Abstract
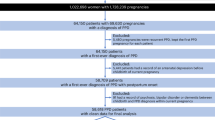
Postpartum depression (PPD) is a common mental health issue that negatively impacts maternal well-being and infant development. The COVID-19 pandemic has exacerbated depression risk among postpartum women due to added stressors from the crisis. This study aimed to assess PPD prevalence during the pandemic and identify associated factors. The study was conducted at Hanoi Obstetrics and Gynecology Hospital from May 2023 to December 2023. This cross-sectional study selected 223 postpartum women via convenience sampling. Data collection utilized online surveys and phone interviews. The Edinburgh Postnatal Depression Scale (EPDS) gauged depression levels, analyzed using Stata 16.0. Descriptive statistics and logistic regression explored relationships between PPD and contributing factors. Among participants, 22.0% scored 9–11 on EPDS, indicating mild depression; 5.8% were high-risk (EPDS 12–13), and 8.5% had PPD (EPDS > 14). The study identified links between PPD and poor sleep, COVID-19 anxiety, and limited social support. PPD remains a critical concern during COVID-19, with factors like sleep quality, pandemic-related anxiety, and social support influencing depression risk. Early screening and psychological interventions are crucial to mitigate PPD’s impact on maternal and infant health post-pandemic.
Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Klainin, P. & Arthur, D. G. Postpartum depression in Asian cultures: a literature review. Int. J. Nurs. Stud. 46, 1355–1373 (2009).
Ko, J. Y., Rockhill, K. M., Tong, V. T., Morrow, B. & Farr, S. L. Trends in postpartum depressive symptoms—27 states, 2004, 2008, and 2012. Morb. Mortal. Wkly Rep. 66, 153 (2017).
Bonari, L. et al. Perinatal risks of untreated depression during pregnancy. Can. J. Psychiatry. 49, 726–735. https://doi.org/10.1177/070674370404901103 (2004).
Goodman, S. H. & Gotlib, I. H. Risk for psychopathology in the children of depressed mothers: a developmental model for Understanding mechanisms of transmission. Psychol. Rev. 106, 458–490. https://doi.org/10.1037/0033-295x.106.3.458 (1999).
Murray, L. The impact of postnatal depression on infant development. J. Child. Psychol. Psychiatry. 33, 543–561. https://doi.org/10.1111/j.1469-7610.1992.tb00890.x (1992).
Liu, Y. et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol. Med. 47, 680–689. https://doi.org/10.1017/s003329171600283x (2017).
Puyané, M. et al. Personality traits as a risk factor for postpartum depression: A systematic review and meta-analysis. J. Affect. Disord. 298, 577–589. https://doi.org/10.1016/j.jad.2021.11.010 (2022).
Zanardo, V. et al. Psychological impact of COVID-19 quarantine measures in Northeastern Italy on mothers in the immediate postpartum period. Int. J. Gynecol. Obstet. Gynecol. 150, 184–188 (2020).
Fallon, V. et al. Psychosocial experiences of postnatal women during the COVID-19 pandemic. A UK-wide study of prevalence rates and risk factors for clinically relevant depression and anxiety. J. Psychiatr. Res. 136, 157–166 (2021).
Bajaj, M. A., Salimgaraev, R., Zhaunova, L. & Payne, J. L. Rates of self-reported postpartum depressive symptoms in the united States before and after the start of the COVID-19 pandemic. J. Psychiatr. Res. 151, 108–112. https://doi.org/10.1016/j.jpsychires.2022.04.011 (2022).
Brown, A. & Shenker, N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Maternal child. Nutr. 17, e13088 (2021).
Thapa, S. B., Mainali, A., Schwank, S. E. & Acharya, G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet. Gynecol. Scand. 99, 817–818 (2020).
Osborne, L. M., Kimmel, M. C. & Surkan, P. J. The crisis of perinatal mental health in the age of Covid-19. Maternal child. Health J. 25, 349–352 (2021).
Liu, C. H., Erdei, C. & Mittal, L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 pandemic. Psychiatry Res. 295, 113552. https://doi.org/10.1016/j.psychres.2020.113552 (2021).
Nguyen, H. T. T., Hoang, A. P., Do, L. T. K., Schiffer, S. & Nguyen, H. T. H. The rate and risk factors of postpartum depression in Vietnam from 2010 to 2020: A literature review. Front. Psychol. 12, 731306–731306. https://doi.org/10.3389/fpsyg.2021.731306 (2021).
Murray, L. et al. Postnatal depressive symptoms amongst women in central vietnam: a cross-sectional study investigating prevalence and associations with social, cultural and infant factors. BMC Pregnancy Childbirth. 15, 1–12 (2015).
Murray, L. et al. Postnatal depressive symptoms amongst women in central vietnam: a cross-sectional study investigating prevalence and associations with social, cultural and infant factors. BMC Pregnancy Childbirth. 15, 234. https://doi.org/10.1186/s12884-015-0662-5 (2015).
Bùi Văn Nhiều, N. T. H. U. Thực trạng rối loạn trầm cảm và nhu cầu hỗ trợ xã hội của bà mẹ có con dưới 6 tháng tuổi tại Thành phố Đà Nẵng. Tạp chí Khoa học và Công nghệ - Đại học Đà Nẵng 20(2), 2022 (2021).
Citu, C. et al. Prevalence and risk factors of postpartum depression in Romanian women during two periods of COVID-19 pandemic. J. Clin. Med. 11, 1628 (2022).
Zhao, X. H. & Zhang, Z. H. Risk factors for postpartum depression: an evidence-based systematic review of systematic reviews and meta-analyses. Asian J. Psychiatry. 53, 102353 (2020).
Lustberg, L. & Reynolds, C. F. III Depression and insomnia: questions of cause and effect. Sleep Med. Rev. 4, 253–262 (2000).
Iranpour, S., Kheirabadi, G. R., Esmaillzadeh, A., Heidari-Beni, M. & Maracy, M. R. Association between sleep quality and postpartum depression. J. Res. Med. Sci. Official J. Isfahan Univ. Med. Sci. https://doi.org/10.4103/1735-1995.193500 (2016).
Bàng Thị Hoài và cộng sự. Sàng lọc trầm cảm sau sinh và một số yếu tố liên quan tại phường Ô Chợ Dừa quận Đống Đa, Hà Nội, năm 2016. Tạp chí Y tế Công cộng Số 45 tháng 6/ (2018). (2018).
Acknowledgements
The authors would like to thank the Hanoi Obstetrics and Gynecology Hospital, the National University of Singapore, and the research collaborator.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: HTTN, HTN and GTTD. Data Curation: GTTD, TTN, CTN and PA. Formal Analysis: HTN and THTP. Funding Acquisition: LB, GTV and RCMH. Methodology & Software: TTN, MR, HD and CSHH. Supervision: HTTN, LB and RCMH. Validation: LAD, HNV and CTN. Writing – Original: HTTN, HTN and THTP. Writing – Review & Editing: HTTN, LB, PA, HD, GTV, RCMH and CSHH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. Approval was granted by the Scientific and Ethical Committee of Hanoi Obstetrics and Gynecology Hospital (No 1296/QĐ-PS). All participants provided their informed consent. All data has been anonymized to maintain confidentiality.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nguyen, H.T.T., Nguyen, H.T., Phan, T.H.T. et al. Prevalence and correlates of postpartum depression during the COVID-19 pandemic: a cross-sectional study in Vietnam. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38669-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38669-3