Abstract
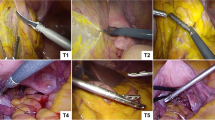
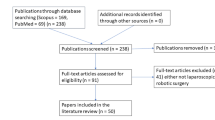
Laparoscopic suturing remains one of the most technically demanding skills in minimally invasive surgery. This study aimed to identify the key technical and cognitive challenges encountered during laparoscopic suturing through both subjective perceptions and objective performance analysis. It was also sought to inform the development of more effective, targeted training strategies to enhance laparoscopic suturing training proficiency. A cross-sectional study was conducted with 33 laparoscopic surgeons, 22 novices and 11 experts. A Delphi consensus among six expert surgeons identified four core subtasks which formed the basis of a structured survey. Participants performed standardized laparoscopic suturing on animal tissue using a box trainer before completing the questionnaire. Objective assessments using the Global Operative Assessment of Laparoscopic Skills (GOALS) evaluated time to completion, needle handling, knot tying quality, tissue manipulation, and tension maintenance through video analysis. Knot tying was reported as the most challenging task by 42.4% of participants, followed by needle handling at 27.3% and maintaining suture tension at 21.2%. No significant difference in perceived difficulty was observed between novice and expert surgeons. Objective GOALS-based analysis demonstrated that expert surgeons significantly outperformed novices across all metrics. Mean time to complete suturing was 5.7 ± 0.8 min for experts compared with 8.4 ± 1.2 min for novices (P < 0.001). Needle handling scores were 4.5 ± 0.3 versus 2.9 ± 0.5 (P < 0.001). Knot tying quality was 4.6 ± 0.4 versus 2.8 ± 0.6 (P < 0.001). Tissue manipulation scores were 4.4 ± 0.3 versus 3.0 ± 0.5 (P < 0.001). Tension maintenance scores were 4.5 ± 0.4 versus 2.7 ± 0.6 (P < 0.001). This study demonstrates that technical challenges in laparoscopic suturing persist across all experience levels. Integrating subjective perceptions with objective GOALS-based video analysis provides a comprehensive assessment of performance differences. Targeted simulation training focusing on knot tying, needle manipulation, hand positioning, and motion efficiency is essential to enhance suturing proficiency.
Similar content being viewed by others
Data availability
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author(s).
References
Gon, H. et al. Advantages of the laparoscopic approach for the initial operation in patients who underwent repeat hepatectomy. J. Gastrointest. Surg. 27(8), 1621–1631 (2023).
Kiblawi, R. et al. Laparoscopic versus open pediatric surgery: Three decades of comparative studies. Eur. J. Pediatr. Surg. 32(01), 9–25 (2022).
Chen, S. et al. Comparison of outcome and cost among open, laparoscopic, and robotic surgical treatments for rectal cancer: A propensity score matched analysis of nationwide inpatient sample data. J. Surg. Oncol. 117(3), 497–505 (2018).
Reznick, R. K. & MacRae, H. Teaching surgical skills—changes in the wind. N. Engl. J. Med. 355(25), 2664–2669 (2006).
Qadrie, Z., Maqbool, M., Dar, M. A. & Qadir, A. Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery. Open. Health 6(1), 20250059 (2025).
Gallagher, A. G., Al-Akash, M., Seymour, N. E. & Satava, R. M. An ergonomic analysis of the effects of camera rotation on laparoscopic performance. Surg. Endosc. 23(12), 2684–2691 (2009).
Bansal, V. K. et al. Laparoscopic suturing skills acquisition: A comparison between laparoscopy-exposed and laparoscopy-naive surgeons. JSLS 16(4), 623 (2012).
Hanna, G. B., Shimi, S. M. & Cuschieri, A. Task performance in endoscopic surgery is influenced by location of the image display. Ann. Surg. 227(4), 481–484 (1998).
Vuagniaux, A., Barberá-Carbonell, B., Dayer, A., Mantziari, S. & Suter, M. Meticulous closure of mesenteric defects effectively reduces the incidence of internal hernia after laparoscopic Roux-en-Y gastric bypass. Obes. Surg. 34(8), 2806–2813 (2024).
Stefanidis, D. et al. Skill retention following proficiency-based laparoscopic simulator training. Surgery 138(2), 165–170 (2005).
S. NE, Virtual reality training improves operating room performance results of a randomized, double-blinded study. Ann. Surg. 236(4), 458–464 (2002).
Sarker, S. K. & Vincent, C. Errors in surgery. Int. J. Surg. 3(1), 75–81 (2005).
Reiley, C. E., Lin, H. C., Yuh, D. D. & Hager, G. D. Review of methods for objective surgical skill evaluation. Surg. Endosc. 25(2), 356–366 (2011).
Croce, E. & Olmi, S. Intracorporeal knot-tying and suturing techniques in laparoscopic surgery: Technical details. JSLS 4(1), 17 (2000).
Cardoso, S. A. et al. Exploring the role of simulation training in improving surgical skills among residents: A narrative review. Cureus 15(9) (2023).
Darzi, A. & Munz, Y. The impact of minimally invasive surgical techniques. Annu. Rev. Med. 55(1), 223–237 (2004).
Akritidou, E. et al. Virtual reality simulation training in laparoscopic suturing and knot-tying: A narrative review. Ann Laparosc. Endosc Surg (2024).
Lim, S., Ghosh, S., Niklewski, P. & Roy, S. Laparoscopic suturing as a barrier to broader adoption of laparoscopic surgery. JSLS 21(3), e2017-00021 (2017).
Dehabadi, M., Fernando, B. & Berlingieri, P. The use of simulation in the acquisition of laparoscopic suturing skills. Int. J. Surg. 12(4), 258–268 (2014).
Vassiliou, M. C. et al. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am. J. Surg. 190(1), 107–113 (2005).
Haber, J. J. & Helou, E. A comparative study of laparoscopic skills between novices and experts: How to steepen the learning curve. Cureus 16, 12 (2024).
Tang, B., Zhang, L. & Alijani, A. Evidence to support the early introduction of laparoscopic suturing skills into the surgical training curriculum. BMC Med. Educ. 20, 1–11 (2020).
Lin, W. et al. Study on the application of progressive training method combined with imagery training method in laparoscopic suturing skills training for resident physicians. BMC Med. Educ. 25(1), 369 (2025).
van Zwieten, T. et al. Assessment methods in laparoscopic colorectal surgery: A systematic review of available instruments. Int. J. Colorectal Dis. 38(1), 105 (2023).
Humm, G., Harries, R. L., Stoyanov, D. & Lovat, L. B. Supporting laparoscopic general surgery training with digital technology: The United Kingdom and Ireland paradigm. BMC Surg. 21(1), 123 (2021).
Bonrath, E. M. et al. Laparoscopic simulation training: Testing for skill acquisition and retention. Surgery 152(1), 12–20 (2012).
Charokar, K. & Modi, J. N. Simulation-based structured training for developing laparoscopy skills in general surgery and obstetrics & gynecology postgraduates. J. Educ. Health Promot. 10(1), 387 (2021).
Mukhtar, F., Shaheen, M. F., Alhabeeb, A. Y., Zafar, M. & Alkattan, K. Impact of Simulation-Based surgical training in laparoscopy on satisfaction level and proficiency in surgical skills. Adv. Med. Educ. Pract. 357–366 (2025).
Liang, Y. et al. Construction and implementation of a laparoscopic skill training course based on a smartphone application and virtual reality. BMC Med. Educ. 24(1), 1111 (2024).
Skjold-Odegaard, B. et al. Development and clinical implementation of a structured, simulation-based training programme in laparoscopic appendectomy: Description, validation and evaluation. BMJ Simul. Technol. Enhanc Learn. 7(6), 517 (2021).
Widder, A. et al. Optimizing laparoscopic training efficacy by ‘deconstruction into key steps’: A randomized controlled trial with novice medical students. Surg. Endosc 36(12), 8726–8736 (2022).
Lovasik, B. P. et al. Development of a laparoscopic surgical skills simulation curriculum: Enhancing resident training through directed coaching and closed-loop feedback. Surgery 171(4), 897–903 (2022).
Xu, X. et al. Evaluation of a progressive laparoscopic training program for clinical professional master’s degree residents in China: Skill improvement and educational implications. BMC Med. Educ. 25(1), 1341 (2025).
Geissler, M. E. et al. Comparison of laparoscopic performance using low-cost laparoscopy simulators versus state-of-the-art simulators: A multi-center prospective, randomized crossover trial. Surg. Endosc. 39(3), 2016–2025 (2025).
Hamilton, A. The future of artificial intelligence in surgery. Cureus 16, 7 (2024).
Riddle, E. W., Kewalramani, D., Narayan, M. & Jones, D. B. Surgical simulation: Virtual reality to artificial intelligence. Curr. Probl. Surg. 61(11), 101625 (2024).
Cheng, K. et al. Artificial intelligence-based automated laparoscopic cholecystectomy surgical phase recognition and analysis. Surg. Endosc 36(5), 3160–3168 (2022).
Fernicola, A., Palomba, G., Capuano, M., De Palma, G. D. & Aprea, G. Artificial intelligence applied to laparoscopic cholecystectomy: What is the next step? A narrative review. Updates Surg. 76(5), 1655–1667 (2024).
Wu, S. et al. Impact of an AI-based laparoscopic cholecystectomy coaching program on the surgical performance: A randomized controlled trial. Int. J. Surg. 110(12), 7816–7823 (2024).
Chevalier, O., Dubey, G., Benkabbou, A., Majbar, M. A. & Souadka, A. Comprehensive overview of artificial intelligence in surgery: A systematic review and perspectives. Pflügers Arch. Eur. J. Physiol. 1–10 (2025).
Brian, R., Murillo, A., Gomes, C. & Alseidi, A. Artificial intelligence and robotic surgical education. Glob. Surg. Educ. J. Assoc. Surg. Educ. 3(1), 60 (2024).
Ma, R. et al. Artificial intelligence-based video feedback to improve novice performance on robotic suturing skills: A pilot study. J. Endourol. (2024).
Huang, X. et al. An intelligent Grasper to provide real-time force feedback to shorten the learning curve in laparoscopic training. BMC Med. Educ. 24(1), 161 (2024).
Luo, Y. et al. Enhancing laparoscopic surgery training: A comparative study of traditional models and automated error detection system. BMC Med. Educ. 25(1), 677 (2025).
Funding
This research has been funded by the Engineering and Physical Sciences Research Council (EPSRC) of the United Kingdom under Grant Reference EP/Y017307/1.
Author information
Authors and Affiliations
Contributions
Conceptualization, C.O. and B.T.; methodology, C.O., S.L., and B.T.; data curation, C.O and B.T.; writing—original draft preparation, C.O.; writing; review and editing, C.O. C.T., S.L., B.Z., P. S., M.E., and B, T. All authors have read and agreed to the current version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of University of Dundee (UOD-SMED-SLS-Staff-2024-24-117).
Informed consent
Verbal consent was obtained from the participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ogbonnaya, C., Li, S., Tang, C. et al. Integrating subjective perceptions and objective video analysis to identify challenges in laparoscopic suturing: a cross-sectional study to enhance surgical training. Sci Rep (2026). https://doi.org/10.1038/s41598-026-39914-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-39914-5