Abstract
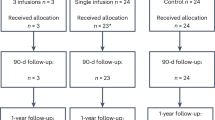
No therapy has been shown to reduce the risk of major adverse liver outcomes (MALO) in patients with cirrhosis due to metabolic dysfunction-associated steatohepatitis (MASH). The Surgical Procedures Eliminate Compensated Cirrhosis In Advancing Long-term (SPECCIAL) observational study compared the effects of metabolic surgery and nonsurgical treatment in patients with obesity and compensated histologically proven MASH-related cirrhosis. Using a doubly robust estimation methodology to balance key baseline characteristics between groups, the time-to-incident MALO was compared between 62 patients (68% female) who underwent metabolic surgery and 106 nonsurgical controls (71% female), with a mean follow-up of 10.0 ± 4.5 years. The 15 year cumulative incidence of MALO was 20.9% (95% confidence interval (CI), 2.5–35.9%) in the surgical group compared with 46.4% (95% CI, 25.6–61.3%) in the nonsurgical group, with an adjusted hazard ratio of 0.28 (95% CI, 0.12–0.64), P = 0.003. The 15 year cumulative incidence of decompensated cirrhosis was 15.6% (95% CI, 0–31.3%) in the surgical group compared with 30.7% (95% CI, 12.9–44.8%) in the nonsurgical group, with an adjusted hazard ratio of 0.20 (95% CI, 0.06–0.68), P = 0.01. Among patients with compensated MASH-related cirrhosis and obesity, metabolic surgery, compared with nonsurgical management, was associated with a significantly lower risk of incident MALO. In the absence of approved medical therapies for compensated MASH-related cirrhosis, metabolic surgery may represent a safe and effective therapeutic option to influence the trajectory of cirrhosis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The dataset generated during the current study is not publicly available to preserve patient confidentiality. However, the dataset is available from the corresponding author to academic investigators following receipt of a signed data-sharing agreement and after reviewing the study protocol (approved by a local institutional review board or research ethics committee), statistical analysis plan and publication plan. The CCHS institutional review board and the Law Department must approve the request before sharing the de-identified data. The corresponding author will respond to these requests within 2 months of receipt.
References
Diehl, A. M. & Day, C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. N. Engl. J. Med. 377, 2063–2072 (2017).
Sanyal, A. J. et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N. Engl. J. Med. 385, 1559–1569 (2021).
Abraldes, J. G., Caraceni, P., Ghabril, M. & Garcia-Tsao, G. Update in the treatment of the complications of cirrhosis. Clin. Gastroenterol. Hepatol. 21, 2100–2109 (2023).
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research. Nonalcoholic Steatohepatitis with Compensated Cirrhosis: Developing Drugs for Treatment. Guidance for Industry (Draft Guidance) https://www.fda.gov/media/127738/download (US FDA, 2019).
de Franchis, R. et al. Baveno VII—Renewing consensus in portal hypertension. J. Hepatol. 76, 959–974 (2022).
Kaplan, D. E. et al. AASLD practice guidance on risk stratification and management of portal hypertension and varices in cirrhosis. Hepatology 79, 1180–1211 (2024).
D’Amico, G., Garcia-Tsao, G. & Pagliaro, L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J. Hepatol. 44, 217–231 (2006).
Loomba, R., Ratziu, V. & Harrison, S. A. NASH Clinical Trial Design International Working Group Expert panel review to compare FDA and EMA guidance on drug development and endpoints in nonalcoholic steatohepatitis. Gastroenterology 162, 680–688 (2022).
Allen, A. M. et al. Clinical course of non-alcoholic fatty liver disease and the implications for clinical trial design. J. Hepatol. 77, 1237–1245 (2022).
Courcoulas, A. P. et al. Long-term outcomes of medical management vs bariatric surgery in type 2 diabetes. JAMA 331, 654–664 (2024).
Mingrone, G. et al. Metabolic surgery versus conventional medical therapy in patients with type 2 diabetes: 10-year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 397, 293–304 (2021).
Ikramuddin, S. et al. Lifestyle intervention and medical management with vs without Roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the Diabetes Surgery Study. JAMA 319, 266–278 (2018).
Verrastro, O. et al. Bariatric–metabolic surgery versus lifestyle intervention plus best medical care in non-alcoholic steatohepatitis (BRAVES): a multicentre, open-label, randomised trial. Lancet 401, 1786–1797 (2023).
Aminian, A. et al. Can nonalcoholic steatohepatitis be surgically cured?: liver histologic comparison after metabolic surgery versus usual care. Ann. Surg. 279, 276–282 (2024).
Lassailly, G. et al. Bariatric surgery provides long-term resolution of nonalcoholic steatohepatitis and regression of fibrosis. Gastroenterology 159, 1290–1301.e5 (2020).
Vuppalanchi, R. et al. Safety and efficacy of bariatric surgery in cirrhosis patients with extreme obesity. Ann. Surg. 275, e174–e180 (2022).
Funk, M. J. et al. Doubly robust estimation of causal effects. Am. J. Epidemiol. 173, 761–767 (2011).
Thomas, L. E., Li, F. & Pencina, M. J. Overlap weighting: a propensity score method that mimics attributes of a randomized clinical trial. JAMA 323, 2417–2418 (2020).
Li, F., Morgan, K. L. & Zaslavsky, A. M. Balancing covariates via propensity score weighting. J. Am. Stat. Assoc. 113, 390–400 (2018).
Heinze, G. & Schemper, M. A solution to the problem of monotone likelihood in Cox regression. Biometrics 57, 114–119 (2001).
Aminian, A. et al. Association of bariatric surgery with major adverse liver and cardiovascular outcomes in patients with biopsy-proven nonalcoholic steatohepatitis. JAMA 326, 2031–2042 (2021).
Khajeh, E. et al. Outcomes of bariatric surgery in patients with obesity and compensated liver cirrhosis. Surg. Obes. Relat. Dis. 18, 727–737 (2022).
Tapper, E. B., Ufere, N. N., Huang, D. Q. & Loomba, R. Review article: current and emerging therapies for the management of cirrhosis and its complications. Aliment. Pharmacol. Ther. 55, 1099–1115 (2022).
Harrison, S. A., Allen, A. M., Dubourg, J., Noureddin, M. & Alkhouri, N. Challenges and opportunities in NASH drug development. Nat. Med. 29, 562–573 (2023).
Loomba, R. et al. Semaglutide 2.4 mg once weekly in patients with non-alcoholic steatohepatitis-related cirrhosis: a randomised, placebo-controlled phase 2 trial. Lancet Gastroenterol. Hepatol. 8, 511–522 (2023).
Harrison, S. A. et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J. Hepatol. 73, 26–39 (2020).
Harrison, S. A. et al. Simtuzumab is ineffective for patients with bridging fibrosis or compensated cirrhosis caused by nonalcoholic steatohepatitis. Gastroenterology 155, 1140–1153 (2018).
Abdelmalek, M. F. et al. Pegbelfermin in patients with nonalcoholic steatohepatitis and compensated cirrhosis (FALCON 2): a randomized phase 2b study. Clin. Gastroenterol. Hepatol. 22, 113–123.e9 (2024).
Rinella, M. E. et al. AASLD practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 77, 1797–1835 (2023).
Brandman, D. Obesity management of liver transplant waitlist candidates and recipients. Clin. Liver Dis. 25, 1–18 (2021).
Sharpton, S. R., Terrault, N. A. & Posselt, A. M. Outcomes of sleeve gastrectomy in obese liver transplant candidates. Liver Transpl. 25, 538–544 (2019).
Idriss, R. et al. Impact of prior bariatric surgery on perioperative liver transplant outcomes. Liver Transpl. 25, 217–227 (2019).
Jastreboff, A. M. et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 387, 205–216 (2022).
Wadden, T. A. et al. Tirzepatide after intensive lifestyle intervention in adults with overweight or obesity: the SURMOUNT-3 phase 3 trial. Nat. Med. 29, 2909–2918 (2023).
Garvey, W. T. et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat. Med. 28, 2083–2091 (2022).
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: introducing the E-value. Ann. Intern. Med. 167, 268–274 (2017).
Kleiner, D. E. et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41, 1313–1321 (2005).
Ishak, K. et al. Histological grading and staging of chronic hepatitis. J. Hepatol. 22, 696–699 (1995).
Ross, M. K., Sanz, J., Tep, B., Follett, R., Soohoo, S. L. & Bell, D. S. Accuracy of an electronic health record patient linkage module evaluated between neighboring academic health care centers. Appl. Clin. Inform. 11, 725–732 (2020).
Pocock, S. J., Clayton, T. C. & Altman, D. G. Survival plots of time-to-event outcomes in clinical trials: good practice and pitfalls. Lancet 359, 1686–1689 (2002).
Altman, D. G. & Andersen, P. K. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ 319, 1492–1495 (1999).
Austin, P. C. Absolute risk reductions and numbers needed to treat can be obtained from adjusted survival models for time-to-event outcomes. J. Clin. Epidemiol. 63, 46–55 (2010).
van Buuren, S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 16, 219–242 (2007).
Rubin, D. B. Inference and missing data. Biometrika 63, 581–592 (1976).
Acknowledgements
We acknowledge M. E. Satava and R. Burton, both from Cleveland Clinic, for their help in collecting some of the data. These individuals received no additional compensation, outside of their usual salary, for their contributions.
Author information
Authors and Affiliations
Contributions
A. Aminian, R.L., A.J.S., N.A. and S.D. contributed to the study concept and design. A. Aminian, A. Aljabri, S.W., D.S.A., H.R., E.A., R.W. and A.M. were involved in data acquisition. J.B. performed the statistical analysis. All authors contributed to the interpretation of data. A. Aminian prepared the first draft of the paper. All authors critically revised the paper for intellectual content and clarity and approved the final version for submission. A. Aminian and S.E.N. provided the administrative support and supervised this work.
Corresponding author
Ethics declarations
Competing interests
A. Aminian reported receiving research grants from Medtronic and Ethicon. He serves as a consultant for Medtronic, Ethicon and Eli Lilly. R.L. serves as a consultant or advisory board member for 89Bio, Alnylam, Arrowhead Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Cirius, CohBar, DiCerna, Galmed, Gilead, Glympse Bio, Intercept, Ionis, Metacrine, NGM Biopharmaceuticals, Novo Nordisk, Pfizer, Sagimet and Viking Therapeutics. In addition, his institution has received grant support from Allergan, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Galmed Pharmaceuticals, Genfit, Gilead, Intercept, Inventiva, Janssen, Madrigal Pharmaceuticals, NGM Biopharmaceuticals, Novartis, Pfizer, pH Pharma and Siemens. He is also cofounder of Liponexus. A.J.S. has stock options in Genfit, Tiziana, Indalo, Durect, Inversago and Galmed. He has served as a consultant to AstraZeneca, Salix, Tobira, Takeda, Janssen, Gilead, Terns, Merck, Madrigal, NGM Biopharmaceuticals, Sagimet, Valeant, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Hemoshear, Novartis, Inventiva, Enyo, Akero, 89Bio, Novo Nordisk, Pfizer, Amgen, Genentech, Regeneron, Alnylam, Hanmi, LG Chem, Histoindex, Theratechnologies, Intercept, Target-RWE, Surrozen, Zydus, Path AI, Exhalenz and Genfit. His institution has received grant support from Gilead, Salix, Tobira, Bristol Myers Squibb, Pfizer, Intercept, Merck, AstraZeneca, Malinckrodt and Novartis. He receives royalties from Elsevier and UptoDate. N.A. has received research funding from 89Bio, Akero, AbbVie/Allergan, Better Therapeutics, Boehringer Ingelheim, Bristol Myers Squibb, Corcept, Galectin, Genentech, Genfit, Gilead, Healio, Hepagene, Intercept, Inventiva, Ionis, Madrigal, Merck, NGM, Noom, NorthSea, Novo Nordisk, Perspectum, Pfizer, Poxel, Viking and Zydus; has attended speaker bureaus for AbbVie/Allergan, Alexion, Echosens, Eisai, Exelixis, Gilead, Intercept, Perspectum, Salix and Theratechnologies; and has acted as a consultant for AbbVie/Allergan, Echosens, Gilead, Intercept, Madrigal, Novo Nordisk, Perspectum, Pfizer and Zydus. S.E.N. reported receiving grants to perform clinical trials from AbbVie, AstraZeneca, Amgen, Bristol Myers Squibb, Eli Lilly, Esperion Therapeutics Inc, Medtronic, MyoKardia, New Amsterdam Pharmaceuticals, Novartis and Silence Therapeutics. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Hao Ma, Geltrude Mingrone, Eric Sheu, Raj Vuppalanchi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Michael Basson, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Cumulative incidence estimates of major adverse liver outcomes in the overlap-weighted patients.
A Kaplan Meier graph shows the cumulative incidence of the primary composite endpoint, incident MALO, in the nonsurgical control group and separately after Roux-en-Y gastric bypass and sleeve gastrectomy. P value is for overall 2-sided comparison of 3 groups from the Cox proportional hazards model.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aminian, A., Aljabri, A., Wang, S. et al. Long-term liver outcomes after metabolic surgery in compensated cirrhosis due to metabolic dysfunction-associated steatohepatitis. Nat Med 31, 988–995 (2025). https://doi.org/10.1038/s41591-024-03480-y
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41591-024-03480-y