Abstract
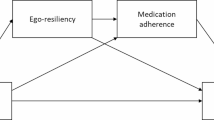
Social support is necessary for patients with heart failure (HF) to take medication, which can lead to decreased hospitalization and mortality rates. However, the effect of patient health literacy on this relationship remains unclear. This study aimed to evaluate the mediating effect of health literacy on the relationship between social support and medication adherence among patients with HF. A cross-sectional correlational design was used between August and October 2024 for 249 patients with HF. Data were collected using patients’ sociodemographic and health status, the Arabic version of the General Medication Adherence Scale (GMAS), BRIEF Health Literacy Screening Tool, and Oslo Social Support Scale (OSSS-3). Hayes’ Process Macro program, version 4.2, Model 4, was used to assess the possible interaction effects. Statistical significance was set at p less than .05. There was a weak positive correlation between patients’ medication adherence and health literacy (r = .247, p < .001) and social support (r = .204, p < .001). In addition, there was a significant correlation between HL status and social support (r = .314, p < .001). Factors that increased medication adherence included older age (B = 0.06, p = .027), not smoking (B = 2.21, p < .001), other chronic diseases (B = 1.23, p = .005), higher health literacy (B = 0.30, p = .002), and social support (B = 0.33, p = .044). The model indicated an indirect positive effect of social support on medication adherence through health literacy (β = 0.064, p = .007). Social support had a positive direct effect on health literacy (β = 0.314, p < .001) and a positive effect of health literacy on medication adherence (β = 0.203, p = .002). Social support had a significant positive direct effect on medication adherence (β = 0.140, p = .031), with a total effect of β = 0.204, p = .001. Health literacy showed a statistically significant indirect association in the mediation model. This study revealed that patients with higher health literacy are better equipped to manage complex treatment regimens and engage in self-care. This effect was further amplified by social support, which both directly and indirectly enhanced adherence.
Similar content being viewed by others
Data availability
The data are available at request from the corresponding author.
Abbreviations
- HF:
-
Heart failure
- GMAS:
-
General Medication Adherence Scale
- OSSS-3:
-
Oslo Social Support Scale
- IMBS:
-
Information-motivation-behavioral skills model
- CI:
-
Confidence interval
References
Ponikowski, P. et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37(27), 2129–2200 (2016).
Savarese, G. & Lund, L. H. Global public health burden of heart failure. Card. Fail. Rev. 3(1), 7–11 (2017).
GBD Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet (Lond. Engl.) 392(10159), 1789–1858 (2018).
Heidenreich, P. A. et al. Forecasting the impact of heart failure in the United States: A policy statement from the American Heart Association. Circ. Heart Fail. 6(3), 606–619 (2013).
Alshammari, B. et al. Exploring nurses’ knowledge of and attitudes towards the management of patients with heart failure in Saudi Arabia: A cross-sectional design. Healthcare (Basel) https://doi.org/10.3390/healthcare13050522 (2025).
Tash, A. A. & Al-Bawardy, R. F. Cardiovascular disease in Saudi Arabia: Facts and the way forward. J. Saudi Heart Assoc. 35(2), 148–162 (2023).
Shah, D., Simms, K., Barksdale, D. J. & Wu, J.-R. Improving medication adherence of patients with chronic heart failure: challenges and solutions. Res. Rep. Clin. Cardiol., pp. 87–95 (2015).
Jarrah, M. et al. Medication adherence and its influencing factors among patients with heart failure: A cross sectional study. Medicina (Kaunas) https://doi.org/10.3390/medicina59050960 (2023).
Jimmy, B. & Jose, J. Patient medication adherence: Measures in daily practice. Oman Med. J. 26(3), 155–159 (2011).
Ruppar, T. M., Cooper, P. S., Mehr, D. R., Delgado, J. M. & Dunbar-Jacob, J. M. Medication adherence interventions improve heart failure mortality and readmission rates: Systematic review and meta-analysis of controlled trials. J. Am. Heart Assoc. 5(6), e002606 (2016).
Hussein, D. et al. Medication adherence and associated factors among chronic heart failure patients on follow-up in North Shewa Public Hospitals, Oromia region, Ethiopia. BMC Cardiovasc. Disord. 24(1), 444 (2024).
Silavanich, V., Nathisuwan, S., Phrommintikul, A. & Permsuwan, U. Relationship of medication adherence and quality of life among heart failure patients. Heart Lung 48(2), 105–110 (2019).
Raffaa, H. S. M. et al. Adherence of heart failure patients to heart failure medications and its determinants in the Aseer region, Southern Saudi Arabia. J. Fam. Med. Prim. Care 9(9), 5041–5045 (2020).
Sayers, S. L., Riegel, B., Pawlowski, S., Coyne, J. C. & Samaha, F. F. Social support and self-care of patients with heart failure. Ann. Behav. Med. 35(1), 70–79 (2008).
Wu, J. R. et al. Medication adherence, social support, and event-free survival in patients with heart failure. Health Psychol. 32(6), 637–646 (2013).
Cheng, Y., Peng, Q., Ding, H., Hu, M. & Li, C. Pathway analysis of the impact of health literacy, social support, and self-management on frailty in patients with chronic heart failure: A cross-sectional study. Medicine (Baltimore) 103(43), e40195 (2024).
Institute of Medicine Committee on Health Literacy In Health Literacy: A Prescription to End Confusion (eds Nielsen-Bohlman, L. et al.) (National Academies Press, 2004).
Munson Klyn, N. A., Mohammed Shaikh, Z. & Dhar, S. Health literacy and self-reported hearing aid use in the health and retirement study. Ear Hear 41(2), 386–394 (2020).
Fisher, J. D. & Fisher, W. A. Changing AIDS-risk behavior. Psychol. Bull. 111(3), 455–474 (1992).
Pasay-an, E., Saguban, R., Cabansag, D. & Alkubati, S. Health literacy as mediator between perception of illness and self-medication behaviour among outpatients in the Kingdom of Saudi Arabia: Implication to primary healthcare nursing. BMC Nurs. 23(1), 278 (2024).
Ruppar, T. M., Delgado, J. M. & Temple, J. Medication adherence interventions for heart failure patients: A meta-analysis. Eur. J. Cardiovasc. Nurs. 14(5), 395–404 (2015).
Shahin, W., Kennedy, G. A. & Stupans, I. The association between social support and medication adherence in patients with hypertension: A systematic review. Pharm. Pract. 19(2), 2300 (2021).
Naqvi, A. A. et al. Development and validation of a novel general medication adherence scale (GMAS) for chronic illness patients in Pakistan. Front. Pharmacol. 9, 1124 (2018).
Naqvi, A. A. et al. Validation of the general medication adherence scale in Saudi patients with chronic diseases. Front. Pharmacol. 10, 633 (2019).
Naqvi, A. A., Hassali, M. A., Jahangir, A., Nadir, M. N. & Kachela, B. Translation and validation of the English version of the general medication adherence scale (GMAS) in patients with chronic illnesses. J. Drug Assess. 8(1), 36–42 (2019).
Haun, J., Luther, S., Dodd, V. & Donaldson, P. Measurement variation across health literacy assessments: Implications for assessment selection in research and practice. J. Health Commun. 17(Suppl 3), 141–159 (2012).
Alqarni, A. S. et al. Relationship between the health literacy and self-medication behavior of primary health care clientele in the Hail region, Saudi Arabia: Implications for public health. Eur. J. Investig. Health Psychol. Educ. 13(6), 1043–1057 (2023).
Kocalevent, R. D. et al. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 6(1), 31 (2018).
Alshammari, B. et al. The influence of social support on sleep and fatigue level among patients receiving hemodialysis in Saudi Arabia: A cross-sectional correlational design. Front. Psychol. 14, 1272500 (2023).
Alharbi, A., Alkubati, S. A., Alshahrani, Y., Pasay-an, E. & Alshara, A. Health-promoting behaviors and its relationship with anxiety, depression, and social support among nursing students in Saudi Arabia: A cross-sectional study. Public Health Nurs. 42(3), 1249–1260 (2025).
Oh, E. H., Kim, C. J. & Schlenk, E. A. A predictive model for medication adherence in older adults with heart failure. Eur. J. Cardiovasc. Nurs. 23(6), 635–643 (2024).
Rezaei, S., Vaezi, F., Afzal, G., Naderi, N. & Mehralian, G. Medication adherence and health literacy in patients with heart failure: A cross-sectional survey in Iran. Health Lit. Res. Pract. 6(3), e191–e199 (2022).
Garred, C. H. et al. Adherence and discontinuation of optimal heart failure therapies according to age: A Danish nationwide study. J. Am. Heart Assoc. 11(19), e026187 (2022).
Hou, Q., Zhao, Y. & Wu, Y. Medication adherence trajectories and clinical outcomes in patients with cardiovascular disease: A systematic review and meta-analysis. J. Glob. Health 15, 04145 (2025).
Garcia, R. A. et al. Association of medication adherence with health outcomes in the ISCHEMIA trial. J. Am. Coll. Cardiol. 80(8), 755–765 (2022).
Ding, N. et al. Cigarette smoking, cessation, and risk of heart failure with preserved and reduced ejection fraction. J. Am. Coll. Cardiol. 79(23), 2298–2305 (2022).
Almazan, J. U. et al. Sustainability in education and healthcare field: An integrative review of factors, barriers, and the path forward for informed practices. Health Prof. Educ. 10(4), 3 (2024).
Parmar, J., El Masri, A., MacMillan, F., McCaffery, K. & Arora, A. Health literacy and medication adherence in adults from ethnic minority backgrounds with type 2 diabetes mellitus: A systematic review. BMC Public Health 25(1), 222 (2025).
Alatawi, A. A., Alaamri, M. & Almutary, H. Social support and adherence to treatment regimens among patients undergoing hemodialysis. Healthcare 12(19), 1958 (2024).
Guo, A. et al. Impact of health literacy and social support on medication adherence in patients with hypertension: A cross-sectional community-based study. BMC Cardiovasc. Disord. 23(1), 93 (2023).
Teppo, K. et al. Association of income and educational levels with adherence to direct oral anticoagulant therapy in patients with incident atrial fibrillation: A Finnish nationwide cohort study. Pharmacol. Res. Perspect. 10(3), e00961 (2022).
Acknowledgements
We would like to thank all patients who participated in this study
Author information
Authors and Affiliations
Contributions
Sameer A. Alkubati: Conceptualization, data curation, formal analysis, investigation, methodology, resources, validation, visualization, writing—original draft, writing—review, and editing. Homoud Khaled Aleyadah; Data curation, investigation, methodology. Habib Alrasashedi: Writing-original draft, writing-review, and editing. Awatif M. Alrasheeday; Writing—original draft; writing—review and editing. Abdulhafith Alharbi: Writing—original draft; writing—review and editing. Bandar Alsaif, Writing—original draft; Writing—review and editing, Joseph U Almazan; Writing—original draft, writing—review, and editing. Aziza Z. Ali; Writing—original draft, writing—review and editing, Bushra Alshammari; Conceptualization, data curation, and investigation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Research Ethics Committee of Ha’ il’s Cluster of Health (2024/13) and the Research Ethics Committee of the University of Ha’il (H/2024/085). This study was conducted in accordance with the principles of the Declaration of Helsinki. Before starting the survey, all participants were requested to read the description on the first page of the online survey link. The purpose and extent of the study, their consent to participate, confidentiality, anonymity, the option to withdraw from research engagement, and the fact that no personal identifying information was collected were covered in this explanation. The purpose of the study was explained to the participants, who were assured that any data collected would only be used for research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alkubati, S.A., Aleyadah, H.K., Alrashedi, H. et al. The impact of social support on medication adherence among patients with heart failure: health literacy as a mediator. Sci Rep (2026). https://doi.org/10.1038/s41598-026-40360-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-40360-6