Abstract
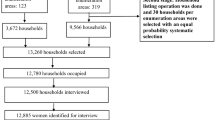
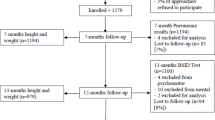
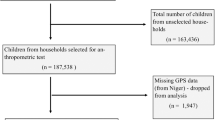
Household air pollution (HAP) is a major environmental health risk globally and is strongly associated with adverse child health outcomes, including neonatal, infant, and under-five mortality. Household environmental conditions such as water source, sanitation, cooking fuel type, and housing materials (roofing and walling) influence exposure levels and subsequent health risks. While there is robust global evidence linking HAP to poor child health outcomes, evidence from Sub-Saharan Africa (SSA) remains comparatively limited, despite the region bearing a disproportionately high burden of solid fuel use and child mortality. This gap constrains a comprehensive understanding of the magnitude and contextual drivers of HAP-related risks among children in SSA. We investigated the association between HAP due to household environmental variables (source of water, sanitation, type of cooking fuel, roofing materials, walling material etc.) and selected child health outcomes (neonatal, infant, ARI and under five mortality) in 32 Sub-Saharan Africa (SSA) countries. In all we analyzed Demographic and Health Survey (DHS) data from 362,072 children under the age of five, applying complex survey design features including stratification, clustering, and sampling weights. HAP exposure was defined using quantile distribution and summarized into Household Air Pollution Index through principal component analysis, categorized as “unexposed”, “moderate exposure” and “high exposure”. Associations were estimated using Poisson regression models with a robust variance adjusting for confounding variables and survey design effects. Approximately two-thirds (65%) children under-five were exposed to HAP, with the highest exposures in Central (71%) and West Africa (67%). Over the study decade, mortality rates were under five (92 per 1000 live births), infants (52 per 1000 live births), and neonatal (28 per 1000 live births). Exposure to HAP was associated with increased risk of under-five mortality (aRR: 1.3; 95% CI: 1.19, 1.46; p = 0.001) and infant mortality (aRR: 1.4; 95% CI: 1.28, 1.60; p = 0.001). Children with high exposure to HAP had a higher mortality risk than the unexposed (aRR: 1.10; 95% CI: 0.91–1.33; p = 0.032). Our findings demonstrate that HAP significantly contributes to infants, ARI and under five mortalities in SSA. Given the heavy reliance on solid fuels in low-resource settings, urgent government action is needed to reduce solid fuel use, improve household sanitation, expand access to clean water, and reconsider housing materials to protect child health.
Similar content being viewed by others
Data availability
The household survey data analysed in this study are publicly available from the Demographic and Health Surveys (DHS) Program ( [https://dhsprogram.com](https:/dhsprogram.com) ) upon registration and approval. Researchers seeking access to the datasets used in this analysis should submit a data request directly through the DHS Program. Further information regarding the specific survey datasets applied is available from the corresponding author upon reasonable request.
References
Pun, V. C., Dowling, R. & Mehta, S. Ambient and household air pollution on early-life determinants of stunting—a systematic review and meta-analysis. Environ. Sci. Pollut Res. 28, 26404–26412 (2021).
IHME. GBD Compare (University of Washington, 2021).
Global burden. Of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1223–1249 (2020).
Tawiah, T. et al. The association between household air pollution and blood pressure in Obuasi municipality. Ghana. Atmosphere 13,12, 2033 (2022).
McCracken, J. P. et al. Household air pollution from solid fuel use: evidence for links to CVD. Glob Heart. 7, 223–234 (2012).
Po, J. Y., FitzGerald, J. M. & Carlsten, C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax 66, 232–239 (2011).
Torres-Duque, C., Maldonado, D., Pérez-Padilla, R., Ezzati, M. & Viegi, G. Biomass fuels and respiratory diseases: a review of the evidence. Proc. Am. Thorac. Soc. 5, 577–590 (2008).
Agrawal, S. & Yamamoto, S. Effect of indoor air pollution from biomass and solid fuel combustion on symptoms of preeclampsia/eclampsia in Indian women. Indoor Air. 25, 341–352 (2015).
Lai, J. et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 3, e203976 (2020).
WHO. Air Pollution and Child Health: Prescribing Clean Air: Summary (World Health Organization, 2018).
UNICEF. Clear the Air for Children. (2016).
UNICEF. One is Too Many: Ending Child Deaths from Pneumonia and Diarrhea. (2016).
He, C. et al. Fine particulate matter air pollution and under-5 children mortality in china: A National time-stratified case-crossover study. Environ. Int. 159, 107022 (2022).
Greenhalgh, T. Cultural Contexts of Health: the Use of Narrative Research in the Health Sector (World Health Organization, 2016).
Balidemaj, F., Isaxon, C., Abera, A. & Malmqvist, E. Indoor air pollution exposure of women in Adama, Ethiopia, and assessment of disease burden attributable to risk factor. Int. J. Environ. Res. Public. Health. 18, 9859 (2021).
Corsi, D. J., Neuman, M., Finlay, J. E. & Subramanian, S. Demographic and health surveys: a profile. Int. J. Epidemiol. 41, 1602–1613 (2012).
Pillarisetti, A., Ye, W. & Chowdhury, S. Indoor air pollution and health: bridging perspectives from developing and developed countries. Annu. Rev. Environ. Resour. 47, 197–229 (2022).
Chowdhury, S. et al. Global and regional health effects of household air pollution and the burden of disease. Environ. Health Perspect. 130, 46001 (2022).
Kodgule, R. & Salvi, S. Exposure to biomass smoke as a cause for airway disease in women and children. Curr. Opin. Allergy Clin. Immunol. 12, 82–90 (2012).
Rana, J., Islam, R. M., Khan, M. N., Aliani, R. & Oulhote, Y. Association between household air pollution and child mortality in Myanmar using multilevel mixed-effects Poisson regression. Sci. Rep. 11, 1–10 (2021).
Fullerton, D. G., Bruce, N. & Gordon, S. B. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans. R Soc. Trop. Med. Hyg. 102, 843–851 (2008).
Rana, J., Uddin, J., Peltier, R. & Oulhote, Y. Associations between indoor air pollution and acute respiratory infections among under-five children in afghanistan: do SES and sex matter? Int. J. Environ. Res. Public. Health. 16, 2910 (2019).
Kleimola, L. B., Patel, A. B., Borkar, J. A. & Hibberd, P. L. Consequences of household air pollution on child survival: evidence from demographic and health surveys in 47 countries. Int. J. Occup. Environ. Health. 21, 294–302 (2015).
Piddock, K. C. et al. A cross-sectional study of household biomass fuel use among a Periurban population in Malawi. Ann. Am. Thorac. Soc. 11, 915–924 (2014).
James, B. S., Shetty, R. S., Kamath, A. & Shetty, A. Household cooking fuel use and its health effects among rural women in Southern India. PLoS One. 15, e0231757 (2020).
Tipre, M. et al. Prenatal exposure to particulate matter (PM2.5) from biomass fuel and low birth weight in a Sri Lankan birth cohort. bioRxiv (2019).
Kiross, G. T., Chojenta, C., Barker, D., Tiruye, T. Y. & Loxton, D. The effect of maternal education on infant mortality in ethiopia: a systematic review and meta-analysis. PLoS One. 14, e0220076 (2019).
Chafe, Z. A. et al. Household cooking with solid fuels contributes to ambient PM2.5 air pollution and the burden of disease. Environ. Health Perspect. 122, 1314–1320 (2014).
Zarulli, V. & Salinari, G. Gender differences in survival across the ages of life: an introduction. Genus 80, 10 (2024).
Costa, J. C., da Silva, I. C. M. & Victora, C. G. Gender bias in under-five mortality in low/middle-income countries. BMJ Glob Health. 2, e000347 (2017).
Chao, F. et al. Sex differences in mortality among children, adolescents, and young people aged 0–24 years: a systematic assessment of national, regional, and global trends from 1990–2021. Lancet Glob Health. 11, e1519–e1530 (2023).
Biradar, R., Patel, K. K. & Prasad, J. B. Effect of birth interval and wealth on under-5 child mortality in Nigeria. Clin. Epidemiol. Glob Health. 7, 234–238 (2019).
Boettiger, D. C. et al. Household factors and under-five mortality in Bankass, mali: results from a cross-sectional survey. BMC Public. Health. 21, 1–10 (2021).
Ekholuenetale, M., Wegbom, A. I., Tudeme, G. & Onikan, A. Household factors associated with infant and under-five mortality in sub-Saharan Africa countries. Int. J. Child. Care Educ. Policy. 14, 1–15 (2020).
Alam, M. B. et al. Household air pollution from cooking fuels and its association with under-five mortality in Bangladesh. Clin. Epidemiol. Glob Health. 17, 101134 (2022).
Amir-ud-Din, R., Kumar, R., Naeem, N. & Khan, M. Air pollution and under-5 child mortality: linking satellite and IPUMS-DHS data across 41 countries in South Asia and Sub-Saharan Africa. BMC Public. Health. 24, 2996 (2024).
Amegah, A. K., Quansah, R. & Jaakkola, J. J. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One. 9, e113920 (2014).
Mishra, V., Smith, K. R. & Retherford, R. D. Effects of cooking smoke and environmental tobacco smoke on acute respiratory infections in young Indian children. Popul. Environ. 26, 375–396 (2005).
Valavanidis, A., Fiotakis, K. & Vlachogianni, T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J. Environ. Sci. Health C. 26, 339–362 (2008).
Naz, S., Page, A. & Agho, K. E. Household air pollution from use of cooking fuel and under-five mortality: the role of breastfeeding status and kitchen location in Pakistan. PLoS One. 12, e0173256 (2017).
Smith, K. R., Samet, J. M., Romieu, I. & Bruce, N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax 55, 518–532 (2000).
Bickton, F. M. et al. Household air pollution and under-five mortality in sub-Saharan africa: an analysis of 14 demographic and health surveys. Environ. Health Prev. Med. 25, 1–11 (2020).
Amnuaylojaroen, T. & Parasin, N. Future health risk assessment of exposure to PM2.5 in different age groups of children in Northern Thailand. Toxics 11, 291 (2023).
Ravindra, K., Kaur-Sidhu, M., Mor, S. & John, S. Trend in household energy consumption pattern in india: a case study on the influence of socio-cultural factors for the choice of clean fuel use. J. Clean. Prod. 213, 1024–1034 (2019).
Le, M. H. et al. Global incidence of adverse clinical events in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Clin. Mol. Hepatol. 30, 235 (2024).
Singh, S. P. et al. Prenatal secondhand cigarette smoke promotes Th2 polarization and impairs goblet cell differentiation and airway mucus formation. J. Immunol. 187, 4542–4552. https://doi.org/10.4049/jimmunol.1101567 (2011).
He, Y. et al. Short-term effects and economic burden of air pollutants on acute lower respiratory tract infections in children in Southwest china: a time-series study. Environ. Health. 22, 1. https://doi.org/10.1186/s12940-023-00962-3 (2023).
Pająk, A., Szafrańska, A. & Królak-Olejnik, B. Early hypophosphatemia in very low birth weight preterm infants. Adv. Clin. Exp. Med. 27, 841–847. https://doi.org/10.17219/acem/70081 (2018).
Arigliani, M. et al. Lung function between 8 and 15 years of age in very preterm infants with fetal growth restriction. Pediatr. Res. 90, 657–663. https://doi.org/10.1038/s41390-020-01299-0 (2021).
Ngandu, C. B. et al. The association between household socio-economic status, maternal socio-demographic characteristics and adverse birth and infant growth outcomes in sub-Saharan africa: a systematic review. J. Dev. Orig Health Dis. 11, 317–334. https://doi.org/10.1017/s2040174419000680 (2019).
Khan, M. N. et al. Household air pollution from cooking and risk of adverse health and birth outcomes in bangladesh: a nationwide population-based study. Environ. Health. 16, 1. https://doi.org/10.1186/s12940-017-0272-y (2017).
Sarfo, J. O. et al. Acute lower respiratory infections among children under five in Sub-Saharan africa: a scoping review of prevalence and risk factors. BMC Pediatr. 23, 1. https://doi.org/10.1186/s12887-023-04033-x (2023).
Ahmed, K. Y. et al. Population modifiable risk factors associated with under-5 acute respiratory tract infections and diarrhoea in 25 countries in sub-Saharan Africa (2014–2021): an analysis of data from demographic and health surveys. eClinicalMedicine 68, 102444. https://doi.org/10.1016/j.eclinm.2024.102444 (2024).
Chilaka, C. A. & Mally, A. Mycotoxin occurrence, exposure and health implications in infants and young children in Sub-Saharan africa: a review. Foods 9, 1585. https://doi.org/10.3390/foods9111585 (2020).
Katoto, P. D. M. C. et al. Ambient air pollution and health in Sub-Saharan africa: current evidence, perspectives and a call to action. Environ. Res. 173, 174–188. https://doi.org/10.1016/j.envres.2019.03.029 (2019).
Das, I., Jagger, P. & Yeatts, K. Biomass cooking fuels and health outcomes for women in Malawi. EcoHealth 14, 7–19. https://doi.org/10.1007/s10393-016-1190-0 (2016).
Acknowledgements
The authors thank Measure DHS for granting access to the data.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
J.K.D., D.D., J.M.K.A., and J.N.F., developed the study concepts. J.K.D., analyzed the data. J.K.D wrote the original draft of the manuscript. D.D, and J.N.F supervised, reviewed, and revised the manuscript. All authors critically read, reviewed, and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Joseph, D.K., Dwomoh, D., Aheto, J.M.K. et al. Impact of household air pollution on under 5 mortalities and ARI in sub saharan africa: evidence from demographic and health survey 2010–2020. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38186-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38186-3