Abstract
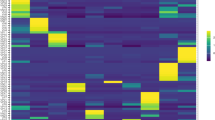
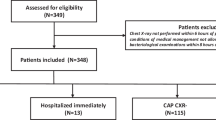
Streptococcus pneumoniae is the most common microbial cause of community-acquired pneumonia. Currently, there are no available models of severe pneumococcal pneumonia in mechanically ventilated animals to mimic clinical conditions of critically ill patients. We studied endogenous pulmonary flora in 4 healthy pigs and in an additional 10 pigs in which we intra-bronchially instilled S. pneumoniae serotype 19 A, characterized by its resistance to penicillin, macrolides and tetracyclines. The pigs underwent ventilation for 72 h. All pigs that were not challenged with S. pneumoniae completed the 72-h study, whereas 30% of infected pigs did not. At 24 h, we clinically confirmed pneumonia in the infected pigs; upon necropsy, we sampled lung tissue for microbiological/histological confirmation of pneumococcal pneumonia. In control pigs, Streptococcus suis and Staphylococcus aureus were the most commonly encountered pathogens, and their lung tissue mean ± s.e.m. concentration was 7.94 ± 20 c.f.u./g. In infected pigs, S. pneumoniae was found in the lungs of all pigs (mean ± s.e.m. pulmonary concentration of 1.26 × 105 ± 2 × 102 c.f.u./g). Bacteremia was found in 50% of infected pigs. Pneumococcal pneumonia was confirmed in all infected pigs at 24 h. Pneumonia was associated with thrombocytopenia, an increase in prothrombin time, cardiac output and vasopressor dependency index and a decrease in systemic vascular resistance. Upon necropsy, microbiological/histological pneumococcal pneumonia was confirmed in 8 of 10 pigs. We have therefore developed a novel model of penicillin- and macrolide-resistant pneumococcal pneumonia in mechanically ventilated pigs with bacteremia and severe hemodynamic compromise. The model could prove valuable for appraising the pathogenesis of pneumococcal pneumonia, the effects associated with macrolide resistance and the outcomes related to the use of new diagnostic strategies and antibiotic or complementary therapies.
This is a preview of subscription content, access via your institution
Access options






Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cilloniz, C. et al. Microbial aetiology of community-acquired pneumonia and its relation to severity. Thorax 66, 340–346 (2011).
Feikin, D. R. et al. Mortality from invasive pneumococcal pneumonia in the era of antibiotic resistance, 1995-1997. Am. J. Public Health 90, 223–229 (2000).
Bedos, J. P. et al. Host-pathogen interactions and prognosis of critically ill immunocompetent patients with pneumococcal pneumonia: the nationwide prospective observational STREPTOGENE study. Intensive Care Med. 44, 2162–2173 (2018).
Schroeder, M. R. & Stephens, D. S. Macrolide resistance in Streptococcus pneumoniae. Front. Cell. Infect. Microbiol. 6, 98 (2016).
Schroeder, M. R. et al. A population-based assessment of the impact of 7- and 13-valent pneumococcal conjugate vaccines on macrolide-resistant invasive pneumococcal disease: emergence and decline of Streptococcus pneumoniae serotype 19A (CC320) with dual macrolide resistance mechanisms. Clin. Infect. Dis. 65, 990–998 (2017).
Naucler, P. et al. Comparison of the impact of pneumococcal conjugate vaccine 10 or pneumococcal conjugate vaccine 13 on invasive pneumococcal disease in equivalent populations. Clin. Infect. Dis. 65, 1780–1789 (2017).
Aliberti, S., Mantero, M., Mirsaeidi, M. & Blasi, F. The role of vaccination in preventing pneumococcal disease in adults. Clin. Microbiol. Infect. 20, 52–58 (2014).
Fenoll, A. et al. Temporal trends of invasive Streptococcus pneumoniae serotypes and antimicrobial resistance patterns in Spain from 1979 to 2007. J. Clin. Microbiol. 47, 1012–1020 (2009).
Quah, J., Jiang, B., Tan, P. C., Siau, C. & Tan, T. Y. Impact of microbial Aetiology on mortality in severe community-acquired pneumonia. BMC Infect. Dis. 18, 451 (2018).
Chiavolini, D., Pozzi, G. & Ricci, S. Animal models of Streptococcus pneumoniae disease. Clin. Microbiol. Rev. 21, 666–685 (2008).
Luna, C. M. et al. Experimental severe Pseudomonas aeruginosa pneumonia and antibiotic therapy in piglets receiving mechanical ventilation. Chest 132, 523–531 (2007).
Martinez-Olondris, P. et al. An experimental model of pneumonia induced by methicillin-resistant Staphylococcus aureus in ventilated piglets. Eur. Respir. J. 36, 901–906 (2010).
Azoulay-Dupuis, E., Bedos, J. P., Vallee, E. & Pocidalo, J. J. Comparative activity of fluorinated quinolones in acute and subacute Streptococcus pneumoniae pneumonia models: efficacy of temafloxacin. J. Antimicrob. Chemother. 28, 45–53 (1991).
Iwasaki, K. et al. Combined effects of both bacteria and gastric juice on pneumonia in mice. Respir. Physiol. 116, 201–209 (1999).
Croisier, D. et al. Mutant selection window in levofloxacin and moxifloxacin treatments of experimental pneumococcal pneumonia in a rabbit model of human therapy. Antimicrob. Agents Chemother. 48, 1699–1707 (2004).
Piroth, L. et al. Development of a new experimental model of penicillin-resistant Streptococcus pneumoniae pneumonia and amoxicillin treatment by reproducing human pharmacokinetics. Antimicrob. Agents Chemother. 43, 2484–2492 (1999).
Kraft, B. D. et al. Development of a novel preclinical model of pneumococcal pneumonia in nonhuman primates. Am. J. Respir. Cell Mol. Biol. 50, 995–1004 (2014).
Reyes, L. F. et al. A non-human primate model of severe pneumococcal pneumonia. PLoS One 11, e0166092 (2016).
Lim, S. C. et al. Transient hemodynamic effects of recruitment maneuvers in three experimental models of acute lung injury. Crit. Care Med. 32, 2378–2384 (2004).
Walden, A. P. et al. Patients with community acquired pneumonia admitted to European intensive care units: an epidemiological survey of the GenOSept cohort. Crit. Care 18, R58 (2014).
Yang, M. et al. Corticosteroid therapy combined with antibiotics for severe Streptococcus pneumoniae pneumonia in ventilated piglets. Eur. Respir. J. 54, PA4553 (2019).
Torres, A. et al. Sampling methods for ventilator-associated pneumonia: validation using different histologic and microbiological references. Crit. Care Med. 28, 2799–2804 (2000).
Cilloniz, C. et al. Community-acquired polymicrobial pneumonia in the intensive care unit: aetiology and prognosis. Crit. Care 15, R209 (2011).
Nicholson, S. C. et al. A randomised, double-blind trial comparing ceftobiprole medocaril with ceftriaxone with or without linezolid for the treatment of patients with community-acquired pneumonia requiring hospitalisation. Int. J. Antimicrob. Agents 39, 240–246 (2012).
MacGowan, A. P., Noel, A. R., Tomaselli, S. & Bowker, K. E. Pharmacodynamics of ceftaroline against Staphylococcus aureus studied in an in vitro pharmacokinetic model of infection. Antimicrob. Agents Chemother. 57, 2451–2456 (2013).
Cilloniz, C. et al. The effect of macrolide resistance on the presentation and outcome of patients hospitalized for Streptococcus pneumoniae pneumonia. Am. J. Respir. Crit. Care Med. 191, 1265–1272 (2015).
Mandell, L. A. et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 44, S27–S72 (2007).
Zimmermann, P., Ziesenitz, V. C., Curtis, N. & Ritz, N. The immunomodulatory effects of macrolides—a systematic review of the underlying mechanisms. Front. Immunol. 9, 302 (2018).
Reyes, L. F. et al. Severe pneumococcal pneumonia causes acute cardiac toxicity and subsequent cardiac remodeling. Am. J. Respir. Crit. Care Med. 196, 609–620 (2017).
Roberts, J. A. & Roberts, D. M. Antibiotic dosing in critically ill patients with septic shock and on continuous renal replacement therapy: can we resolve this problem with pharmacokinetic studies and dosing guidelines? Crit. Care 18, 156 (2014).
So, W., Crandon, J. L. & Nicolau, D. P. Poor outcomes of empiric ceftriaxone +/- azithromycin for community-acquired pneumonia caused by methicillin-susceptible Staphylococcus aureus. Intern. Emerg. Med. 11, 545–551 (2016).
Owens, R. C. Jr. et al. Pharmacodynamics of ceftriaxone and cefixime against community-acquired respiratory tract pathogens. Int. J. Antimicrob. Agents 17, 483–489 (2001).
Li Bassi, G. et al. Effects of duty cycle and positive end-expiratory pressure on mucus clearance during mechanical ventilation*. Crit. Care Med. 40, 895–902 (2012).
D’Angelo, E. et al. Respiratory mechanics in anesthetized paralyzed humans: effects of flow, volume, and time. J. Appl. Physiol. (1985) 67, 2556–2564 (1989).
Cruz, D. N. et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA 301, 2445–2452 (2009).
Li Bassi, G. et al. Gravity predominates over ventilatory pattern in the prevention of ventilator-associated pneumonia. Crit. Care Med. 42, e620–e627 (2014).
Onyeji, C. O. et al. Comparative efficacies of levofloxacin and ciprofloxacin against Streptococcus pneumoniae in a mouse model of experimental septicaemia. Int. J. Antimicrob. Agents 12, 107–114 (1999).
Rennard, S. I. et al. Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J. Appl. Physiol. (1985) 60, 532–538 (1986).
Preston, S. L. et al. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA 279, 125–129 (1998).
Acknowledgements
We deeply thank Francesc Marco (Microbiology Department, Hospital Clinic) for his swift and valuable support in identifying and providing human S. pneumoniae strains upon study commencement. In addition, we acknowledge the healthcare providers from the pulmonary intensive care unit at Hospital Clinic, Barcelona for all their encouragement during these studies. Support was provided by the Instituto de Salud Carlos III de Madrid (Spain) (FIS PI15/00506), Fundació La Marató de TV3 (201831-10), the Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Centro de Investigación Biomedica En Red- Enfermedades Respiratorias (CIBERES) and BITRECS (IDIBAPS) 2019.
Author information
Authors and Affiliations
Contributions
R.A., G.L.B, A.M. and A.T. participated in the development of the protocol, study design, study management, statistical analysis and data interpretation and wrote the first draft of the report. L.F.B, E.A.X., M. Rigol, G.F., C.T., J.B., F.P., M.C., T.C., C.C., M.Y., H.Y., M.A., J.D.M., F.D.R., M.A.S., M. Rinaudo and S.T. participated in data collection and interpretation and critically reviewed the first draft of the report. M.J.S., D.P.N., A.A. and J.R. participated in study design and reviewed the report.
Corresponding author
Ethics declarations
Competing interests
A.T. has received grants from MedImmune, Cubist, Bayer, Theravance and Polyphor and personal fees as an advisory board member from Bayer, Roche, The Medicines CO and Curetis. He has received personal fees as a member of the speaker’s bureau from GSK, Pfizer, Astra Zeneca and Biotest Advisory Board, outside the submitted work. None of the other authors have any competing interests with the current publication.
Additional information
Peer review information Lab Animal thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Methods, Supplementary Figures 1–4, Supplementary Tables 1–2
Supplementary Data
ARRIVE checklist
Rights and permissions
About this article
Cite this article
Amaro, R., Li Bassi, G., Motos, A. et al. Development and characterization of a new swine model of invasive pneumococcal pneumonia. Lab Anim 50, 327–335 (2021). https://doi.org/10.1038/s41684-021-00876-y
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41684-021-00876-y
This article is cited by
-
Corticosteroid and antimicrobial therapy in macrolide-resistant pneumococcal pneumonia porcine model
Intensive Care Medicine Experimental (2025)
-
Estimation of normal lung weight index in healthy female domestic pigs
Intensive Care Medicine Experimental (2024)
-
An ovine septic shock model of live bacterial infusion
Intensive Care Medicine Experimental (2024)