Abstract
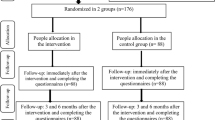
Conflicting study outcomes on women undergoing cesarean sections underscore the complex relationship between repeated cesarean deliveries and factors such as sense of coherence, self-efficacy, and anxiety, highlighting the need for empowerment-based interventions to improve mothers’ mental health and parenting outcomes. This randomized controlled trial aimed to evaluate an educational program based on the self-management empowerment model on sense of coherence, self-efficacy, and postpartum anxiety in cesarean mothers. In 2024, 98 women scheduled for cesarean delivery at Shohada-ye-Khalij-e-Fars Hospital, Bushehr, Iran, were selected by convenience sampling and randomly assigned via block randomization to intervention (n = 49) or control (n = 49) groups. The intervention group received a five-step education program over two months. Antonovsky’s Sense of Coherence Questionnaire, Sherer’s Self-Efficacy Scale, and Spielberger Anxiety Questionnaire were administered pre- and post-intervention. Data were analyzed using SPSS version 27 with descriptive/inferential statistics (p < 0.05). Mean changes showed significant intervention effects: self-efficacy − 1.58 ± 7.31 (control) versus 2.79 ± 6.42 (intervention, ŋ2 = 0.151, p < 0.001); sense of coherence 2.67 ± 8.36 (control) versus 4.81 ± 6.58 (intervention, ŋ2 = 0.073, p = 0.018); anxiety 0.02 ± 15.99 (control) versus − 13.07 ± 13.7 (intervention, ŋ2 = 0.224, p < 0.001). The self-management empowerment model significantly improved sense of coherence and self-efficacy while reducing postpartum anxiety, recommending its integration into postpartum care programs.
Trial Registration http://www.irct.ir/, IRCTID: IRCT20130422013092N12 registered July 11, 2024.
Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- CS:
-
Cesarean section
- CONSORT:
-
Consolidated standards of reporting trials
- PTSD:
-
Post-traumatic stress disorder
- RCT:
-
Randomized controlled trial
- SOC:
-
Sense of coherence
- SES:
-
Socioeconomic status
- WHO:
-
World Health Organization
References
Downe, S., Calleja Agius, J., Balaam, M.-C. & Frith, L. Understanding childbirth as a complex salutogenic phenomenon: The EU COST BIRTH action special collection. PLoS ONE 15(8), e0236722 (2020).
Omidvar, B. & Liraviani, N. S. A causal explanation of maternal sense of competency: The study role of parental self-efficacy of mothers and cognitive emotion regulation strategies. Q. J. Woman Soc. 9(36), 1–16 (2019).
Maryami, F., Maryami, Z., Bigdeli, I., Najafi, M. & Kiani, M. The role of social support and personality traits in the incidence of postpartum depression. J. Gorgan Univ. Med. Sci. 22(1), 88–94 (2020).
Dennis, C.-L., Coghlan, M. & Vigod, S. Can we identify mothers at-risk for postpartum anxiety in the immediate postpartum period using the State-Trait Anxiety Inventory?. J. Affect. Disord. 150(3), 1217–1220 (2013).
Field, T. Postpartum anxiety prevalence, predictors and effects on child development: A review. J. Psychiatr. Psychiatr. Disord. 1(2), 86–102 (2017).
Wenzel, A., Haugen, E., Jackson, L. & Robinson, K. Prevalence of generalized anxiety at eight weeks postpartum. Arch. Womens Ment. Health 6(1), 43–49 (2003).
Janssen, A. B. et al. Persistence of anxiety symptoms after elective caesarean delivery. BJPsych Open 4(5), 354–360 (2018).
Dekel, S. et al. Delivery mode is associated with maternal mental health following childbirth. Arch. Womens Ment. Health 22(6), 817–824 (2019).
Chen, Y. et al. Prevalence of post-traumatic stress disorder following caesarean section: a systematic review and meta-analysis. J. Womens Health 29(2), 200–209 (2020).
Orovou, E., Antoniou, E., Zervas, I. & Sarantaki, A. Prevalence and correlates of postpartum PTSD following emergency cesarean sections: implications for perinatal mental health care: A systematic review and meta-analysis. BMC Psychol. 13(1), 26 (2025).
Chuektong, C., Nirattharadorn, M. & Buaboon, N. The breastfeeding self-efficacy enhancement program with LINE application among mothers with cesarean section: A quasi-experimental study. Pac. Rim Int. J. Nurs. Res. 27(4), 711–721 (2023).
Fallon, V., Groves, R., Halford, J. C. G., Bennett, K. M. & Harrold, J. A. Postpartum anxiety and infant-feeding outcomes: A systematic review. J. Hum. Lact. 32(4), 740–758 (2016).
Kuo, S.-Y., Chen, S.-R. & Tzeng, Y.-L. Depression and anxiety trajectories among women who undergo an elective cesarean section. PLoS ONE 9(1), e86653 (2014).
Gutiérrez, N. O. et al. The effects of accompaniment on maternal anxiety during elective cesarean delivery: A quasi-experimental study. Matern. Child Health J. 27(8), 1352–1360 (2023).
Sharifi, S., Niknami, M., Bostani Khalesi, Z., Maroufizadeh, S. & Haji, H. F. Effect of auriculotherapy on the anxiety of women after cesarean section: A clinical trial. J. Holist. Nurs. Midwifery 34(1), 3–12 (2024).
Maluka, S. O. & Peneza, A. K. Perceptions on male involvement in pregnancy and childbirth in Masasi District, Tanzania: A qualitative study. Reprod. Health 15(1), 68 (2018).
Tehrani, G. Evaluation of effect of postpartum care education based on maternal educational needs on knowledge of postpartum care. Nurs. Midwifery J. 15(2), 76–85 (2017).
Asadi, M., Tabari, F., Haghani, S., Ghadirian, F. The effect of education based on empowerment model on anxiety among transsexual clients undergoing hormone therapy (2019).
Forster, D. A., McLachlan, H. L. & Lumley, J. Factors associated with breastfeeding at six months postpartum in a group of Australian women. Int. Breastfeed. J. 1(1), 18 (2006).
Cunqueiro, M., Comeche, M. I., Docampo, D. Self-efficacy, use of coping behavior strategies and experience of childbirth in low-risk pregnancy. August) doi, 10 (2017).
Heydarpour, S., Keshavarz, Z. & Bakteari, M. Factors affecting maternal role adaptation in mothers of preterm infants hospitalized in the intensive care unit: A qualitative study. J. Qualit. Res. Health Sci. 6(2), 134–146 (2017).
Farley, H. Promoting self-efficacy in patients with chronic disease beyond traditional education: A literature review. Nurs. Open 7(1), 30–41 (2020).
Dilks, F. M. & Beal, J. A. Role of self-efficacy in birth choice. J. Perinat. Neonatal Nurs. 11(1), 1–9 (1997).
Loto, O. M. et al. Cesarean section in relation to self-esteem and parenting among new mothers in southwestern Nigeria. Acta Obstet. Gynecol. Scand. 89(1), 35–38 (2010).
Supliyani, E., Handayani, I., Pramanik, N. D., Suarniti, N. W. The effectiveness of postpartum education and support models in enhancing mothers’ self-efficacy after cesarean section. Healthc. Low Resour. Settings 13 (2025).
Möllerberg, M.-L., Årestedt, K., Swahnberg, K., Benzein, E. & Sandgren, A. Family sense of coherence and its associations with hope, anxiety and symptoms of depression in persons with cancer in palliative phase and their family members: A cross-sectional study. Palliat. Med. 33(10), 1310–1318 (2019).
Urakawa, K., Yokoyama, K. & Itoh, H. Sense of coherence is associated with reduced psychological responses to job stressors among Japanese factory workers. BMC. Res. Notes 5(1), 247 (2012).
Braun-Lewensohn, O. & Sagy, S. Community resilience and sense of coherence as protective factors in explaining stress reactions: Comparing cities and rural communities during missiles attacks. Community Ment. Health J. 50(2), 229–234 (2014).
Oz, Y., Sarid, O., Peleg, R. & Sheiner, E. Sense of coherence predicts uncomplicated delivery: A prospective observational study. J. Psychosom. Obstet. Gynecol. 30(1), 29–33 (2009).
Ferguson, S., Davis, D., Browne, J. & Taylor, J. Sense of coherence and childbearing: A scoping review of the literature. Int. J. Childbirth 4(3), 134 (2014).
Organization WH. WHO Recommendations on Intrapartum Care for a Positive Childbirth Experience: World Health Organization (2018).
Antonovsky, A. Health, stress, and coping. New Perspect. Ment. Phys. Well-being 12–37 (1979).
Becker C. Salutogenesis 30 Years Later: Where do we go from here? (2010).
Asplund, D. et al. Pretreatment quality of life in patients with rectal cancer is associated with intrusive thoughts and sense of coherence. Int. J. Colorectal Dis. 32(11), 1639–1647 (2017).
Heydari, F., Nikfarid, L., Oujian, P., Nasiri, M. & Motefakker, S. Predictors of perceived family sense of coherence in parents of children with cancer. Indian J. Palliat. Care 28(1), 28 (2022).
Jörgensen, S., Ginis, K. A. M., Iwarsson, S. & Lexell, J. Depressive symptoms among older adults with long-term spinal cord injury: Associations with secondary health conditions, sense of coherence, coping strategies and physical activity. J. Rehabil. Med. 49(8), 644–651 (2017).
Keil, D. C., Vaske, I., Kenn, K., Rief, W. & Stenzel, N. M. With the strength to carry on: the role of sense of coherence and resilience for anxiety, depression and disability in chronic obstructive pulmonary disease. Chron. Respir. Dis. 14(1), 11–21 (2017).
Egger, J. W. Integrative Verhaltenstherapie und Psychotherapeutische Medizin: Ein Biopsychosoziales Modell (Springer, 2015).
Kröninger-Jungaberle, H. & Grevenstein, D. Development of salutogenetic factors in mental health-Antonovsky’s sense of coherence and Bandura’s self-efficacy related to Derogatis’ symptom check list (SCL-90-R). Health Qual. Life Outcomes 11(1), 80 (2013).
Mato, M. & Tsukasaki, K. Factors promoting sense of coherence among university students in urban areas of Japan: Individual-level social capital, self-efficacy, and mental health. Glob. Health Promot. 26(1), 60–68 (2019).
Alcantara, J., Myers, S., Emmanuel, E., Grace, S. Sense of coherence in pregnancy: A systematic review of the literature (2023).
Baldwin, S., Malone, M., Sandall, J. & Bick, D. Mental health and wellbeing during the transition to fatherhood: A systematic review of first time fathers’ experiences. JBI Evid. Synth. 16(11), 2118–2191 (2018).
Koelen, M. & Lindström, B. Making healthy choices easy choices: The role of empowerment. Eur. J. Clin. Nutr. 59(1), S10–S16 (2005).
Leidy, N. K. & Haase, J. E. Functional status from the patient’s perspective: the challenge of preserving personal integrity. Res. Nurs. Health 22(1), 67–77 (1999).
Hourzad, A., Pouladi, S., Ostovar, A. & Ravanipour, M. The effects of an empowering self-management model on self-efficacy and sense of coherence among retired elderly with chronic diseases: A randomized controlled trial. Clin. Interv. Aging 13, 2215–2224 (2018).
Khezri, R., Ravanipour, M., Motamed, N., Vahedparast, H. Effect of self-management empowering model on the quality of life in the elderly patients with hypertension. IRANIAN JOURNAL OF AGEING. 10(4), 68-79. https://sid.ir/paper/95210/en. (2016).
Ravanipour, M. et al. Power resources of older people in Iran. Int. J. Older People Nurs. 8(1), 71–79 (2013).
de Loenzien, M., Mac, Q. N. H. & Dumont, A. Women’s empowerment and elective cesarean section for a single pregnancy: A population-based and multivariate study in Vietnam. BMC Pregnancy Childbirth 21(1), 3 (2021).
Khanum, S. et al. Mental health of mothers after natural childbirth and cesarean section: A comparative study in Kohat, Khyber Pakhtunkhwa, Pakistan. Texto Contexto-Enfermagem 31, e20220140 (2022).
Li, L., Wan, W. & Zhu, C. Breastfeeding after a cesarean section: A literature review. Midwifery 103, 103117 (2021).
Zlakowska, P. Fear of childbirth and sense of coherence with their determinants in endangered and healthy pregnancies. J. Pre-Clin. Clin. Res. 14(3), 90–93 (2020).
Dikmen-Yildiz, P., Ayers, S. & Phillips, L. Factors associated with post-traumatic stress symptoms (PTSS) 4–6 weeks and 6 months after birth: A longitudinal population-based study. J. Affect. Disord. 221, 238–245 (2017).
Sherer, M. et al. The self-efficacy scale: Construction and validation. Psychol. Rep. 51(2), 663–671 (1982).
Najafi, M. & Foladjang, M. The relationship between self-efficacy and mental health among high school students. Clin. Psychol. Personal. 5(1), 69–82 (2007).
Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 36(6), 725–733 (1993).
Mahammadzadeh, A., Poursharifi, H. & Alipour, A. Validation of Sense of Coherence (SOC) 13-item scale in Iranian sample. Procedia Soc. Behav. Sci. 5, 1451–1455 (2010).
Safavi, M. & Marofi, S. Correlation between attachment styles and state-or trait-anxiety. Med. Sci. J. Islamic Azad Univ.-Tehran Med. Branch 22(4), 307–312 (2012).
Taqavi, M., Najafi, M., Kianersi, F. & Aqayan, S. Comparing of alexithymia, defensive styles and state-trait anxiety among patients with generalized anxiety disorder major depression disorder and normal individuals. J. Clin. Psychol. 5(2), 67–76 (2013).
Chen, D., Lang, B., Wu, L., Zhou, S. & Chen, S. Early oral feeding within two hours for parturients compared with delayed oral feeding after cesarean section: A systematic review and meta-analysis. BMC Pregnancy Childbirth 24(1), 623 (2024).
Granberg, A., Ekström-Bergström, A. & Bäckström, C. First-time mothers’ enjoyment of breastfeeding correlates with duration of breastfeeding, sense of coherence, and parental couple and child relation: a longitudinal Swedish cohort study. Nutr. Res. Pract. 2020(1), 8194389 (2020).
Kekäläinen, T., Kokko, K., Sipilä, S. & Walker, S. Effects of a 9-month resistance training intervention on quality of life, sense of coherence, and depressive symptoms in older adults: Randomized controlled trial. Qual. Life Res. 27(2), 455–465 (2018).
Musavinasab, M., Ravanipour, M., Pouladi, S., Motamed, N. & Barekat, M. The effect of self-management empowerment model on the sense of coherence among elderly patients with cardiovascular disease. Educ. Gerontol. 42(2), 100–108 (2016).
Ngai, F. W. & Chan, P. S. Perception of family sense of coherence during parental transition: A qualitative study. J. Health Psychol. 26(13), 2435–2449 (2021).
Pakkala, I. et al. Effects of intensive strength-power training on sense of coherence among 60–85-year-old people with hip fracture: A randomized controlled trial. Aging Clin. Exp. Res. 24(3), 295–299 (2012).
Olza, I. et al. Women’s psychological experiences of physiological childbirth: a meta-synthesis. BMJ Open 8(10), e020347 (2018).
Abd El-Kader, A. I. Effectiveness of childbirth self-efficacy enhancing classes on labor length and outcomes among egyptian primiparous women: A quasi-experimental study. SAGE Open Nurs. 10, 23779608241288756 (2024).
Farasati, M. et al. The effect of in-home supportive counseling on maternal functioning and self-efficacy following cesarean section among primiparous women. J. Educ. Health Promot. 13(1), 26 (2024).
Mohseni, H. et al. An investigation into the effects of prenatal care instruction at home on breast-feeding self-efficacy of first-time pregnant women referred to shiraz clinics, Iran. Int. J. Women’s Health Reproduct. Sci. 6(1), 41–46 (2018).
Azizah, N., Rosyidah, R. & Jayanti, R. D. Improving parenting self-efficacy in post-partum sectio caesarea. J. Midpro. 14(2), 176–181 (2022).
Moattari, M., Ebrahimi, M., Sharifi, N. & Rouzbeh, J. The effect of empowerment on the self-efficacy, quality of life and clinical and laboratory indicators of patients treated with hemodialysis: A randomized controlled trial. Health Qual. Life Outcomes 10(1), 115 (2012).
Bandura, A. Social foundations of thought and action. Englewood Cliffs NJ 1986(23–28), 2 (1986).
Gao, L.-l, Sun, K. & Chan, S.W.-C. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery 30(5), 532–538 (2014).
Kellams, A. L. et al. The impact of a prenatal education video on rates of breastfeeding initiation and exclusivity during the newborn hospital stay in a low-income population. J. Hum. Lact. 32(1), 152–159 (2016).
Botha, E., Helminen, M., Kaunonen, M., Lubbe, W. & Joronen, K. Mothers’ parenting self-efficacy, satisfaction and perceptions of their infants during the first days postpartum. Midwifery 88, 102760 (2020).
Agarwal, R. Management of hypertension in hemodialysis patients. Hemodial. Int. 10(3), 241–248 (2006).
Arfaie, K., Nahidi, F., Simbar, M., Bakthiari, M. Parenting challenges and pregnancy induced anxiety: A qualitative study (2017).
Gandomi, N., Sharifzadeh, G., Torshizi, M. & Norozi, E. The effect of educational intervention based on self-efficacy theory on pregnancy anxiety and childbirth outcomes among Iranian primiparous women. J. Educ. Health Promot. 11, 14 (2022).
Kharazi, S. S., Peyman, N. & Esmaily, H. Effect of an educational intervention based on self-efficacy theory and health literacy strategies on pregnancy outcomes: a randomized clinical trial. Iran. J. Obstet. Gynecol. Infertil. 21(5), 33–46 (2018).
Kuo, T.-C. et al. Effects of an integrated childbirth education program to reduce fear of childbirth, anxiety, and depression, and improve dispositional mindfulness: A single-blind randomised controlled trial. Midwifery 113, 103438 (2022).
Mohammadi, F., Kohan, S., Farzi, S., Khosravi, M. & Heidari, Z. The effect of pregnancy training classes based on bandura self-efficacy theory on postpartum depression and anxiety and type of delivery. J. Educ. Health Promot. 10, 273 (2021).
Kohan, S., Heidari, Z. & Keshvari, M. Iranian Women’s experiences of breastfeeding support: A qualitative study. J. Pediatr. Perspect. 4(10), 3587–3600 (2016).
Kohan, S., Keshvari, M., Mohammadi, F. & Heidari, Z. Designing and evaluating an empowering program for breastfeeding: A mixed-methods study. Arch. Iran. Med. 22(8), 443–452 (2019).
Missler, M., van Straten, A., Denissen, J., Donker, T. & Beijers, R. Effectiveness of a psycho-educational intervention for expecting parents to prevent postpartum parenting stress, depression and anxiety: A randomized controlled trial. BMC Pregnancy Childbirth 20(1), 658 (2020).
Henshaw, E. J. et al. “Trying to figure out if you’re doing things right, and where to get the info”: Parents recall information and support needed during the first 6 weeks postpartum. Matern. Child Health J. 22(11), 1668–1675 (2018).
Liberska, H. & Deja, M. Satisfaction with life, emotions, and identity processes in Polish first-time mothers and fathers and their child’s age. Int. J. Environ. Res. Public Health 18(2), 799 (2021).
Nomaguchi, K. & Milkie, M. A. Parenthood and well-being: A decade in review. J. Marriage Fam. 82(1), 198–223 (2020).
Acknowledgements
The present manuscript was extracted from the Master’s thesis by Fariba Najafi ShahaliBegloo, Faculty of Nursing and Midwifery of Bushehr University of Medical Sciences, Bushehr, Iran. The study was approved by the Research Council and the Research Ethics Committee (code: (IR.BPUMS.REC.1403.102)) of Bushehr University of Medical Sciences, Bushehr, Iran. The study protocol was registered at the Iranian Registry of Clinical Trials (registration number: IRCT20130422013092N12). We would like to thank the Deputy of Research at Bushehr University of Medical Sciences for the financial support. We would like to express our gratitude to the local authorities for their support and all mothers who participated in this study for their active participation in the study.
Funding
This work was supported by the Research Council of Bushehr University of Medical Sciences (Grant Number: IR.BPUMS.REC.1403.102). The Research Council of Bushehr University of Medical Sciences had no role in conducting the study, data analysis or interpretation, writing the manuscript, or decisions about submitting the script for publication.
Author information
Authors and Affiliations
Contributions
The contribution of the authors to the research was as follows: Research design by MR, FK, SM, FN; data collection by FN; research execution by MR, FK, SM, FN; data analysis by SM; documentation by MR, FK, SM, FN; and primary responsibility for the final content by MR, FK, SM, FN. All authors were major contributions in writing the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Najafi ShahaliBegloo, F., Kamali, F., Mohamadi, S. et al. Assessment of self-management empowerment program on sense of coherence, self-efficacy and postpartum anxiety in cesarean mothers randomized trial. Sci Rep (2026). https://doi.org/10.1038/s41598-026-37944-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-37944-7