Abstract
The escalating effects of climate change, particularly global warming, are posing an increasing burden on human health. Older adults are particularly susceptible to the impact of extreme heat. Adequate water intake is essential to prevent dehydration in hot environments. Therefore, it is important to understand water turnover (WT) and intake. WT of older adults in hot environments remains unknown. This study aimed at investigating the seasonal effects on WT, total energy expenditure (TEE), and physical activity using doubly labeled water (DLW) and a triaxial accelerometer. A total of 26 older Japanese adult males and females aged ≥ 65 years participated in the study. WT and TEE were measured using DLW in May and August 2012. The mean values of maximum, mean, and minimum temperatures and mean humidity of the measurement days were 24 °C, 19 °C, 14 °C, and 57% in May (spring) and 35 °C, 29 °C, 25 °C, and 66% in August (summer) 2012, respectively. The mean (standard deviation, SD) age of the participants was 73.7 (5.4) years. Total body water increased significantly from 31.1 (4.6) to 31.9 (5.2) kg (+ 0.8 kg, P = 0.009) from May to August. TEE decreased significantly from 2271 (280) to 2123 (470) kcal/day (- 149 kcal/d, P = 0.036), while WT increased significantly from 2.939 (0.625) to 3.579 (0.943) L/day (+ 0.640 L/d, P < 0.001). WT increased by 640 mL/day during summer compared to that during spring, when the average temperature was 19 °C. Our findings indicate that WT increases during hot weather in older adults, reflecting seasonal adaptation.
Similar content being viewed by others
Data availability
The original contributions of this study are included in this article. Further inquiries can be directed to the corresponding author, Yosuke Yamada.
References
Romanello, M. et al. The 2023 report of the Lancet Countdown on health and climate change: The imperative for a health-centred response in a world facing irreversible harms. Lancet 402, 2346–2394. https://doi.org/10.1016/s0140-6736(23)01859-7 (2023).
Cai, W. et al. Views on climate change and health. Nat. Clim. Chang. 14, 419–423. https://doi.org/10.1038/s41558-024-01998-0 (2024).
Xi, D. et al. Risk factors associated with heatwave mortality in Chinese adults over 65 years. Nat. Med. 30, 1489–1498. https://doi.org/10.1038/s41591-024-02880-4 (2024).
Jacobsen, A. P. et al. Climate change and the prevention of cardiovascular disease. Am. J. Prev. Cardiol. 12, 100391. https://doi.org/10.1016/j.ajpc.2022.100391 (2022).
Ebi, K. L. et al. Hot weather and heat extremes: Health risks. Lancet 398, 698–708. https://doi.org/10.1016/s0140-6736(21)01208-3 (2021).
Vicedo-Cabrera, A. M. et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Chang. 11, 492–500. https://doi.org/10.1038/s41558-021-01058-x (2021).
Meade, R. D. et al. Physiological factors characterizing heat-vulnerable older adults: A narrative review. Environ. Int. 144, 105909. https://doi.org/10.1016/j.envint.2020.105909 (2020).
Hajat, S., Kovats, R. S. & Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk?. Occup. Environ. Med. 64, 93–100. https://doi.org/10.1136/oem.2006.029017 (2007).
Zanobetti, A., O’Neill, M. S., Gronlund, C. J. & Schwartz, J. D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. U. S. A. 109, 6608–6613. https://doi.org/10.1073/pnas.1113070109 (2012).
Balmain, B. N., Sabapathy, S., Louis, M. & Morris, N. R. Aging and thermoregulatory control: The clinical implications of exercising under heat stress in older individuals. Biomed. Res. Int. 2018, 8306154. https://doi.org/10.1155/2018/8306154 (2018).
Kenney, W. L. & Munce, T. A. Invited review: Aging and human temperature regulation. J. Appl. Physiol. 1985(95), 2598–2603. https://doi.org/10.1152/japplphysiol.00202.2003 (2003).
Bobb, J. F., Obermeyer, Z., Wang, Y. & Dominici, F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA 312, 2659–2667. https://doi.org/10.1001/jama.2014.15715 (2014).
Kephart, J. L. et al. City-level impact of extreme temperatures and mortality in Latin America. Nat. Med. 28, 1700–1705. https://doi.org/10.1038/s41591-022-01872-6 (2022).
Ballester, J. et al. Author Correction: Heat-related mortality in Europe during the summer of 2022. Nat. Med. 30, 603. https://doi.org/10.1038/s41591-023-02649-1 (2024).
Hooper, L., Bunn, D., Jimoh, F. O. & Fairweather-Tait, S. J. Water-loss dehydration and aging. Mech. Ageing Dev. 136–137, 50–58. https://doi.org/10.1016/j.mad.2013.11.009 (2014).
El-Sharkawy, A. M., Sahota, O., Maughan, R. J. & Lobo, D. N. The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clin. Nutr. 33, 6–13. https://doi.org/10.1016/j.clnu.2013.11.010 (2014).
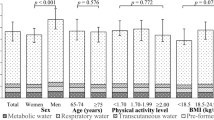
Yamada, Y. et al. Variation in human water turnover associated with environmental and lifestyle factors. Science 378, 909–915. https://doi.org/10.1126/science.abm8668 (2022).
Jéquier, E. & Constant, F. Water as an essential nutrient: The physiological basis of hydration. Eur. J. Clin. Nutr. 64, 115–123. https://doi.org/10.1038/ejcn.2009.111 (2010).
Yamada, Y. et al. Extracellular water may mask actual muscle atrophy during aging. J. Gerontol. A Biol. Sci. Med. Sci. 65, 510–516. https://doi.org/10.1093/gerona/glq001 (2010).
Phillips, P. A. et al. Reduced thirst after water deprivation in healthy elderly men. N. Engl. J. Med. 311, 753–759. https://doi.org/10.1056/nejm198409203111202 (1984).
Rowe, J. W., Shock, N. W. & DeFronzo, R. A. The influence of age on the renal response to water deprivation in man. Nephron 17, 270–278. https://doi.org/10.1159/000180731 (1976).
Davies, D. F. & Shock, N. W. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J. Clin. Invest. 29, 496–507. https://doi.org/10.1172/jci102286 (1950).
Denic, A., Glassock, R. J. & Rule, A. D. Structural and functional changes with the aging kidney. Adv. Chronic Kidney Dis. 23, 19–28. https://doi.org/10.1053/j.ackd.2015.08.004 (2016).
McDermott, B. P. et al. National athletic trainers’ association position statement: Fluid replacement for the physically active. J. Athl. Train 52, 877–895. https://doi.org/10.4085/1062-6050-52.9.02 (2017).
Hajat, S., O’Connor, M. & Kosatsky, T. Health effects of hot weather: From awareness of risk factors to effective health protection. Lancet 375, 856–863. https://doi.org/10.1016/s0140-6736(09)61711-6 (2010).
Li, S., Xiao, X. & Zhang, X. Hydration status in older adults: Current knowledge and future challenges. Nutrients https://doi.org/10.3390/nu15112609 (2023).
Liska, D. et al. Narrative review of hydration and selected health outcomes in the general population. Nutrients https://doi.org/10.3390/nu11010070 (2019).
Kim, H. K. et al. Predictors of water turnover in older adults: A doubly labeled water- and triaxial accelerometer-based study. J. Nutr. https://doi.org/10.1016/j.tjnut.2024.04.023 (2024).
Tanaka, N. et al. Relationship between seasonal changes in food intake and energy metabolism, physical activity, and body composition in young Japanese women. Nutrients https://doi.org/10.3390/nu14030506 (2022).
Garriga, A., Sempere-Rubio, N., Molina-Prados, M. J. & Faubel, R. Impact of seasonality on physical activity: A systematic review. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19010002 (2021).
Stelmach-Mardas, M. et al. Seasonality of food groups and total energy intake: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 70, 700–708. https://doi.org/10.1038/ejcn.2015.224 (2016).
Japan Meteorological Agency (2025). https://www.data.jma.go.jp/stats/etrn/view/monthly_s1.php?prec_no=61&block_no=47759&year=2012&month=5&day=&view=p1 (Accessed 20 April 2025)
Tani, Y. et al. The influence of season and air temperature on water intake by food groups in a sample of free-living Japanese adults. Eur. J. Clin. Nutr. 69, 907–913. https://doi.org/10.1038/ejcn.2014.290 (2015).
Westerterp, K. R., Plasqui, G. & Goris, A. H. Water loss as a function of energy intake, physical activity and season. Br. J. Nutr. 93, 199–203. https://doi.org/10.1079/bjn20041310 (2005).
Plasqui, G. & Westerterp, K. R. Seasonal variation in total energy expenditure and physical activity in Dutch young adults. Obes. Res. 12, 688–694. https://doi.org/10.1038/oby.2004.80 (2004).
Sohn, W., Heller, K. E. & Burt, B. A. Fluid consumption related to climate among children in the United States. J. Public Health Dent. 61, 99–106. https://doi.org/10.1111/j.1752-7325.2001.tb03373.x (2001).
Swanson, Z. S. & Pontzer, H. Water turnover among human populations: Effects of environment and lifestyle. Am. J. Hum. Biol. 32, e23365. https://doi.org/10.1002/ajhb.23365 (2020).
Zhang, X. et al. Human total, basal and activity energy expenditures are independent of ambient environmental temperature. iScience 25, 104682. https://doi.org/10.1016/j.isci.2022.104682 (2022).
Nissensohn, M., Castro-Quezada, I. & Serra-Majem, L. Beverage and water intake of healthy adults in some European countries. Int. J. Food Sci. Nutr. 64, 801–805. https://doi.org/10.3109/09637486.2013.801406 (2013).
Popkin, B. M., D’Anci, K. E. & Rosenberg, I. H. Water, hydration, and health. Nutr. Rev. 68, 439–458. https://doi.org/10.1111/j.1753-4887.2010.00304.x (2010).
Sawka, M. N., Cheuvront, S. N. & Carter, R. 3rd. Human water needs. Nutr. Rev. 63, S30–S39. https://doi.org/10.1111/j.1753-4887.2005.tb00152.x (2005).
Peel, M. C., Finlayson, B. L. & McMahon, T. A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 11, 1633–1644. https://doi.org/10.5194/hess-11-1633-2007 (2007).
Organization World Health Organization. Heat and Health, (2018). https://www.who.int/news-room/fact-sheets/detail/climate-change-heat-and-health (Accessed 11 June 2024)
Taylor, J. A. et al. Multisystem physiological perspective of human frailty and its modulation by physical activity. Physiol. Rev. 103, 1137–1191. https://doi.org/10.1152/physrev.00037.2021 (2023).
Ricci, N. A. & Cunha, A. I. L. Physical exercise for frailty and cardiovascular diseases. Adv. Exp. Med. Biol. 1216, 115–129. https://doi.org/10.1007/978-3-030-33330-0_12 (2020).
Deshayes, T. A. & Périard, J. D. Regular physical activity across the lifespan to build resilience against rising global temperatures. EBioMedicine 96, 104793. https://doi.org/10.1016/j.ebiom.2023.104793 (2023).
Wootton, E., Grossmann, M. & Warren, A. M. Dysnatremia in a changing climate: A global systematic review of the association between serum sodium and ambient temperature. Clin. Endocrinol. (Oxf.) 100, 527–541. https://doi.org/10.1111/cen.15052 (2024).
Baker, L. B., Munce, T. A. & Kenney, W. L. Sex differences in voluntary fluid intake by older adults during exercise. Med. Sci. Sports Exerc. 37, 789–796. https://doi.org/10.1249/01.mss.0000162622.78487.9c (2005).
Prpic, M., Hoffmann, C., Bauer, W., Hoffmann, P. & Kappert, K. Urban heat and burden of hyponatremia. JAMA Netw. Open 7, e2450280. https://doi.org/10.1001/jamanetworkopen.2024.50280 (2024).
Fujihira, K., Takahashi, M., Wang, C. & Hayashi, N. Factors explaining seasonal variation in energy intake: A review. Front. Nutr. 10, 1192223. https://doi.org/10.3389/fnut.2023.1192223 (2023).
Charlot, K., Faure, C. & Antoine-Jonville, S. Influence of hot and cold environments on the regulation of energy balance following a single exercise session: A mini-review. Nutrients https://doi.org/10.3390/nu9060592 (2017).
Millet, J. et al. Effects of acute heat and cold exposures at rest or during exercise on subsequent energy intake: A systematic review and meta-analysis. Nutrients https://doi.org/10.3390/nu13103424 (2021).
Sato, M. et al. Effects of aging on thermoregulatory responses and hormonal changes in humans during the four seasons in Japan. Int. J. Biometeorol. 55, 229–234. https://doi.org/10.1007/s00484-010-0328-y (2011).
Ji, K., Kim, Y. & Choi, K. Water intake rate among the general Korean population. Sci. Total Environ. 408, 734–739. https://doi.org/10.1016/j.scitotenv.2009.10.076 (2010).
Ng, S. W., Ni Mhurchu, C., Jebb, S. A. & Popkin, B. M. Patterns and trends of beverage consumption among children and adults in Great Britain, 1986–2009. Br. J. Nutr. 108, 536–551 (2012).
Kant, A. K., Graubard, B. I. & Atchison, E. A. Intakes of plain water, moisture in foods and beverages, and total water in the adult US population–nutritional, meal pattern, and body weight correlates: National Health and Nutrition Examination Surveys 1999–2006. Am. J. Clin. Nutr. 90, 655–663. https://doi.org/10.3945/ajcn.2009.27749 (2009).
Manz, F., Johner, S. A., Wentz, A., Boeing, H. & Remer, T. Water balance throughout the adult life span in a German population. Br. J. Nutr. 107, 1673–1681. https://doi.org/10.1017/s0007114511004776 (2012).
Albrecht, B. M., Stalling, I., Recke, C., Doerwald, F. & Bammann, K. Associations between older adults’ physical fitness level and their engagement in different types of physical activity: Cross-sectional results from the OUTDOOR ACTIVE study. BMJ Open 13, e068105. https://doi.org/10.1136/bmjopen-2022-068105 (2023).
Japan Meteorological Agency (2024). https://www.jma.go.jp/jma/index.html (Accessed 11 June 2024)
Yamada, Y. et al. Validity of a triaxial accelerometer and simplified physical activity record in older adults aged 64–96 years: A doubly labeled water study. Eur. J. Appl. Physiol. 118, 2133–2146. https://doi.org/10.1007/s00421-018-3944-6 (2018).
Yamada, Y. et al. Erratum to: Calculation of total energy expenditure in publications on physical activity energy by Yamada et al. in 2009 and 2013. Eur. J. Appl. Physiol. 116, 1279–1280. https://doi.org/10.1007/s00421-016-3376-0 (2016).
Weir, J. B. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 109, 1–9. https://doi.org/10.1113/jphysiol.1949.sp004363 (1949).
Ministry of Health Labour and Welfare Japan. Recommended Dietary Allowances for the Japanese 5th edn. (1995).
Raman, A. et al. Water turnover in 458 American adults 40–79 yr of age. Am. J. Physiol. Renal Physiol. 286, F394-401. https://doi.org/10.1152/ajprenal.00295.2003 (2004).
Du Bois, D. & Du Bois, E. F. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 5, 303–311 (1989).
Ministry of Education, C., Sprots, Science and Technology. Standard Tables of Food Composition in Japan. 7th revised. ed. (2015).
Acknowledgements
The authors would like to express our gratitude to all individuals who participated in the Kyoto–Kameoka Study as examiners for their valuable contributions to this work. We also acknowledge the administrative staff of Kameoka City and Kyoto Prefecture for their support. Finally, we express our sincere gratitude to all participants for their cooperation in this study. We would like to thank all investigators and volunteers who participated in this study, as well as Editage (www.Editage.jp) for English language editing.
Funding
This work was supported by the Japan Society for the Promotion of Science (KAKENHI grant numbers 24240091 to K.M. and 15H05363, 24H00683 to Y.Y.) and Suntory Holdings Limited, Osaka, Japan. The funding source had no role in the study design, data collection, analysis, interpretation, article writing, or decision to submit the article for publication.
Author information
Authors and Affiliations
Consortia
Contributions
The authors’ responsibilities are as follows: Y.Y., H.-K.K., and M.K.: conceptualization; Y.Y., T.Y., E.Y., H.N., and H.-K.K.: data curation; H.-K.K., A.I., and Y.Y.: formal analysis; Y.Y., T.Y., Yui.N., K.Y., H.S., and M.K.: investigation; Y.Y., H.-K.K., T.Y., Y.W., R.O., and M.K.: methodology; Y.Y. and M.K.: project administration; Y.Y., R.T., Y.N., N.T., and M.K.: resources; Y.Y. and M.K.: supervision; H.-K.K.: visualization; H.-K.K. Yui.N., and Y.Y.: writing—original All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
R.T., Y.N., and N.T. are employees of Suntory Holdings Limited. Y.Y. received a research grant from Suntory Holdings Ltd. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, HK., Nakayama, Y., Yoshida, T. et al. Hydration, water requirements, and energy balance from spring to summer in free-living older adults: a doubly labelled water study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38832-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38832-w