Abstract
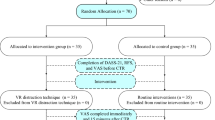
Chronic low back pain (cLBP) significantly impacts quality of life, highlighting the need for safe, home-based, non-pharmacological therapies. This study (NCT04409353) evaluated three interventions utilizing Virtual Reality (VR) for managing cLBP. 385 participants were randomized across three groups: Skills-Based VR (biofeedback, interoceptive training, and relaxation), Distraction VR (immersive 360-degree videos), and Sham VR (2D videos). The primary outcome was the change in PROMIS Pain Interference (PI). Secondary outcomes included the change in physical function, anxiety, depression, sleep disturbance, opioid use, and Fitbit-measured steps and sleep efficiency. No significant differences were observed between active VR (Skills-Based and Distraction) and Sham VR for the primary or most secondary outcomes. Secondary findings indicated a greater reduction in daily opioid use in the Distraction VR group compared to Sham VR (p = 0.009), and exploratory analyses revealed that baseline anxiety significantly predicted PROMIS-PI improvement within the Skills-Based VR (p = 0.025) group. Depression symptoms showed no such association. Adverse events were predominantly mild and self-limited, with cybersickness being the most common. Neither active VR program outperformed Sham VR for the primary outcome. High adherence across groups underscored the feasibility of home-based VR. Future studies, powered to test anxiety-moderated treatment effects and opioid-use reduction as primary outcomes, are warranted.
Similar content being viewed by others
Data availability
Per NIH and BACPAC consortium data-sharing requirements, deidentified datasets containing participant characteristics and PROs are published on the Vivli platform (https://doi.org/10.25934/PR00011733).
Code availability
The underlying code used for study is not publicly available but may be made available to qualified researchers on reasonable request from the corresponding author.
References
Hurwitz, E. L., Randhawa, K., Yu, H., Côté, P. & Haldeman, S. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur. Spine J. 27, 796–801 (2018).
Murray, C. J. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (Lond., Engl.) 380, 2197–2223 (2012).
Shmagel, A., Ngo, L., Ensrud, K. & Foley, R. Prescription Medication Use Among Community-Based U.S. Adults With Chronic Low Back Pain: A Cross-Sectional Population Based Study. J. Pain. : Off. J. Am. Pain. Soc. 19, 1104–1112 (2018).
Crofford, L. J. Adverse effects of chronic opioid therapy for chronic musculoskeletal pain. Nat. Rev. Rheumatol. 6, 191 (2010).
Medical Extended Reality Program: Research on Medical Extended Reality-Based Medical Devices, https://www.fda.gov/medical-devices/medical-device-regulatory-science-research-programs-conducted-osel/medical-extended-reality-program-research-medical-extended-reality-based-medical-devices.
Spiegel, B. M. R. et al. What is medical extended reality? A taxonomy defining the current breadth and depth of an evolving field. J. Med Ext. Real. 1, 4–12 (2024).
Mistry, D., Brock, C. A. & Lindsey, T. The present and future of virtual reality in medical education: a narrative review. Cureus 15, e51124 (2023).
Ahern, M. M. et al. The effectiveness of virtual reality in patients with spinal pain: a systematic review and meta-analysis. Pain. Pr. 20, 656–675 (2020).
Brea-Gómez, B. et al. Virtual reality in the treatment of adults with chronic low back pain: a systematic review and meta-analysis of randomized clinical trials. Int J. Environ. Res Public Health 18, 11806 (2021).
Garrett, B., Taverner, T. & McDade, P. Virtual reality as an adjunct home therapy in chronic pain management: an exploratory study. JMIR Med. Inform. 5, e11 (2017).
Goudman, L. et al. Virtual reality applications in chronic pain management: systematic review and meta-analysis. JMIR Serious Games 10, e34402 (2022).
Grassini, S. Virtual reality assisted non-pharmacological treatments in chronic pain management: a systematic review and quantitative meta-analysis. Int J. Environ. Res Public Health 19, 4071 (2022).
Groenveld, T. D. et al. Effect Of A Behavioural Therapy-Based Virtual Reality Application On Quality Of Life In Chronic Low Back Pain. Clin. J. Pain. https://doi.org/10.1097/AJP.0000000000001110 (2023).
Guo, Q. et al. Virtual reality intervention for patients with neck pain: systematic review and meta-analysis of randomized controlled trials. J. Med Internet Res 25, e38256 (2023).
Huang, Q., Lin, J., Han, R., Peng, C. & Huang, A. Using virtual reality exposure therapy in pain management: A systematic review and meta-analysis of randomized controlled trials. Value Health 25, 288–301 (2022).
Kantha, P., Lin, J.-J. & Hsu, W.-L. The effects of interactive virtual reality in patients with chronic musculoskeletal disorders: a systematic review and meta-analysis. Games Health J. 12, 1–12 (2023).
Lier, E. J., de Vries, M., Steggink, E. M., Ten Broek, R. P. G. & van Goor, H. Effect modifiers of virtual reality in pain management: a systematic review and meta-regression analysis. Pain 164, 1658–1665 (2023).
Mallari, B., Spaeth, E. K., Goh, H. & Boyd, B. S. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J. Pain. Res 12, 2053–2085 (2019).
Wiederhold, B. K., Gao, K., Sulea, C. & Wiederhold, M. D. Virtual reality as a distraction technique in chronic pain patients. Cyberpsychology, Behav. Soc. Netw. 17, 346–352 (2014).
Maddox, T. et al. In-home virtual reality program for chronic low back pain: durability of a randomized, placebo-controlled clinical trial to 18 months post-treatment. Reg Anesth Pain Med, rapm-2022-104093 (2022).
Device Classification under Section 513(F)(2)(De Novo), https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRL/rl.cfm?lid=764583&lpcd=QRA.
Garcia, L. M. et al. An 8-Week Self-Administered At-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J. Med Internet Res 23, e26292 (2021).
Maddox, T. et al. In-Home Virtual Reality Program for Chronic Lower Back Pain: A Randomized Sham-Controlled Effectiveness Trial in a Clinically Severe and Diverse Sample. Mayo Clin. Proc. Digit Health 1, 563–573 (2023).
Hoag, J. A., Karst, J., Bingen, K., Palou-Torres, A. & Yan, K. Distracting Through Procedural Pain and Distress Using Virtual Reality and Guided Imagery in Pediatric, Adolescent, and Young Adult Patients: Randomized Controlled Trial. J. Med Internet Res 24, e30260 (2022).
Bradshaw, D. H., Donaldson, G. W., Jacobson, R. C., Nakamura, Y. & Chapman, C. R. Individual differences in the effects of music engagement on responses to painful stimulation. J. Pain. : Off. J. Am. Pain. Soc. 12, 1262–1273 (2011).
Bair, M. J., Robinson, R. L., Katon, W. & Kroenke, K. Depression and pain comorbidity: a literature review. Arch. Intern Med 163, 2433–2445 (2003).
Leung, L. Pain catastrophizing: an updated review. Indian J. Psychol. Med 34, 204–217 (2012).
Lee, K. E., Ryu, H. & Chang, S. J. The Effect of Pain Catastrophizing on Depression among Older Korean Adults with Chronic Pain: The Mediating Role of Chronic Pain Interference and Sleep Quality. Int J Environ Res Public Health 17, https://doi.org/10.3390/ijerph17238716 (2020).
Taguchi, K. et al. Integrated cognitive behavioral therapy for chronic pain: An open-labeled prospective single-arm trial. Med. (Baltim.) 100, e23859 (2021).
Ehde, D. M., Dillworth, T. M. & Turner, J. A. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am. Psychol. 69, 153–166 (2014).
Birckhead, B. et al. Home-based virtual reality for chronic pain: protocol for an NIH-supported randomised-controlled trial. BMJ Open 11, e050545 (2021).
Greco, C. M. et al. Biobehavioral assessments in BACPAC: recommendations, rationale, and methods. Pain. Med 24, S61–S70 (2023).
Harris, P. A. et al. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42, 377–381 (2009).
Ross, L. et al. Bridging the Gap: Culturally Responsive Strategies for NIH Trial Recruitment. J. Racial Ethn. Health Disparities https://doi.org/10.1007/s40615-024-02166-y (2024).
Wickham, H. in ggplot2: Elegant Graphics for Data Analysis 189-201 (Springer International Publishing, 2016).
Acknowledgements
This work is primarily supported by the NIH/NIAMS Award Number UH3AR076573. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. NIAMS had no role in the design of the study, and did not have a role in the analysis, interpretation of data, or decision to submit results for publication. AppliedVR provided the VR devices and software for the trial through grant budgetary support. However, the company was not involved in the conduct of the study, data analysis, interpretation, or the decision to submit the findings for publication. The study received additional support from the Marc and Sheri Rapaport Fund for Digital Health Science and Precision Health at Cedars-Sinai and NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
Author information
Authors and Affiliations
Contributions
B.M.R.S. wrote the main manuscript text. S.A.E. prepared Figure 1. S.Y.C. performed statistical analyses and prepared Table 1 and Figures 2-3. B.M.R.S., S.A.E., S.Y.C., S.P., M.L.I., S.V., J.T., F.A., M.A.V., Z.K., T.N., M.T., L.R., M.V., O.L., I.D., T.V., and J.F. reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no conflicts of interest to declare. AppliedVR, the manufacturer of RelieVRx, participated in the Cedars-Sinai Accelerator in partnership with Techstars in 2016; however, none of the authors are employed by AppliedVR, hold equity in the company, receive royalties from the company, or benefit financially from the Cedars-Sinai Accelerator. One author (B.S.) serves on the Editorial Board of npj Digital Medicine but had no involvement in the review, handling, or decision-making related to this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Spiegel, B.M.R., Eberlein, S.A., Persky, S. et al. Randomized-controlled trial of skills-based vr vs. distraction vr vs. sham VR for chronic low back pain. npj Digit. Med. (2026). https://doi.org/10.1038/s41746-026-02437-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-026-02437-4