal seizures in rats. Am. J. Obstet. Gynecol. 167, 1605–1610 (1992).
Ghabriel, M. N. & Vink, R. in Magnesium in the Central Nervous System (eds R. Vink & M. Nechifor) (Univ. Adelaide Press, 2011).
Bigal, M. E., Bordini, C. A., Tepper, S. J. & Speciali, J. G. Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. Cephalalgia 22, 345–353 (2002).
Steiner, T. J., Findley, L. J. & Yuen, A. W. Lamotrigine versus placebo in the prophylaxis of migraine with and without aura. Cephalalgia 17, 109–112 (1997).
Silberstein, S., Goode-Sellers, S., Twomey, C., Saiers, J. & Ascher, J. Randomized, double-blind, placebo-controlled, phase II trial of gabapentin enacarbil for migraine prophylaxis. Cephalalgia 33, 101–111 (2013).
Hoffmann, U., Dilekoz, E., Kudo, C. & Ayata, C. Gabapentin suppresses cortical spreading depression susceptibility. J. Cereb. Blood Flow Metab. 30, 1588–1592 (2010).
Smith, M. I. et al. Repetitive cortical spreading depression in a gyrencephalic feline brain: inhibition by the novel benzoylamino-benzopyran SB-220453. Cephalalgia 20, 546–553 (2000).
Hauge, A. W., Asghar, M. S., Schytz, H. W., Christensen, K. & Olesen, J. Effects of tonabersat on migraine with aura: a randomised, double-blind, placebo-controlled crossover study. Lancet Neurol. 8, 718–723 (2009).
Tassorelli, C. et al. Noninvasive vagus nerve stimulation as acute therapy for migraine: the randomized PRESTO study. Neurology 91, e364–e373 (2018).
Martelletti, P. et al. Consistent effects of non-invasive vagus nerve stimulation (nVNS) for the acute treatment of migraine: additional findings from the randomized, sham-controlled, double-blind PRESTO trial. J. Headache Pain 19, 101 (2018).
Grazzi, L. et al. Practical and clinical utility of non-invasive vagus nerve stimulation (nVNS) for the acute treatment of migraine: a post hoc analysis of the randomized, sham-controlled, double-blind PRESTO trial. J. Headache Pain 19, 98 (2018).
Diener, H. C. et al. Non-invasive vagus nerve stimulation (nVNS) for the preventive treatment of episodic migraine: the multicentre, double-blind, randomised, sham-controlled PREMIUM trial. Cephalalgia 39, 1475–1487 (2019).
Chen, S. P. et al. Vagus nerve stimulation inhibits cortical spreading depression. Pain 157, 797–805 (2016).
Liu, T. T. et al. Efficacy profile of noninvasive vagus nerve stimulation on cortical spreading depression susceptibility and the tissue response in a rat model. J. Headache Pain 23, 12 (2022).
Morais, A. et al. Vagus nerve stimulation inhibits cortical spreading depression exclusively through central mechanisms. Pain 161, 1661–1669 (2020).
Andreou, A. P. et al. Transcranial magnetic stimulation and potential cortical and trigeminothalamic mechanisms in migraine. Brain 139, 2002–2014 (2016).
Lloyd, J. O. et al. Cortical mechanisms of single-pulse transcranial magnetic stimulation in migraine. Neurotherapeutics 17, 1973–1987 (2020).
Lloyd, J. O. et al. Single-pulse transcranial magnetic stimulation for the preventive treatment of difficult-to-treat migraine: a 12-month prospective analysis. J. Headache Pain 23, 63 (2022).
Starling, A. J. et al. A multicenter, prospective, single arm, open label, observational study of sTMS for migraine prevention (ESPOUSE Study). Cephalalgia 38, 1038–1048 (2018).
Lipton, R. B. et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 9, 373–380 (2010).
Misra, U. K., Kalita, J. & Bhoi, S. K. High-rate repetitive transcranial magnetic stimulation in migraine prophylaxis: a randomized, placebo-controlled study. J. Neurol. 260, 2793–2801 (2013).
Leahu, P. et al. Increased migraine-free intervals with multifocal repetitive transcranial magnetic stimulation. Brain Stimul. 14, 1544–1552 (2021).
Ayata, C. Spreading depression: from serendipity to targeted therapy in migraine prophylaxis. Cephalalgia 29, 1095–1114 (2009).
Takizawa, T., Ayata, C. & Chen, S. P. Therapeutic implications of cortical spreading depression models in migraine. Prog. Brain Res. 255, 29–67 (2020).
Ayata, C. Pearls and pitfalls in experimental models of spreading depression. Cephalalgia 33, 604–613 (2013).
Morais, A., Qin, T., Ayata, C. & Harriott, A. M. Inhibition of persistent sodium current reduces spreading depression-evoked allodynia in a mouse model of migraine with aura. Pain 164, 2564–2571 (2023).
Harriott, A. M., Kaya, M. & Ayata, C. Oxytocin shortens spreading depolarization-induced periorbital allodynia. J. Headache Pain 25, 152 (2024).
Harriott, A. M. et al. The effect of sex and estrus cycle stage on optogenetic spreading depression induced migraine-like pain phenotypes. J. Headache Pain 24, 85 (2023).
Harriott, A. M., Takizawa, T., Chung, D. Y. & Chen, S. P. Spreading depression as a preclinical model of migraine. J. Headache Pain 20, 45 (2019).
Tuttle, A. H. et al. A deep neural network to assess spontaneous pain from mouse facial expressions. Mol. Pain 14, 1744806918763658 (2018).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
A.M.H. serves on the board of directors for the Headache Cooperative of New England, the American Migraine Foundation and the American Headache Society, and has received compensation from Abbvie and Theranica for participation on scientific advisory boards. C.A. declares no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks A. Andreou, T. Dalkara, D. Pietrobon, M. Shibata and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harriott, A.M., Ayata, C. Spreading depolarization as a therapeutic target in migraine. Nat Rev Neurol 21, 529–543 (2025). https://doi.org/10.1038/s41582-025-01128-0
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41582-025-01128-0
This article is cited by
-
Spreading depolarization activates the cGAS–STING pathway and drives cranial nociception: therapeutic potential of STING modulation
The Journal of Headache and Pain (2026)