Abstract
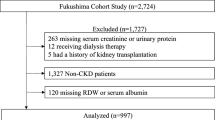
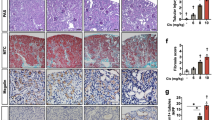
This Review evaluates various mouse and rat models of chronic kidney disease (CKD) that result from repeated low-dose cisplatin (RLDC) treatment while also discussing ethical considerations on the topic. Cisplatin can cause nephrotoxicity, and high doses of cisplatin can cause acute kidney injury. The RLDC regimen has been used in the treatment of solid organ cancers and has shown efficacy in reducing the occurrence of acute kidney injury in patients. However, prolonged treatments may lead to CKD. Mouse and rat models that effectively replicate the pathological features of CKD are invaluable for studying the mechanisms of the disease and exploring potential therapeutic interventions. Whereas administration of a single higher dose in some RLDC models may lead to higher mortality rates, a single lower dose may not replicate the fibrotic characteristics of CKD. Here we gathered information on mouse and rat models of RLDC-induced CKD and analyzed the impact of different variables, such as animal age, cisplatin dosage and administration frequency, on success rates, mortality rate and weight loss. Among the different models, weekly intraperitoneal administration of 8 mg/kg or 9 mg/kg of cisplatin for a total of 4 weeks in 12-week-old male C57BL/6 mice showed the most similar clinical characteristics of CKD while adhering to ethical requirements. In this Review, we suggest the best timings for both drug intervention and observation based on the biological traits of the model. Furthermore, given the limited research available on RLDC-induced CKD rat models, it is urgent to focus on developing RLDC methods that can induce detailed characteristics of CKD in rats.
This is a preview of subscription content, access via your institution
Access options
Similar content being viewed by others
References
Tang, C., Livingston, M. J., Safirstein, R. & Dong, Z. Cisplatin nephrotoxicity: new insights and therapeutic implications. Nat. Rev. Nephrol. 19, 53–72 (2023).
McSweeney, K. R. et al. Mechanisms of cisplatin-induced acute kidney injury: pathological mechanisms, pharmacological interventions, and genetic mitigations. Cancers 13, 1572 (2021).
Bhat, Z. Y. et al. Understanding the risk factors and long-term consequences of cisplatin-associated acute kidney injury: an observational cohort study. PLoS ONE 10, e0142225 (2015).
Menon, N. S. et al. Quality of life in patients with locally advanced head and neck squamous cell carcinoma undergoing concurrent chemoradiation with once-a-week versus once-every-3-weeks cisplatin. Cancer Med 11, 3939–3948 (2022).
Kiyota, N. et al. Weekly cisplatin plus radiation for postoperative head and neck cancer (jcog1008): a multicenter, noninferiority, phase II/III randomized controlled trial. J. Clin. Oncol. 40, 1980–1990 (2022).
Suppadungsuk, S. et al. Preloading magnesium attenuates cisplatin-associated nephrotoxicity: pilot randomized controlled trial (PRAGMATIC study). ESMO Open 7, 100351 (2022).
Mapuskar, K. A. et al. The antioxidant and anti-inflammatory activities of avasopasem manganese in age-associated, cisplatin-induced renal injury. Redox Biol. 70, 103022 (2024).
Mapuskar, K. A. et al. Avasopasem manganese (GC4419) protects against cisplatin-induced chronic kidney disease: an exploratory analysis of renal metrics from a randomized phase 2b clinical trial in head and neck cancer patients. Redox Biol. 60, 102599 (2023).
Sears, S. M. & Siskind, L. J. Potential therapeutic targets for cisplatin-induced kidney injury: lessons from other models of AKI and fibrosis. J. Am. Soc. Nephrol. 32, 1559–1567 (2021).
Qiu, C.-W., Chen, B., Zhu, H.-F., Liang, Y.-L. & Mao, L.-S. Gastrodin alleviates cisplatin nephrotoxicity by inhibiting ferroptosis via the SIRT1/FOXO3A/GPX4 signaling pathway. J. Ethnopharmacol. https://doi.org/10.1016/j.jep.2023.117282 (2024).
Zhang, D. et al. Protein kinase Cδ suppresses autophagy to induce kidney cell apoptosis in cisplatin nephrotoxicity. J. Am. Soc. Nephrol. 28, 1131–1144 (2017).
Shi, M. et al. Cisplatin nephrotoxicity as a model of chronic kidney disease. Lab Invest. 98, 1105–1121 (2018).
Sharp, C. N. et al. Repeated administration of low-dose cisplatin in mice induces fibrosis. Am. J. Physiol. Renal Physiol. 310, F560–F568 (2016).
Balmer, L. A. et al. Genetic characterization of early renal changes in a novel mouse model of diabetic kidney disease. Kidney Int. 96, 918–926 (2019).
Fu, Y. et al. Chronic effects of repeated low-dose cisplatin treatment in mouse kidneys and renal tubular cells. Am. J. Physiol. Renal Physiol. 317, F1582–f1592 (2019).
Sears, S. M. et al. C57BL/6 mice require a higher dose of cisplatin to induce renal fibrosis and CCL2 correlates with cisplatin-induced kidney injury. Am. J. Physiol. Renal Physiol. 319, F674–F685 (2020).
Su, H. et al. Subcellular trafficking of tubular MDM2 implicates in acute kidney injury to chronic kidney disease transition during multiple low-dose cisplatin exposure. FASEB J. 34, 1620–1636 (2020).
Wu, L. et al. Bone marrow mesenchymal stem cells ameliorate cisplatin-induced renal fibrosis via miR-146a-5p/Tfdp2 axis in renal tubular epithelial cells. Front. Immunol. 11, 623693 (2020).
Yamashita, N. et al. Cumulative DNA damage by repeated low-dose cisplatin injection promotes the transition of acute to chronic kidney injury in mice. Sci. Rep. 11, 20920 (2021).
Sharp, C. N. & Siskind, L. J. Developing better mouse models to study cisplatin-induced kidney injury. Am. J. Physiol. Renal Physiol. 313, F835–f841 (2017).
Li, C. et al. N-acetylcysteine ameliorates cisplatin-induced renal senescence and renal interstitial fibrosis through sirtuin1 activation and p53 deacetylation. Free Radic. Biol. Med. 130, 512–527 (2019).
Li, S. et al. Tubular cell senescence promotes maladaptive kidney repair and chronic kidney disease after cisplatin nephrotoxicity. JCI Insight 8, e166643 (2023).
Sharp, C. N. et al. Subclinical kidney injury induced by repeated cisplatin administration results in progressive chronic kidney disease. Am. J. Physiol. Renal Physiol. 315, F161–f172 (2018).
Sears, S. M. et al. Pharmacological inhibitors of autophagy have opposite effects in acute and chronic cisplatin-induced kidney injury. Am. J. Physiol. Renal Physiol. 323, F288–F298 (2022).
Tsai, Y. S. et al. Lactobacillus rhamnosus GKLC1 ameliorates cisplatin-induced chronic nephrotoxicity by inhibiting cell inflammation and apoptosis. Biomed. Pharmacother. 147, 112701 (2022).
Guo, X. et al. Kidney-targeted renalase agonist prevents cisplatin-induced chronic kidney disease by inhibiting regulated necrosis and inflammation. J. Am. Soc. Nephrol. 33, 342–356 (2022).
Mapuskar, K. A. et al. Persistent increase in mitochondrial superoxide mediates cisplatin-induced chronic kidney disease. Redox Biol. 20, 98–106 (2019).
Landau, S. I. et al. Regulated necrosis and failed repair in cisplatin-induced chronic kidney disease. Kidney Int. 95, 797–814 (2019).
Garovic, V. D. & August, P. Sex differences and renal protection: keeping in touch with your feminine side. J. Am. Soc. Nephrol. 27, 2921–2924 (2016).
Boddu, R. et al. Unique sex- and age-dependent effects in protective pathways in acute kidney injury. Am. J. Physiol. Renal Physiol. 313, F740–f755 (2017).
Fu, Y. et al. The STAT1/HMGB1/NF-κB pathway in chronic inflammation and kidney injury after cisplatin exposure. Theranostics 13, 2757–2773 (2023).
Shi, G. et al. RB/T 173-2018. Guidelines of Assessment for Humane Endpoints in Animal Experiment (National Certification and Accreditation Administration, 2018).
Talbot, S. R. et al. Defining body-weight reduction as a humane endpoint: a critical appraisal. Lab. Anim. 54, 99–110 (2020).
Morton, D. B. Humane endpoints in animal experimentation for biomedical research: ethical, legal and practical aspects. In Humane Endpoints in Animal Experiments for Biomedical Research (eds Hendriksen, C. F. M. & Morton, D. B.) 5–12 (The Royal Society Medical Press, 1998).
El-Waseif, E. G., Sharawy, M. H. & Suddek, G. M. The modulatory effect of sodium molybdate against cisplatin-induced CKD: role of TGF-β/Smad signaling pathway. Life Sci. 306, 120845 (2022).
Xing, Z., Gong, K., Hu, N. & Chen, Y. The reduction of uromodulin, complement factor H, and their interaction is associated with acute kidney injury to chronic kidney disease transition in a four-time cisplatin-injected rat model. Int. J. Mol. Sci. 24, 6636 (2023).
Shati, A. A. et al. Comparison of the ameliorative roles of crab chitosan nanoparticles and mesenchymal stem cells against cisplatin-triggered nephrotoxicity. Int. J. Biol. Macromol. 242, 124985 (2023).
Al Za’abi, M. et al. Effects of repeated increasing doses of cisplatin as models of acute kidney injury and chronic kidney disease in rats. Naunyn Schmiedebergs Arch. Pharmacol. 394, 249–259 (2021).
Gholami, A. et al. The ameliorating effect of Limosilactobacillus fermentum and its supernatant postbiotic on cisplatin-induced chronic kidney disease in an animal model. BMC Complement. Med. Ther. 23, 243 (2023).
Acknowledgements
The study was supported by grants from the Office of Science and Technology and Talent Work of Luzhou (2024LZXNYDJ082) and Science and Technology Department of Sichuan Province (2022YFS0621).
Author information
Authors and Affiliations
Contributions
H.-W.S. analyzed the literature and revised the manuscript. C.-W.Q. supervised the project and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Lab Animal thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Su, HW., Qiu, CW. A comparative review of murine models of repeated low-dose cisplatin-induced chronic kidney disease. Lab Anim 54, 42–49 (2025). https://doi.org/10.1038/s41684-024-01504-1
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41684-024-01504-1