Abstract
Improving glucose sensitivity remains an unmet medical need in treating type 2 diabetes (T2D). Dorzagliatin is a dual-acting, orally bioavailable glucokinase activator that enhances glucokinase activity in a glucose-dependent manner, improves glucose-stimulated insulin secretion and demonstrates effects on glycemic control in patients with T2D. We report the findings of a randomized, double-blind, placebo-controlled phase 3 clinical trial to evaluate the efficacy and safety of dorzagliatin in patients with T2D. Eligible drug-naïve patients with T2D (n = 463) were randomly assigned to the dorzagliatin or placebo group at a ratio of 2:1 for 24 weeks of double-blind treatment, followed by 28 weeks of open-label treatment with dorzagliatin for all patients. The primary efficacy endpoint was the change in glycated hemoglobin from baseline to week 24. Safety was assessed throughout the trial. At week 24, the least-squares mean change in glycated hemoglobin from baseline (95% confidence interval) was −1.07% (−1.19%, −0.95%) in the dorzagliatin group and −0.50% (−0.68%, −0.32%) in the placebo group (estimated treatment difference, −0.57%; 95% confidence interval: −0.79%, −0.36%; P < 0.001). The incidence of adverse events was similar between the two groups. There were no severe hypoglycemia events or drug-related serious adverse events in the dorzagliatin group. In summary, dorzagliatin improved glycemic control in drug-naïve patients with T2D and showed a good tolerability and safety profile.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data from analyses in the SEED study are not publicly available due to the sponsor’s contractual obligations. We encourage researchers or parties interested in collaboration for noncommercial use to submit an application to the corresponding authors (lichen@huamedicine.com). Applications should specifically outline the data the parties are interested in receiving and how the data will be used; the use of the data must also comply with the Human Genetics Resources Administration requirements of China and other country-specific or region-specific regulations. All shared data will be de-identified and will be made available 2 years after the date of publication. A signed data access agreement with the sponsor is required before accessing the shared data. The study protocol and statistical analysis plan are provided with the paper.
References
International Diabetes Federation. IDF Diabetes Atlas tenth edition (2021).
DeFronzo, R. A. Lilly lecture 1987. The triumvirate: beta cell, muscle, liver. A collusion responsible for NIDDM. Diabetes 37, 667–687 (1988).
Wang, L. et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317, 2515–2523 (2017).
Consortium, R. Lack of durable improvements in beta-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care 42, 1742–1751 (2019).
Basu, A. et al. Effects of type 2 diabetes on insulin secretion, insulin action, glucose effectiveness, and postprandial glucose metabolism. Diabetes Care 32, 866–872 (2009).
Rizza, R. A. Pathogenesis of fasting and postprandial hyperglycemia in type 2 diabetes: implications for therapy. Diabetes 59, 2697–2707 (2010).
Kahn, S. E. et al. Importance of early-phase insulin secretion to intravenous glucose tolerance in subjects with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 86, 5824–5829 (2001).
Schwartz, S. S. et al. The time is right for a new classification system for diabetes: rationale and implications of the beta-cell-centric classification schema. Diabetes Care 39, 179–186 (2016).
Chen, L. R&D Strategies for type 2 diabetes: elucidate the underlying pathology and improve the impaired organ functions. Prog. Pharm. Sci. 40, P161 (2016).
Wajchenberg, B. L. Beta-cell failure in diabetes and preservation by clinical treatment. Endocr. Rev. 28, 187–218 (2007).
Matschinsky, F. M. & Ellerman, J. E. Metabolism of glucose in the islets of Langerhans. J. Biol. Chem. 243, 2730–2736 (1968).
Matschinsky, F. M. & Wilson, D. F. The central role of glucokinase in glucose homeostasis: a perspective 50 years after demonstrating the presence of the enzyme in Islets of Langerhans. Front. Physiol. 10, 148 (2019).
Matschinsky, F. M. Assessing the potential of glucokinase activators in diabetes therapy. Nat. Rev. Drug Discov. 8, 399–416 (2009).
Matschinsky, F. M. Banting lecture 1995. A lesson in metabolic regulation inspired by the glucokinase glucose sensor paradigm. Diabetes 45, 223–241 (1996).
Agius, L. Glucokinase and molecular aspects of liver glycogen metabolism. Biochem. J. 414, 1–18 (2008).
Pino, M. F. et al. Glucokinase thermolability and hepatic regulatory protein binding are essential factors for predicting the blood glucose phenotype of missense mutations. J. Biol. Chem. 282, 13906–13916 (2007).
Raimondo, A. et al. Phenotypic severity of homozygous GCK mutations causing neonatal or childhood-onset diabetes is primarily mediated through effects on protein stability. Hum. Mol. Genet. 23, 6432–6440 (2014).
Matschinsky, F. M. Glucokinase, glucose homeostasis, and diabetes mellitus. Curr. Diab. Rep. 5, 171–176 (2005).
Froguel, P. et al. Familial hyperglycemia due to mutations in glucokinase. Definition of a subtype of diabetes mellitus. N. Engl. J. Med. 328, 697–702 (1993).
Glaser, B. et al. Familial hyperinsulinism caused by an activating glucokinase mutation. N. Engl. J. Med. 338, 226–230 (1998).
Heimberg, H. et al. The glucose sensor protein glucokinase is expressed in glucagon-producing alpha cells. Proc. Natl Acad. Sci. USA 93, 7036–7041 (1996).
Basco, D. et al. Alpha-cell glucokinase suppresses glucose-regulated glucagon secretion. Nat. Commun. 9, 546 (2018).
Moede, T. et al. Glucokinase intrinsically regulates glucose sensing and glucagon secretion in pancreatic alpha cells. Sci. Rep. 10, 20145 (2020).
Agius, L. Targeting hepatic glucokinase in type 2 diabetes: weighing the benefits and risks. Diabetes 58, 18–20 (2009).
Li, C. et al. Regulation of glucagon secretion in normal and diabetic human islets by gamma-hydroxybutyrate and glycine. J. Biol. Chem. 288, 3938–3951 (2013).
Haeusler, R. A. et al. Decreased expression of hepatic glucokinase in type 2 diabetes. Mol. Metab. 4, 222–226 (2015).
Jiang, M. H. et al. Hypermethylation of hepatic Gck promoter in ageing rats contributes to diabetogenic potential. Diabetologia 51, 1525–1533 (2008).
Basu, A. et al. Effects of type 2 diabetes on the ability of insulin and glucose to regulate splanchnic and muscle glucose metabolism: evidence for a defect in hepatic glucokinase activity. Diabetes 49, 272–283 (2000).
Basu, A. et al. Type 2 diabetes impairs splanchnic uptake of glucose but does not alter intestinal glucose absorption during enteral glucose feeding: additional evidence for a defect in hepatic glucokinase activity. Diabetes 50, 1351–1362 (2001).
Grimsby, J. et al. Allosteric activators of glucokinase: potential role in diabetes therapy. Science 301, 370–373 (2003).
Eiki, J. et al. Pharmacokinetic and pharmacodynamic properties of the glucokinase activator MK-0941 in rodent models of type 2 diabetes and healthy dogs. Mol. Pharmacol. 80, 1156–1165 (2011).
Sarabu, R. et al. Discovery of piragliatin–first glucokinase activator studied in type 2 diabetic patients. J. Med. Chem. 55, 7021–7036 (2012).
Vella, A. et al. Targeting hepatic glucokinase to treat diabetes with TTP399, a hepatoselective glucokinase activator. Sci. Transl. Med. 11, eaau3441 (2019).
Xu, H. et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of novel glucokinase activator HMS5552: results from a first-in-human single ascending dose study. Drug Des. Devel. Ther. 10, 1619–1626 (2016).
Ericsson, H. et al. Tolerability, pharmacokinetics, and pharmacodynamics of the glucokinase activator AZD1656, after single ascending doses in healthy subjects during euglycemic clamp. Int. J. Clin. Pharmacol. Ther. 50, 765–777 (2012).
Denney, W. S., Denham, D. S., Riggs, M. R. & Amin, N. B. Glycemic effect and safety of a systemic, partial glucokinase activator, PF-04937319, in patients with type 2 diabetes mellitus inadequately controlled on metformin—a randomized, crossover, active-controlled study. Clin. Pharmacol. Drug Dev. 5, 517–527 (2016).
Zhi, J. & Zhai, S. Effects of piragliatin, a glucokinase activator, on fasting and postprandial plasma glucose in patients with type 2 diabetes mellitus. J. Clin. Pharmacol. 56, 231–238 (2016).
Meininger, G. E. et al. Effects of MK-0941, a novel glucokinase activator, on glycemic control in insulin-treated patients with type 2 diabetes. Diabetes Care 34, 2560–2566 (2011).
Wilding, J. P., Leonsson-Zachrisson, M., Wessman, C. & Johnsson, E. Dose-ranging study with the glucokinase activator AZD1656 in patients with type 2 diabetes mellitus on metformin. Diabetes Obes. Metab. 15, 750–759 (2013).
Kiyosue, A., Hayashi, N., Komori, H., Leonsson-Zachrisson, M. & Johnsson, E. Dose-ranging study with the glucokinase activator AZD1656 as monotherapy in Japanese patients with type 2 diabetes mellitus. Diabetes Obes. Metab. 15, 923–930 (2013).
Amin, N. B. et al. Two dose-ranging studies with PF-04937319, a systemic partial activator of glucokinase, as add-on therapy to metformin in adults with type 2 diabetes. Diabetes Obes. Metab. 17, 751–759 (2015).
Katz, L. et al. AMG 151 (ARRY-403), a novel glucokinase activator, decreases fasting and postprandial glycaemia in patients with type 2 diabetes. Diabetes Obes. Metab. 18, 191–195 (2016).
Zhi, J. et al. A novel glucokinase activator RO4389620 improved fasting and postprandial plasma glucose in type 2 diabetic patients. Diabetologia 51, S23 (2008).
Zhai, S., Georgy, A., Liang, Z. & Zhi, J. Pharmacokinetic and pharmacodynamic drug interaction study of piragliatin, a glucokinase activator, and glyburide, a sulfonylurea, in type 2 diabetic patients. Clin. Pharmacol. Drug Dev. 5, 552–556 (2016).
Zheng, S. et al. Safety, pharmacokinetics, and pharmacodynamics of globalagliatin, a glucokinase activator, in chinese patients with type 2 diabetes mellitus: a randomized, phase ib, 28-day ascending dose study. Clin. Drug Investig. 40, 1155–1166 (2020).
Scheen, A. J. New hope for glucokinase activators in type 2 diabetes? Lancet Diabetes Endocrinol. 6, 591–593 (2018).
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin. J. Diabetes Mellitus 13, 315–409 (2021).
Zhu, D. et al. Dorzagliatin monotherapy in Chinese patients with type 2 diabetes: a dose-ranging, randomised, double-blind, placebo-controlled, phase 2 study. Lancet Diabetes Endocrinol. 6, 627–636 (2018).
Klein, K. R. et al. The SimpliciT1 study: a randomized, double-blind, placebo-controlled phase 1b/2 adaptive study of TTP399, a hepatoselective glucokinase activator, for adjunctive treatment of type 1 diabetes. Diabetes Care 44, 960–968 (2021).
McCafferty, K. et al. ARCADIA study protocol: a phase II, randomised, double-blind, placebo-controlled clinical trial to assess the safety and efficacy of AZD1656 in patients with diabetes hospitalised with suspected or confirmed COVID-19. BMJ Open 11, e049650 (2021).
Wang, P. et al. Effects of a novel glucokinase activator, HMS5552, on glucose metabolism in a rat model of type 2 diabetes mellitus. J. Diabetes Res. 2017, 5812607 (2017).
Zhu, X. X. et al. Dorzagliatin (HMS5552), a novel dual-acting glucokinase activator, improves glycaemic control and pancreatic β-cell function in patients with type 2 diabetes: a 28-day treatment study using biomarker-guided patient selection. Diabetes Obes. Metab. 20, 2113–2120 (2018).
Zhu, D. L. et al. Clinically differentiated glucokinase activator HMS5552: effective control of 24-hour glucose and improvement of beta cell function in T2DM patients. Diabetes https://doi.org/10.2337/db15-932-1471 (2015).
Chen, L., Shan, Y., Jin, X. & Lv, X. Dorzagliatin differentiates from early generation of glucokinase activators: an enzyme kinetics study. Diabetes 68, 1151-P (2019).
Davis, E. A. et al. Mutants of glucokinase cause hypoglycaemia- and hyperglycaemia syndromes and their analysis illuminates fundamental quantitative concepts of glucose homeostasis. Diabetologia 42, 1175–1186 (1999).
NCT05102149: Study to evaluate the safety and efficacy of PB-201 in treatment-naive patients with type 2 diabetes mellitus. https://www.clinicaltrials.gov/ct2/show/NCT05102149 (2021).
Chen, L., Zhang, J., Yang, R. & Feng, L. Glucokinase activator dorzagliatin (HMS5552) regulates GLP-1 release in T2D patients and is synergistic with sitagliptin and empagliflozin in optimizing beta-cell function. Diabetes 70, 117-LB (2021).
Miao, J. et al. Effect of renal impairment on the pharmacokinetics and safety of dorzagliatin, a novel dual-acting glucokinase activator. Clin. Transl. Sci. 15, 548–557 (2021).
DAWN Study Group. Dorzagliatin add-on therapy to metformin in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, phase 3 trial. Nat. Med. (2022) (in press).
MedDRA Maintenance and Support Services Organization. Introductory Guide to MedDRA version 23.0 (March 2020). https://www.meddra.org/how-to-use/support-documentation
Acknowledgements
This study was sponsored by Hua Medicine. We thank J. Chen for medical writing and editing support, funded by Hua Medicine; L. Li, C. Geng and L. Yuan (Hua Medicine) for assistance with the efficacy data; A. Wang (Hua Medicine) for assistance with the safety data; X. Liu (Hua Medicine) for assistance with the statistical analyses; and G. Yu and F. Tang, who reviewed an earlier version of the manuscript on behalf of Hua Medicine. Hua Medicine participated in the design, conduct and data analysis and interpretation of the clinical study, the preparation of the manuscript, and were involved in making the decision to publish. The study was also funded in part, by grants from the National Major Scientific and Technological Special Project for Significant New Drug Development (2014ZX09101002004 and 2018ZX09711002–012–001), the Shanghai Science and Technology Innovation Action Project (14431908300, 15XD1520500, 17DZ1910200 and 19431905200), the Shanghai Pudong District Science and Technology Innovation Action Project (PKJ2014-S06) and the Shanghai Municipal Commission of Economy and Informatization Innovation Action Project (XC-ZXSJ-01-2015-02 and 18XI-18).
Author information
Authors and Affiliations
Contributions
D.Zhu and L.Chen led the design, conduct and analysis of the clinical study and the development of the manuscript. X.Li and W.Yang contributed to the protocol design, data analysis and manuscript draft as the study consultants. The trial was designed and overseen by representatives of Hua Medicine with input from selected site investigators. The site investigators collected the data, and the sponsor performed the data analyses. All of the authors interpreted the data and vouched for its accuracy and completeness and the fidelity of the trial to the protocol. The first author wrote the first draft of the manuscript with assistance from an independent medical writer funded by the sponsor. The manuscript was subsequently revised and approved by all authors, who agreed to submit the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
L.Chen, Y. Zhao and Y. Zhang are employees of Hua Medicine. D.Zhu, X.Li and W.Yang served on the Diabetes Advisory Board for Hua Medicine. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Victor Volovici, Naveed Sattar and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Jennifer Sargent and Joao Monteiro, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
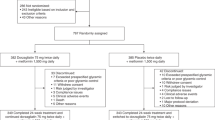
Extended Data Fig. 1 SEED trial design.
The SEED trial design was shown in the Extended Data Fig. 1, in which it showed the process of T2D patients completing the SEED study. Selected drug naive T2D patients entered into a 4 week single-blinded placebo run-in period followed by a randomization into a 24-week double blinded placebo controlled treatment to evaluate the primary efficacy and safety endpoints. Upon completion of the double blinded period, patients entered into an open-label 28 week treatment to evaluate drug safety endpoints, followed by a 1-week end of study follow-up.
Supplementary information
Supplementary Information
Supplementary Tables 1–10, clinical study protocol and statistical analysis plan
Rights and permissions
About this article
Cite this article
Zhu, D., Li, X., Ma, J. et al. Dorzagliatin in drug-naïve patients with type 2 diabetes: a randomized, double-blind, placebo-controlled phase 3 trial. Nat Med 28, 965–973 (2022). https://doi.org/10.1038/s41591-022-01802-6
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41591-022-01802-6
This article is cited by
-
Drug-induced regeneration of pancreatic beta cells: An approach to cellular therapeutic targets
Cell Regeneration (2025)
-
Glucokinase activator, circulating metabolites, and cardio-cerebrovascular diseases: a Mendelian randomization study
Cardiovascular Diabetology (2025)
-
An update on current type 2 diabetes mellitus (T2DM) druggable targets and drugs targeting them
Molecular Diversity (2025)
-
Factors influencing the initial glycemic efficacy of dorzagliatin, a novel glucokinase activator, in type 2 diabetes
Endocrine (2025)
-
Clinical research progress on β-cell dysfunction in T2DM development in the Chinese population
Reviews in Endocrine and Metabolic Disorders (2025)