Abstract
Given that breathing is one of the most fundamental physiological functions, there is an urgent need to broaden our understanding of the fluid dynamics that governs it. There would be many benefits from doing so, including a better assessment of respiratory health, a basis for more precise delivery of pharmaceutical drugs for treatment, and the understanding and potential minimization of respiratory infection transmission. We review the physics of particle generation in the respiratory tract, the fate of these particles in the air on exhalation and the physics of particle inhalation. The main focus is on evidence from experimental studies. We conclude that although there is qualitative understanding of the generation of particles in the respiratory tract, a basic quantitative knowledge of the characteristics of the particles emitted during respiratory activities and their fate after emission, and a theoretical understanding of particle deposition during inhalation, nevertheless the general understanding of the entire process is rudimentary, and many open questions remain.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Morawska, L. & Buonanno, G. The physics of particle formation and deposition during breathing. Nat. Rev. Phys. 3, 300–301 (2021).
Wei, J. & Li, Y. Airborne spread of infectious agents in the indoor environment. Am. J. Infect. Control. 44, S102–S108 (2016).
Rayleigh, L. On the stability, or instability, of certain fluid motions. Proc. Lond. Math. Soc. 1, 57–72 (1879).
Stadnytskyi, V., Anfinrud, P. & Bax, A. Breathing, speaking, coughing or sneezing: what drives transmission of SARS-CoV-2?J. Intern. Med. 290, 1010–1027 (2021).
Johnson, G. et al. Modality of human expired aerosol size distributions. J. Aerosol Sci. 42, 839–851 (2011).
Abkarian, M. & Stone, H. Stretching and break-up of saliva filaments during speech: a route for pathogen aerosolization and its potential mitigation. Phys. Rev. Fluids 5, 102301 (2020).
Bake, B., Larsson, P., Ljungkvist, G., Ljungström, E. & Olin, A. Exhaled particles and small airways. Respir. Res. 20, 8 (2019).
Almstrand, A.-C. et al. Effect of airway opening on production of exhaled particles. J. Appl. Physiol. 108, 584–588 (2010).
Fahy, J. V. & Dickey, B. F. Airway mucus function and dysfunction. N. Engl. J. Med. 363, 2233–2247 (2010).
Patterson, B. & Wood, R. Is cough really necessary for TB transmission? Tuberculosis 117, 31–35 (2019).
Johnson, G. R. & Morawska, L. The mechanism of breath aerosol formation. J. Aerosol Med. Pulm. Drug Deliv. 22, 229–237 (2009).
Balachandar, S., Zaleski, S., Soldati, A., Ahmadi, G. & Bourouiba, L. Host-to-host airborne transmission as a multiphase flow problem for science-based social distance guidelines. Int. J. Multiph. Flow. 132, 103439 (2020).
Collins, L. & Dawes, C. The surface area of the adult human mouth and thickness of the salivary film covering the teeth and oral mucosa. J. Dent. Res. 66, 1300–1302 (1987).
Kaufman, E. & Lamster, I. B. The diagnostic applications of saliva — a review. Crit. Rev. Oral. Biol. Med. 13, 197–212 (2002).
Fennelly, K. P. Particle sizes of infectious aerosols: implications for infection control. Lancet Respir. Med. 8, 914–924 (2020).
Effros, R. M. et al. Dilution of respiratory solutes in exhaled condensates. Am. J. Respir. Crit. Care Med. 165, 663–669 (2002).
Stadnytskyi, V., Bax, C. E., Bax, A. & Anfinrud, P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl Acad. Sci. USA 117, 11875–11877 (2020).
Anand, S. & Mayya, Y. Size distribution of virus laden droplets from expiratory ejecta of infected subjects. Sci. Rep. 10, 21174 (2020).
Basu, S. Computational characterization of inhaled droplet transport to the nasopharynx. Sci. Rep. 11, 6652 (2021).
Bar-On, Y. M., Flamholz, A., Phillips, R. & Milo, R. Science Forum: SARS-CoV-2 (COVID-19) by the numbers. eLife 9, e57309 (2020).
Zayas, G. et al. Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC Pulm. Med. 12, 11 (2012).
Lindsley, W. G. et al. Viable influenza A virus in airborne particles expelled during coughs versus exhalations. Influenza Other Respir. Viruses 10, 404–413 (2016).
Castleman, R. A. The mechanism of the atomization of liquids. J. Res. Natl Bur. Stand. 7, 269–376 (1931).
Wells, W. F. Airborne Contagion and Air Hygiene: An Ecological Study of Droplet Infections (Harvard Univ. Press, 1955).
Descamps, M., Matas, J.-P. & Cartellier, A. H. Gas–liquid atomisation: gas phase characteristics by PIV measurements and spatial evolution of the spray. In 2nd colloque INCA, Initiative en Combustion Avancée, 1 (HAL Open Science, 2008); https://hal.archives-ouvertes.fr/hal-00704346.
Scheubel, F. N. On atomization in carburetors. National Advisory Committee for Aeronautics Technical Memorandum 644 (1927); https://ntrs.nasa.gov/api/citations/19930094772/downloads/19930094772.pdf?attachment=true
Sauter, J. Untersuchung der von Spritzvergasern gelieten Zerstäubung. Forschungsarbeiten auf dem Gebiete des Ingenieurwesens, Vol. 312 (Springer, 1928).
Hong, M., Cartellier, A. & Hopfinger, E. J. Characterization of phase detection optical probes for the measurement of the dispersed phase parameters in sprays. Int. J. Multiph. Flow 30, 615–648 (2004).
Edwards, D. A. et al. Inhaling to mitigate exhaled bioaerosols. Proc. Natl Acad. Sci. USA 101, 17383–17388 (2004).
Zayas, G., Dimitry, J., Zayas, A., O’Brien, D. & King, M. A new paradigm in respiratory hygiene: increasing the cohesivity of airway secretions to improve cough interaction and reduce aerosol dispersion. BMC Pulm. Med. 5, https://doi.org/10.1186/1471-2466-5-11 (2005).
Hasan, M. A., Lange, C. F. & King, M. L. Effect of artificial mucus properties on the characteristics of airborne bioaerosol droplets generated during simulated coughing. J. Nonnewton. Fluid Mech. 165, 1431–1441 (2010).
Vasudevan, M. & Lange, C. F. Surface tension effects on instability in viscoelastic respiratory fluids. Math. Biosci. 205, 180–194 (2007).
Lasheras, J., Villermaux, E. & Hopfinger, E. Break-up and atomization of a round water jet by a high-speed annular air jet. J. Fluid Mech. 357, 351–379 (1998).
Villermaux, E. Fragmentation versus cohesion. J. Fluid Mech. 898, P1 (2020).
Chen, Z. et al. Determination of rheology and surface tension of airway surface liquid: a review of clinical relevance and measurement techniques. Respir. Res. 20, 274 (2019).
Brown, E. S., Johnson, R. P. & Clements, J. A. Pulmonary surface tension. J. Appl. Physiol. 14, 717–720 (1959).
Schürch, S., Bachofen, H., Goerke, J. & Green, F. Surface properties of rat pulmonary surfactant studied with the captive bubble method: adsorption, hysteresis, stability. Biochim. Biophys. Acta 1103, 127–136 (1992).
Keshavarz, B. et al. Studying the effects of elongational properties on atomization of weakly viscoelastic solutions using Rayleigh Ohnesorge jetting extensional rheometry (ROJER). J. Nonnewton. Fluid Mech. 222, 171–189 (2015).
Watanabe, W. et al. Why inhaling salt water changes what we exhale. J. Colloid Interface Sci. 307, 71–78 (2007).
Keshavarz, B., Houze, E. C., Moore, J. R., Koerner, M. R. & McKinley, G. H. Ligament mediated fragmentation of viscoelastic liquids. Phys. Rev. Lett. 117, 154502 (2016).
Edwards, D. A. et al. Exhaled aerosol increases with COVID-19 infection, age, and obesity. Proc. Natl Acad. Sci. USA 118, e2021830118 (2021).
Fairchild, C. & Stampfer, J. Particle concentration in exhaled breath. Am. Ind. Hyg. Assoc. J. 48, 948–949 (1987).
Asadi, S. et al. Effect of voicing and articulation manner on aerosol particle emission during human speech. PLoS ONE 15, e0227699 (2020).
Asadi, S. et al. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 9, 2348 (2019).
Alsved, M. et al. Exhaled respiratory particles during singing and talking. Aerosol Sci. Technol. 54, 1245–1248 (2020).
Oratis, A. T., Bush, J. W., Stone, H. A. & Bird, J. C. A new wrinkle on liquid sheets: turning the mechanism of viscous bubble collapse upside down. Science 369, 685–688 (2020).
Fiegel, J., Clarke, R. & Edwards, D. A. Airborne infectious disease and the suppression of pulmonary bioaerosols. Drug Discov. Today 11, 51–57 (2006).
Bake, B. et al. Exhaled particles after a standardized breathing maneuver. J. Aerosol Med. Pulm. Drug Deliv. 30, 267–273 (2017).
Merghani, K. M. M., Sagot, B., Gehin, E., Da, G. & Motzkus, C. A review on the applied techniques of exhaled airflow and droplets characterization. Indoor Air 31, 7–25 (2021).
Gupta, J., Lin, C. H. & Chen, Q. Flow dynamics and characterization of a cough. Indoor Air 19, 517–525 (2009).
Gupta, J. K., Lin, C. H. & Chen, Q. Characterizing exhaled airflow from breathing and talking. Indoor Air 20, 31–39 (2010).
Xu, C., Nielsen, P., Gong, G., Liu, L. & Jensen, R. Measuring the exhaled breath of a manikin and human subjects. Indoor Air 25, 188–197 (2015).
Xu, C., Nielsen, P. V., Liu, L., Jensen, R. L. & Gong, G. Human exhalation characterization with the aid of schlieren imaging technique. Build. Environ. 112, 190–199 (2017).
Papineni, R. S. & Rosenthal, F. S. The size distribution of droplets in the exhaled breath of healthy human subjects. J. Aerosol Med. 10, 105–116 (1997).
Yang, S., Lee, G. W., Chen, C.-M., Wu, C.-C. & Yu, K.-P. The size and concentration of droplets generated by coughing in human subjects. J. Aerosol Med. 20, 484–494 (2007).
Morawska, L. et al. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J. Aerosol Sci. 40, 256–269 (2009).
Hersen, G. et al. Impact of health on particle size of exhaled respiratory aerosols: case-control study. Clean 36, 572–577 (2008).
Chao, C. Y. H. et al. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. J. Aerosol Sci. 40, 122–133 (2009).
Duguid, J. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. Epidemiol. Infect. 44, 471–479 (1946).
Loudon, R. G. & Roberts, R. M. Droplet expulsion from the respiratory tract. Am. Rev. Respir. Dis. 95, 435–442 (1967).
Lindsley, W. G. et al. Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J. Occup. Environ. Hyg. 9, 443–449 (2012).
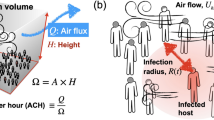
Buonanno, G., Morawska, L. & Stabile, L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: prospective and retrospective applications. Environ. Int. 145, 106112 (2020).
Wells, W. F. On air-borne infection. Study II. Droplet and droplet nuclei. Am. J. Epidemiol. 20, 611–618 (1934).
Xie, X., Li, Y., Chwang, A., Ho, P. & Seto, W. How far droplets can move in indoor environments — revisiting the Wells evaporation–falling curve. Indoor Air 17, 211–225 (2007).
Scientific Brief, 7 May 2021: SARS-CoV-2 transmission (CDC, 2021).
Coronavirus disease (COVID-19): How is it transmitted? https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted (WHO, 2021).
Bourouiba, L., Dehandschoewercker, E. & Bush, J. W. M. Violent expiratory events: on coughing and sneezing. J. Fluid Mech. 745, 537–563 (2014).
Asgharian, B. A model of deposition of hygroscopic particles in the human lung. Aerosol Sci. Technol. 38, 938–947 (2004).
Baturin, V. V. Fundamentals of Industrial Ventilation (Pergamon, 1972).
Rajaratnam, N. Turbulent Jets (Elsevier, 1976).
Turner, J. S. Buoyancy Effects in Fluids (Cambridge Univ. Press, 1979).
Ng, C. S. et al. Growth of respiratory droplets in cold and humid air. Phys. Rev. Fluids 6, 054303 (2021).
Bradley, R., Evans, M. G. & Whytlaw-Gray, R. The rate of evaporation of droplets. evaporation and diffusion coefficients, and vapour pressures of dibutyl phthalate and butyl stearate. Proc. R. Soc. A 186, 368–390 (1946).
Langmuir, I. The evaporation of small spheres. Phys. Rev. 12, 368 (1918).
Pirhadi, M., Sajadi, B., Ahmadi, G. & Malekian, D. Phase change and deposition of inhaled droplets in the human nasal cavity under cyclic inspiratory airflow. J. Aerosol Sci. 118, 64–81 (2018).
Sazhin, S. S. Advanced models of fuel droplet heating and evaporation. Prog. Energy Combust. Sci. 32, 162–214 (2006).
Božič, A. & Kanduč, M. Relative humidity in droplet and airborne transmission of disease. J. Biol. Phys. 47, 1–29 (2021).
Kukkonen, J., Vesala, T. & Kulmala, M. The interdependence of evaporation and settling for airborne freely falling droplets. J. Aerosol Sci. 20, 749–763 (1989).
Netz, R. R. Mechanisms of airborne infection via evaporating and sedimenting droplets produced by speaking. J. Phys. Chem. B 124, 7093–7101 (2020).
Netz, R. R. & Eaton, W. A. Physics of virus transmission by speaking droplets. Proc. Natl Acad. Sci. USA 117, 25209–25211 (2020).
Nicas, M., Nazaroff, W. W. & Hubbard, A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J. Occup. Environ. Hyg. 2, 143–154 (2005).
Liu, L., Wei, J., Li, Y. & Ooi, A. Evaporation and dispersion of respiratory droplets from coughing. Indoor Air 27, 179–190 (2017).
Villermaux, E., Moutte, A., Amielh, M. & Meunier, P. Fine structure of the vapor field in evaporating dense sprays. Phys. Rev. Fluids 2, 074501 (2017).
de Oliveira, P. M., Mesquita, L. C., Gkantonas, S., Giusti, A. & Mastorakos, E. Evolution of spray and aerosol from respiratory releases: theoretical estimates for insight on viral transmission. Proc. R. Soc. A 477, 20200584 (2021).
Chong, K. L. et al. Extended lifetime of respiratory droplets in a turbulent vapor puff and its implications on airborne disease transmission. Phys. Rev. Lett. 126, 034502 (2021).
Smith, S. H. et al. Aerosol persistence in relation to possible transmission of SARS-CoV-2. Phys. Fluids 32, 107108 (2020).
Ai, Z. T. & Melikov, A. K. Airborne spread of expiratory droplet nuclei between the occupants of indoor environments: a review. Indoor Air 28, 500–524 (2018).
Mui, K. W., Wong, L. T., Wu, C. & Lai, A. C. Numerical modeling of exhaled droplet nuclei dispersion and mixing in indoor environments. J. Hazard. Mater. 167, 736–744 (2009).
Nielsen, P. V. & Xu, C. Multiple airflow patterns in human microenvironment and the influence on short-distance airborne cross-infection — a review. Indoor Built Environ. https://doi.org/10.1177/1420326X211048539 (2021).
Riediker, M. et al. Particle toxicology and health — where are we? Particle and fibre. Toxicology 16, 19 (2019).
Hopke, P. K., Dai, Q., Li, L. & Feng, Y. Global review of recent source apportionments for airborne particulate matter. Sci. Total. Environ. 740, 140091 (2020).
Kerminen, V.-M. et al. Atmospheric new particle formation and growth: review of field observations. Environ. Res. Lett. 13, 103003 (2018).
Kittelson, B. D. Engines and nanoparticles: a review. J. Aerosol Sci. 29, 575–588 (1998).
Kumar, P., Pirjola, L., Ketzel, M. & Harrison, R. M. Nanoparticle emissions from 11 non-vehicle exhaust sources–A review. Atmos. Environ. 67, 252–277 (2013).
Querol, X. et al. Speciation and origin of PM10 and PM2.5 in selected European cities. Atmos. Environ. 38, 6547–6555 (2004).
Peters, A. et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part. Fibre Toxicol. 3, 13 (2006).
Kreyling, W. et al. Translocation of ultrafine insoluble iridium particles from lung epithelium to extrapulmonary organs is size dependent but very low. J. Toxicol. Environ. Health A 65, 1513–1530 (2002).
Oberdörster, G. et al. Translocation of inhaled ultrafine particles to the brain. Inhal. Toxicol. 16, 437–445 (2004).
Beelen, R. et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 383, 785–795 (2014).
Weichenthal, S. Selected physiological effects of ultrafine particles in acute cardiovascular morbidity. Environ. Res. 115, 26–36 (2012).
Fu, P., Guo, X., Cheung, F. M. H. & Yung, K. K. L. The association between PM2.5 exposure and neurological disorders: a systematic review and meta-analysis. Sci. Total Environ. 655, 1240–1248 (2019).
Raaschou-Nielsen, O. et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European study of cohorts for air pollution effects (ESCAPE). Lancet Oncol. 14, 813–822 (2013).
Donaldson, K., Stone, V., Clouter, A., Renwick, L. & MacNee, W. Ultrafine particles. Occup. Environ. Med. 58, 211–216 (2001).
Global Burden of Disease (GBD) Visualization Hub. https://vizhub.healthdata.org/gbd-compare/ (GBD, 2020).
Wölfel, R. et al. Virological assessment of hospitalized patients with COVID-2019. Nature 581, 465–469 (2020).
Morawska, L. & Cao, J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 139, 105730 (2020).
Van Doremalen, N. et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 382, 1564–1567 (2020).
Watanabe, T., Bartrand, T. A., Weir, M. H., Omura, T. & Haas, C. N. Development of a dose-response model for SARS coronavirus. Risk Anal. 30, 1129–1138 (2010).
Schmid, O. & Cassee, F. R. On the pivotal role of dose for particle toxicology and risk assessment: exposure is a poor surrogate for delivered dose. Part. Fibre Toxicol. 14, 52 (2017).
Schmid, O. et al. Dosimetry and toxicology of inhaled ultrafine particles. Biomarkers 14, 67–73 (2009).
Licina, D., Tian, Y. & Nazaroff, W. W. Inhalation intake fraction of particulate matter from localized indoor emissions. Build. Environ. 123, 14–22 (2017).
Morawska, L. et al. A paradigm shift to combat indoor respiratory infection. Science 372, 689–691 (2021).
Human Respiratory Tract Model for Radiological Protection (ICRP, 1994).
Tsuda, A., Henry, F. S. & Butler, J. P. Particle transport and deposition: basic physics of particle kinetics. Compr. Physiol. 3, 1437–1471 (2011).
Wang, C.-s. Inhaled Particles (Elsevier Academic, 2005).
Yeh, H.-C. & Schum, G. Models of human lung airways and their application to inhaled particle deposition. Bull. Math. Biol. 42, 461–480 (1980).
Altshuler, B., Palmes, E., Yarmus, L. & Nelson, N. Intrapulmonary mixing of gases studied with aerosols. J. Appl. Physiol. 14, 321–327 (1959).
Ferron, G., Haider, B. & Kreyling, W. Inhalation of salt aerosol particles — I. Estimation of the temperature and relative humidity of the air in the human upper airways. J. Aerosol Sci. 19, 343–363 (1988).
Vu, T. V., Delgado-Saborit, J. M. & Harrison, R. M. A review of hygroscopic growth factors of submicron aerosols from different sources and its implication for calculation of lung deposition efficiency of ambient aerosols. Air Qual. Atmos. Health 8, 429–440 (2015).
Christou, S. et al. Anatomical variability in the upper tracheobronchial tree: sex-based differences and implications for personalized inhalation therapies. J. Appl. Physiol. 130, 678–707 (2021).
Hussain, M., Renate, W.-H. & Werner, H. Effect of intersubject variability of extrathoracic morphometry, lung airways dimensions and respiratory parameters on particle deposition. J. Thorac. Dis. 3, 156 (2011).
Poorbahrami, K., Vignon-Clementel, I. E., Shadden, S. C. & Oakes, J. M. A whole lung in silico model to estimate age dependent particle dosimetry. Sci. Rep. 11, 11180 (2021).
Martonen, T., Zhang, Z. & Lessmann, R. Fluid dynamics of the human larynx and upper tracheobronchial airways. Aerosol Sci. Technol. 19, 133–156 (1993).
Banko, A. J., Coletti, F., Elkins, C. J. & Eaton, J. K. Oscillatory flow in the human airways from the mouth through several bronchial generations. Int. J. Heat. Fluid Flow. 61, 45–57 (2016).
Hofmann, W. Modelling inhaled particle deposition in the human lung — a review. J. Aerosol Sci. 42, 693–724 (2011).
Guo, L. L., Johnson, G. R., Hofmann, W., Wang, H. & Morawska, L. Deposition of ambient ultrafine particles in the respiratory tract of children: a novel experimental method and its application. J. Aerosol Sci. 139, 105465 (2020).
Guo, L. et al. Experimentally determined deposition of ambient urban ultrafine particles in the respiratory tract of children. Environ. Int. 145, 106094 (2020).
Londahl, J. et al. A set-up for field studies of respiratory tract deposition of fine and ultrafine particles in humans. J. Aerosol Sci. 37, 1152–1163 (2006).
Morawska, L., Hofmann, W., Hitchins-Loveday, J., Swanson, C. & Mengersen, K. Experimental study of the deposition of combustion aerosols in the human respiratory tract. J. Aerosol Sci. 36, 939–957 (2005).
Heyder, J., Gebhart, J., Rudolf, G., Schiller, C. F. & Stahlhofen, W. Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J. Aerosol Sci. 17, 811–825 (1986).
Jaques, P. A. & Kim, C. S. Measurement of total lung deposition of inhaled ultrafine particles in healthy men and women. Inhal. Toxicol. 12, 715–731 (2000).
Kim, C. S. & Jaques, P. A. Analysis of total respiratory deposition of inhaled ultrafine particles in adult subjects at various breathing patterns. Aerosol Sci. Technol. 38, 525–540 (2004).
Kim, C. S. & Jaques, P. A. Total lung deposition of ultrafine particles in elderly subjects during controlled breathing. Inhal. Toxicol. 17, 387–399 (2005).
Lin, C.-W. et al. Experimental measurements of regional lung deposition in Taiwanese. Aerosol Air Qual. Res. 19, 832–839 (2019).
Montoya, L. et al. Continuous measurements of ambient particle deposition in human subjects. Aerosol Sci. Technol. 38, 980–990 (2004).
Rissler, J. et al. Deposition efficiency of inhaled particles (15–5000 nm) related to breathing pattern and lung function: an experimental study in healthy children and adults. Part. Fibre Toxicol. 14, 10 (2017).
Jakobsson, J. K. et al. Altered deposition of inhaled nanoparticles in subjects with chronic obstructive pulmonary disease. BMC Pulm. Med. 18, 129 (2018).
Möller, W. et al. Deposition, retention, and translocation of ultrafine particles from the central airways and lung periphery. Am. J. Respir. Crit. Care Med. 177, 426–432 (2008).
Sturm, R. Total deposition of ultrafine particles in the lungs of healthy men and women: experimental and theoretical results. Ann. Transl. Med. 4, 234 (2016).
Daigle, C. C. et al. Ultrafine particle deposition in humans during rest and exercise. Inhal. Toxicol. 15, 539–552 (2003).
Altshuler, B., Yarmxus, L., Palmes, E. & Nelson, K. Aerosol deposition in the human respiratory tract. I. Experimental procedures and total deposition. Arch. Ind. Health 15, 293–303 (1957).
Emmett, P., Aitken, R. & Hannan, W. Measurements of the total and regional deposition of inhaled particles in the human respiratory tract. J. Aerosol Sci. 13, 549–560 (1982).
Foord, N., Black, A. & Walsh, M. Regional deposition of 2.5–7.5 μm diameter inhaled particles in healthy male non-smokers. J. Aerosol Sci. 9, 343–357 (1978).
Giacomelli-Maltoni, G., Melandri, C., Prodis, V. & Tarroni, G. Deposition efficiency of monodisperse particles in human respiratory tract. Am. Ind. Hyg. Assoc. J. 33, 603–610 (1972).
Stahlhofen, W., Gebhart, J. & Heyder, J. Experimental determination of the regional deposition of aerosol particles in the human respiratory tract. Am. Ind. Hyg. Assoc. J. 41, 385–398a (1980).
Löndahl, J. et al. Measurement techniques for respiratory tract deposition of airborne nanoparticles: a critical review. J. Aerosol Med. Pulm. Drug Deliv. 27, 229–254 (2014).
Dautrebande, L., Beckmann, H. & Walkenhorst, W. in Die Staublungenerkrankungen (eds Jötten, K. W. & Klosterkötter, W.) 297–307 (Springer, 1958).
Heyder, J., Armbruster, L., Gebhart, J., Grein, E. & Stahlhofen, W. Total deposition of aerosol particles in the human respiratory tract for nose and mouth breathing. J. Aerosol Sci. 6, 311–328 (1975).
Landahl, H., Tracewell, T. & Lassen, W. On the retention of air-borne particulates in the human lung: II. Arch. Ind. Hyg. Occup. Med. 3, 359–366 (1951).
Landahl, H., Tuacewell, T. & Lassen, W. Retention of air-borne particulates in the human lung: III. Arch. Ind. Hyg. Occup. Med. 6, 508–511 (1952).
Morawska, L., Barron, W. & Hitchins, J. Experimental deposition of environmental tobacco smoke submicrometer particulate matter in the human respiratory tract. Am. Ind. Hyg. Assoc. J. 60, 334–339 (1999).
Geiser, M. & Kreyling, W. G. Deposition and biokinetics of inhaled nanoparticles. Part. Fibre Toxicol. 7, 2 (2010).
Cheng, Y.-S., Zhou, Y. & Chen, B. T. Particle deposition in a cast of human oral airways. Aerosol Sci. Technol. 31, 286–300 (1999).
Carvalho, T. C., Peters, J. I. & Williams, R. O. III Influence of particle size on regional lung deposition — what evidence is there? Int. J. Pharm. 406, 1–10 (2011).
Zhou, Y. & Cheng, Y.-S. Particle deposition in a cast of human tracheobronchial airways. Aerosol Sci. Technol. 39, 492–500 (2005).
Taylor, G. et al. Gamma scintigraphic pulmonary deposition study of glycopyrronium/formoterol metered dose inhaler formulated using co-suspension delivery technology. Eur. J. Pharm. Sci. 111, 450–457 (2018).
Ghazwani, A., Biddiscombe, M. & Usmani, O. Comparing lung geometrical areas of interest in gamma scintigraphy as assessment tool for inhaled drug deposition. Eur. Respir. J. 52, PA1022 (2018).
Häussermann, S., Sommerer, K. & Scheuch, G. Regional lung deposition: in vivo data. J. Aerosol Med. Pulm. Drug Deliv. 33, 291–299 (2020).
Dubsky, S. & Fouras, A. Imaging regional lung function: a critical tool for developing inhaled antimicrobial therapies. Adv. Drug Deliv. Rev. 85, 100–109 (2015).
Porra, L. et al. Quantitative imaging of regional aerosol deposition, lung ventilation and morphology by synchrotron radiation CT. Sci. Rep. 8, 3519 (2018).
Phalen, R. & Raabe, O. The evolution of inhaled particle dose modeling: a review. J. Aerosol Sci. 99, 7–13 (2016).
Sze To, G. N. & Chao, C. Y. H. Review and comparison between the Wells–Riley and dose–response approaches to risk assessment of infectious respiratory diseases. Indoor Air 20, 2–16 (2010).
Duguid, J. The numbers and the sites of origin of the droplets expelled during expiratory activities. Edinb. Med. J. 52, 385 (1945).
Xie, X., Li, Y., Sun, H. & Liu, L. Exhaled droplets due to talking and coughing. J. R. Soc. Interface 6, S703–S714 (2009).
Ehrenstein, D. How speaking creates droplets that may spread COVID-19. Physics 13, 157 (2020).
Randall, K., Ewing, E. T., Marr, L., Jimenez, J. & Bourouiba, L. How did we get here: what are droplets and aerosols and how far do they go? A historical perspective on the transmission of respiratory infectious diseases. Interface Focus 11, 20210049 (2021).
Kulkarni, P., Baron, P. A. & Willeke, K. Aerosol Measurement: Principles, Techniques, and Applications (Wiley, 2011).
Milton, D. K. A Rosetta stone for understanding infectious drops and aerosols. J. Pediatr. Infect. Dis. Soc. 9, 413–415 (2020).
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Physics thanks the anonymous referees for their contributions to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morawska, L., Buonanno, G., Mikszewski, A. et al. The physics of respiratory particle generation, fate in the air, and inhalation. Nat Rev Phys 4, 723–734 (2022). https://doi.org/10.1038/s42254-022-00506-7
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s42254-022-00506-7
This article is cited by
-
Beyond additive effects: examining the combined impact of air pollutant interactions on pulmonary tuberculosis in China
BMC Public Health (2025)
-
Characterization of respiratory particles released during continuous speech and its relation to mask performance
Scientific Reports (2025)
-
Oxidative potential of PM1, PM2.5, and PM10 collected in car and tram tunnels to analyse their impact on public health
Scientific Reports (2025)
-
Size Distributions and Health Risks of Atmospheric Particulate Polycyclic Aromatic Hydrocarbons in an Inland Urban Area of Baoding, China
Bulletin of Environmental Contamination and Toxicology (2025)
-
Snoring-generated fluid droplets as a potential mechanistic link between sleep-disordered breathing and pneumonia
Respiratory Research (2024)