Abstract
Two adolescent mental health fields — sleep and depression — have advanced largely in parallel until about four years ago. Although sleep problems have been thought to be a symptom of adolescent depression, emerging evidence suggests that sleep difficulties arise before depression does. In this Review, we describe how the combination of adolescent sleep biology and psychology uniquely predispose adolescents to develop depression. We describe multiple pathways and contributors, including a delayed circadian rhythm, restricted sleep duration and greater opportunity for repetitive negative thinking while waiting for sleep. We match each contributor with evidence-based sleep interventions, including bright light therapy, exogenous melatonin and cognitive-behaviour therapy techniques. Such treatments improve sleep and alleviate depression symptoms, highlighting the utility of sleep treatment for comorbid disorders experienced by adolescents.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Roenneberg, T. et al. A marker for the end of adolescence. Curr. Biol. 14, R1038–R1039 (2004). This seminal paper postulates that the end of adolescence is a turning point in development at which a late chronotype begins to turn to an early chronotype.
Carskadon, M. A. Sleep in adolescents: the perfect storm. Pediatr. Clin. North Am. 58, 637–647 (2011).
Gariepy, G. et al. How are adolescents sleeping? Adolescent sleep patterns and sociodemographic differences in 24 European and North American countries. J. Adolesc. Health 66, S81–S88 (2020). This paper provides a comprehensive and contemporary snapshot of adolescent sleep patterns across numerous countries in the Northern Hemisphere.
Gradisar, M., Gardner, G. & Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 12, 110–118 (2011).
Ong, J. L., Tandi, J., Patanaik, A., Lo, J. C. & Chee, M. W. L. Large-scale data from wearables reveal regional disparities in sleep patterns that persist across age and sex. Sci. Rep. 9, 3415 (2019). This is the largest objective assessment of young people’s sleep, and includes a comparative analysis of regions, gender and changes across the lifespan.
Short, M. A., Weber, N., Reynolds, C., Coussens, S. & Carskadon, M. A. Estimating adolescent sleep need using dose-response modelling. Sleep 41, zsy011 (2018).
Short, M. A. et al. A cross-cultural comparison of sleep duration between US and Australian adolescents: the effect of school start time, parent set bedtimes, and extracurricular load. Health Educ. Behav. 40, 323–330 (2013).
Bowers, J. M. & Moyer, A. Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep Health 3, 423–431 (2017).
Becker, S. P. et al. Prospective examination of adolescent sleep paterrns and behaviors before and during COVID-19. Sleep 44, zsab054 (2020). This paper provides an excellent prospective description of the effects of the COVID-19 pandemic on the sleep of adolescents.
Gruber, R., Saha, S., Somerville, G., Boursier, J. & Wise, M. S. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 76, 33–35 (2020). This is a rich qualitative analysis of the effects of the COVID-19 pandemic on adolescent sleep.
Meltzer, L. J. et al. COVID-19 instructional approaches (in-person, online, hybrid), school start times, and sleep in over 5,000 U.S. adolescents. Sleep 44, zsab180 (2021). This timely study finds differences in adolescent sleep depending on the structure of the school day.
Barnes, M. et al. Setting adolescents up for success: promoting a policy to delay high school start times. Sch. Health Policy 86, 552–557 (2016).
Carskadon, M. A., Vieira, C. & Acebo, C. Association between puberty and delayed phase preference. Sleep 16, 258–262 (1993).
Merikangas, K. R., Nakamura, E. F. & Kessler, R. C. Epidemiology of mental disorders in children and adolescents. Dialogues Clin. Neurosci. 11, 7–20 (2009).
Polanczyk, G. V., Salum, G. A., Sugaya, L. S., Caye, A. & Rohde, L. A. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatr. 56, 345–365 (2015).
Thapar, A., Collishaw, S., Pine, D. S. & Thapar, A. K. Depression in adolescence. Lancet 379, 17–23 (2012).
Hyde, J. S., Mezulis, A. H. & Abramson, L. Y. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol. Rev. 115, 291–313 (2008).
Rice, F., Harold, G. & Thapar, A. The genetic aetiology of childhood depression: a review. J. Child Psychol. Psychiat. 43, 65–79 (2002).
Tully, E. C., Iacono, W. G. & McGue, M. Ad adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. Am. J. Psychiat. 165, 1148–1154 (2008).
Goodyer, I., Wright, C. & Altham, P. The friendships and recent life events of anxious and depressed school-age children. Br. J. Psychiat. 156, 689–698 (1990).
Pine, D. S., Cohen, P., Johnson, J. G. & Brook, J. S. Adolescent life events as predictors of adult depression. J. Affect. Dis. 68, 49–57 (2002).
Hawker, D. S. J. & Boulton, M. J. Twenty years’ research on peer victimization and psychosocial maladjustment: a meta-analytic review of cross-sectional studies. J. Child Psychol. Psychiat. 41, 441–455 (2000).
Dunn, V. & Goodyer, I. M. Longitudinal investigation into childhood- and adolescent-onset depression: psychiatric outcome in early adulthood. Br. J. Psychiat. 188, 216–222 (2018).
Harrington, R., Dubicka, B. Natural history of mood disorders in children and adolescens. In The Depressed Child and Adolescent 2nd edn (ed. Goodyer, I. M.) (Cambridge Univ. Press, 2001).
Fergussin, D. M. & Woodward, L. J. Mental health, educational, and social role outcomes of adolescents with depression. Arch. Gen. Psychiat. 59, 225–231 (2002).
Halperin, J. M., Rucklidge, J. J., Powers, R. L., Miller, C. J. & Newcorn, J. H. Childhood CBCL bipolar profile and adolescent/young adult personality disorders: a 9-year follow-up. J. Affect. Dis. 130, 155–161 (2011).
Rudolph, K. D. & Klein, D. N. Exploring depressive personality traits in youth: origins, correlates, and developmental consequences. Dev. Psychopathol. 21, 1155–1180 (2009).
Fergusson, D. M., Boden, J. M. & Horwood, L. J. Recurrence of major depression in adolescence and early adulthood and later mental health, educational and economic outcomes. Br. J. Psychiat. 191, 335–342 (2007).
Franko, D. L., Striegel-Moore, R. H., Thompson, D., Schreiber, G. B. & Daniels, S. R. Does adolescent depression predict obesity in black and white young adult women? Psychol. Med. 35, 1505–1532 (2005).
Gotlib, I. H., Lewinsohn, P. M. & Seeley, J. R. Consequences of depression during adolescence: marital status and marital functioning in early adulthood. J. Abnorm. Psychol. 107, 686–690 (1998).
Bridge, J. A., Goldstein, T. R. & Brent, D. A. Adolescent suicide and suicidal behavior. J. Child. Psychol. Psychiat. 47, 372–394 (2006).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Fried, E. I. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front. Psychol. 6, 309 (2015).
Goodyer, I. M. et al. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychsocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled superiority trial. Lancet Psychiat. 4, 109–119 (2017).
Loades, M. E. et al. Depression symptom clusters in adolescents: a latent class analysis in a clinical sample. Psychother. Res. https://doi.org/10.1080/10503307.2022.2030498 (2022).
Orchard, F., Pass, L., Marshall, T. & Reynolds, S. Clinical characteristics of adolescents referred for treatment of depressive disorders. Child. Adolesc. Ment. Health 22, 61–68 (2017).
Lovato, N. L. & Gradisar, M. A meta-analysis and model of the relationship between sleep depression in adolescents: recommendations for future research and clinical practice. Sleep Med. Rev. 18, 521–529 (2014). This study identifies and quantifies key sleep variables that predict depression onset in adolescents.
de Zambotti, M., Goldstone, A., Colrain, I. M. & Baker, F. C. Insomnia disorder in adolescence: diagnosis, impact and treatment. Sleep Med. Rev. 39, 12–24 (2018).
Ford, T., Goodman, R. & Meltzer, H. The British child and adolescent mental health survey 1999: the prevalence of DSM-IV disorders. J. Am. Acad. Child. Adolesc. Psychiat. 42, 1203–1211 (2003).
Angold, A., Costello, E. J., Erkanli, A. & Worthman, C. M. Pubertal changes in hormone levels and depression in girls. Psychol. Med. 29, 1043–1053 (1999).
Essau, C. A. & Chang, W. C. Epidemiology, comorbidity, and course of adolescent depression. In Treatments for Adolescent Depression: Theory and Practice (ed. Essau, C. A.) (Oxford Univ. Press, 2009).
Angold, A. & Costello, E. J. Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. Am. J. Psychiat. 150, 1779–1791 (1993).
Borbély, A. A. A two process model of sleep regulation. Hum. Neurobiol. 1, 195–204 (1982).
Greene, R. W., Bjorness, T. E. & Suzuki, A. The adenosine-mediated, neuronal-glial, homeostatic sleep response. Curr. Opin. Neurobiol. 44, 236–242 (2017).
Borbély, A. A., Daan, S., Wirz‐Justice, A. & Deboer, T. The two‐process model of sleep regulation: a reappraisal. J. Sleep Res. 25, 131–143 (2016). This paper provides an updated account of the most powerful framework for understanding the biological underpinnings of adolescent sleep.
Jenni, O. G. & LeBourgeois, M. K. Understanding sleep–wake behavior and sleep disorders in children: the value of a model. Curr. Opin. Psychiat. 19, 282 (2006).
Campbell, I. G., Grimm, K. J., de Bie, E. & Feinberg, I. Sex, puberty, and the timing of sleep EEG measured adolescent brain maturation. Proc. Natl Acad. Sci. 109, 5740–5743 (2012).
Feinberg, I., Higgins, L. M., Khaw, W. Y. & Campbell, I. G. The adolescent decline of NREM delta, an indicator of brain maturation, is linked to age and sex but not to pubertal stage. Dev. Physiol. Pregn. 291, R1724–R1729 (2006).
Tononi, G. & Cirelli, C. Sleep function and synaptic homeostasis. Sleep Med. Rev. 10, 49–62 (2006).
Fontanellaz-Castiglione, C. E. G., Markovic, A. & Tarokh, L. Sleep and the adolescent brain. Curr. Opin. Physiol. 15, 167–171 (2020).
Jenni, O. G., Achermann, P. & Carskadon, M. A. Homeostatic sleep regulation in adolescents. Sleep 28, 1446–1454 (2005).
Taylor, D. J., Jenni, O. G., Acebo, C. & Carskadon, M. A. Sleep tendency during extended wakefulness: insights into adolescent sleep regulation and behavior. J. Sleep Res. 14, 239–244 (2005). This is the first and only study to objectively measure the waking portion of the sleep homeostatic process in adolescents.
Nelson, A. B., Faraguna, U., Zoltan, J. T., Tononi, G. & Cirelli, C. Sleep patterns and homeostatic mechanisms in adolescent mice. Brain Sci. 3, 318–343 (2013).
Tarokh, L., Carskadon, M. A. & Achermann, P. Dissipation of sleep pressure is stable across adolescence. Neuroscience 216, 167–177 (2012).
Lo, J. C., Ong, J. L., Leong, R. L., Gooley, J. J. & Chee, M. W. Cognitive performance, sleepiness, and mood in partially sleep deprived adolescents: the need for sleep study. Sleep 39, 687–698 (2016). This study finds mood effects after a simulated week of restricted sleep and recovery sleep.
Fuligni, A. J., Bai, S., Krull, J. L. & Gonzales, N. A. Individual differences in optimum sleep for daily mood during adolescence. J. Clin. Child. Adolesc. Psychol. 48, 469–479 (2017).
Skorucak, J. et al. Homeostatic response to sleep restriction in adolescents. Sleep 44, zsab106 (2021).
Skorucak, J. et al. Response to chronic sleep restriction, extension, and subsequent total sleep deprivation in humans: adaptation or preserved sleep homeostasis? Sleep 41, zsy078 (2018).
Achermann, P. The two-process model of sleep regulation revisited. Aviat. Space Environ. Med. 75, A37–A43 (2004).
Carskadon, M. A., Acebo, C. & Jenni, O. G. Regulation of adolescent sleep: implications for behavior. Ann. NY Acad. Sci. 1021, 276–291 (2004).
Crowley, S., Acebo, C., Fallone, G. & Carskadon, M. Estimating dim light melatonin onset (DLMO) phase in adolescents using summer or school-year sleep/wake schedules. Sleep 29, 1632–1641 (2006).
Micic et al. Nocturnal melatonin profiles in patients with delayed sleep-wake phase disorder and control sleepers. J. Biol. Rhythms 30, 437–448 (2015).
Micic, G. et al. The endogenous circadian temperature period length (tau) in delayed sleep phase disorder compared to good sleepers. J. Sleep. Res. 22, 617–624 (2013).
Micic, G. et al. Circadian melatonin and temperature taus in delayed sleep–wake phase disorder and non-24-h sleep–wake rhythm disorder patients: an ultradian constant routine study. J. Biol. Rhythm. 31, 387–405 (2016).
Micic, G. et al. Circadian tau difference and rhythm associations in delayed sleep-wake phase disorder and sighted non-24-h sleep-wake rhythm disorder. Sleep 44, zsaa132 (2021). This study confirms that circadian rhythm is longer in those diagnosed with a circadian rhythm disorder.
Reppert, S. M. & Weaver, D. R. Molecular analysis of mammalian circadian rhythms. Ann. Rev. Physiol. 63, 647–676 (2001).
Burgess, H. J. & Eastman, C. I. Human tau in an ultradian light–dark cycle. J. Biol. Rhythm. 23, 374–376 (2008).
Czeisler, C. A. et al. Stability, precision, and near-24-h period of the human circadian pacemaker. Science 284, 2177–2181 (1999).
Duffy, J. F. & Wright, K. P. Jr Entrainment of the human circadian system by light. J. Biol. Rhythms 20, 326–338 (2005).
Zeitzer, J. M., Dijk, D. J., Kronauer, R. E., Brown, E. N. & Czeisler, C. A. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J. Physiol. 526, 695–702 (2000).
Crowley, S., Wolfson, A., Tarokh, L. & Carskadon, M. An update on adolescent sleep: new evidence informing the perfect storm model. J. Adolesc. 67, 55–65 (2018). This is a review of the biological and psychosocial factors that influence an adolescent’s sleep.
Hagenauer, M. H., Perryman, J. I., Lee, T. M. & Carskadon, M. A. Adolescent changes in the homeostatic and circadian regulation of sleep. Dev. Neurosci. 31, 276–284 (2009).
Crowley, S. J. & Carskadon, M. A. Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol. Int. 27, 1469–1492 (2010).
Dawson, D., Lack, L. & Morris, M. Phase resetting of the human circadian pacemaker with use of a single pulse of bright light. Chronobiol. Int. 10, 94–102 (1993).
Strogatz, S. H., Kronauer, E. R. & Czeisler, C. Circadian pacemaker interferes with sleep onset at specific times each day: role in insomnia. Am. J. Physiol. 253, R172–R178 (1987).
Saxvig, I. et al. Objective measures of sleep and dim light melatonin onset in adolescents and young adults with delayed sleep phase disorder compared to healthy controls. J. Sleep Res. 22, 365–372 (2013).
Owens, J. A., Belon, K. & Moss, P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch. Pediatr. Adolesc. Med. 164, 608–614 (2010).
Bei, B. et al. Actigraphy-assessed sleep during school and vacation periods: a naturalistic study of restricted and extended sleep opportunities in adolescents. J. Sleep Res. 23, 107–117 (2014).
Short, M. A. & Chee, M. W. L. Adolescent sleep restriction effects on cognition and mood. Prog. Brain Res. 246, 55–71 (2019).
Taylor, A., Wright, H. R. & Lack, L. C. Sleeping-in on the weekend delays circadian phase and increases sleepiness the following week. Sleep Biol. Rhythms 6, 172–179 (2008).
American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic and Coding Manual 3rd edn (American Academy of Sleep Medicine, 2014).
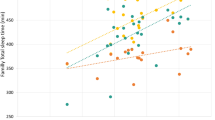
Raniti, M. B. et al. Sleep duration and sleep quality: associations with depressive symptoms across adolescence. Behav. Sleep Med. 15, 198–215 (2017).
Fredriksen, K., Rhodes, J., Reddy, R. & Way, N. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Dev. 75, 84–95 (2004).
Baum, K. T. et al. Sleep restriction worsens mood and emotion regulation in adolescents. J. Child. Psychol. Psychiat. 55, 180–190 (2014).
Vriend, J. et al. Manipulating sleep duration alters emotional functioning and cognitive performance in children. J. Pediatr. Psychol. 38, 1058–1069 (2013).
Talbot, L. S., McGlinchey, E. L., Kaplan, K. A., Dahl, R. E. & Harvey, A. G. Sleep deprivation in adolescents and adults: changes in affect. Emotion 10, 831–841 (2010).
Short, M. A., Booth, S. A., Omar, O., Ostlundh, L. & Arora, T. The relationship between sleep duration and mood in adolescents: a systematic review and meta-analysis. Sleep. Med. Rev. 52, 101311 (2020). This is an updated quantification of the link between mood states and sleep quantity.
McLaughlin, K. A., Hatzenbuehler, M. L., Mennin, D. S. & Nolen-Hoeksema, S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav. Res. Ther. 49, 544–554 (2011).
Prehn-Kristensen, A. et al. Sleep in children enhances preferentially emotional declarative but not procedural memories. J. Exp. Child. Psychol. 104, 132–139 (2009).
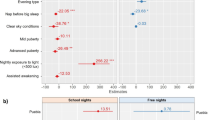
Bauducco, S., Richardson, C. & Gradisar, M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 34, 77–83 (2020).
Nguyen, C., Murray, G., Anderson, S., Filipowicz, A. & Ingram, K. K. In vivo molecular chronotyping, circadian misalignment, and high rates of depression in young adults. J. Affect. Disord. 250, 425–431 (2019).
Dolsen, M. R. & Harvey, A. G. Dim light melatonin onset and affect in adolescents with an evening circadian preference. J. Adolesc. Health 62, 94–99 (2018).
Chiu, W.-H., Yang, H. J. & Kuo, P.-H. Chronotype preference matters for depression in youth. Chronobiol. Int. 34, 933–941 (2017).
Merikanto, I. et al. Eveningness as a risk for behavioral problems in late adolescence. Chronobiol. Int. 34, 225–234 (2017).
Koo, D. L. et al. Association between morningness–eveningness, sleep duration, weekend catch‐up sleep and depression among Korean high‐school students. J. Sleep Res. 30, e13063 (2021).
Haraden, D. A., Mullin, B. C. & Hankin, B. L. The relationship between depression and chronotype: a longitudinal assessment during childhood and adolescence. Depress. Anxiety 34, 967–976 (2017).
Van den Berg, J. F., Kivelä, L. & Antypa, N. Chronotype and depressive symptoms in students: an investigation of possible mechanisms. Chronobiol. Int. 35, 1248–1261 (2018).
Vetter, C. et al. Prospective study of chronotype and incident depression among middle-and older-aged women in the Nurses’ Health Study II. J. Psychiatr. Res. 103, 156–160 (2018).
Haraden, D. A., Mullin, B. C. & Hankin, B. L. Internalizing symptoms and chronotype in youth: a longitudinal assessment of anxiety, depression and tripartite model. Psychiat. Res. 272, 797–805 (2019).
McClung, C. A. How might circadian rhythms control mood? Let me count the ways. Biol. Psychiat. 74, 242–249 (2013).
Gradisar, M. et al. Randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep 34, 1671–1680 (2011).
Biddle, S. J., Ciaccioni, S., Thomas, G. & Vergeer, I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol. Sport Exerc. 42, 146–155 (2019).
Heinrich, L. M. & Gullone, E. The clinical significance of loneliness: a literature review. Clin. Psychol. Rev. 26, 695–718 (2006).
Stephenson, K. M., Schroder, C. M., Bertschy, G. & Bourgin, P. Complex interaction of circadian and non-circadian effects of light on mood: shedding new light on an old story. Sleep Med. Rev. 16, 445–454 (2012).
Warner, S., Murray, G. & Meyer, D. Holiday and school-term sleep patterns of Australian adolescents. J. Adolesc. 31, 595–608 (2008).
Antypa, N. et al. Associations between chronotypes and psychological vulnerability factors of depression. Chronobiol. Int. 34, 1125–1135 (2017).
Watkins, E. R. & Roberts, H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behav. Res. Ther. 127, 103573 (2020). This study shows that daily changes in ruminative thinking are weighted towards more rumination at both ends of the day.
Takano, K. & Tanno, Y. Diurnal variation in rumination. Emotion 11, 1046 (2011).
Hühne, A., Welsh, D. K. & Landgraf, D. Prospects for circadian treatment of mood disorders. Ann. Med. 50, 637–654 (2018).
Hickie, I. B. & Rogers, N. L. Novel melatonin-based therapies: potential advances in the treatment of major depression. Lancet 378, 621–631 (2011).
Short, M. A., Gradisar, M., Gill, J. & Camfferman, D. Identifying adolescent sleep problems. PLoS ONE 8, e75031 (2013). This study finds discrepancies between adolescent perceptions of a sleep problem and researcher classifications.
Hysing, M., Haugland, S., Stormark, K. M., Bøe, T. & Siversten, B. Sleep and school attendance in adolescence: results from a large population-based study. Scand. J. Pub. Health 43, 2–9 (2014).
Lichstein, K. L., Durrence, H. H., Taylor, D. J., Bush, A. J. & Riedel, B. W. Quantitative criteria for insomnia. Behav. Res. Ther. 41, 427–445 (2003).
Orchard, F., Gregory, A. M., Gradisar, M. & Reynolds, S. Self-reported sleep patterns and quality amongst adolescents: cross-sectional and prospective associations with aniety and depression. J. Child. Psychol. Psychiat. 61, 1126–1137 (2020).
Jakobsson, M., Sundin, K., Högberg, K. & Josefsson, K. “I want to sleep but I can’t”: adolescents’ lived experience of sleeping difficulties. J. Sch. Nurs. https://doi.org/10.1177/1059840520966011 (2020). This paper provides rich qualitative information about adolescents’ experiences of sleeplessness.
Espie, C. A. Understanding insomnia through cognitive modelling. Sleep Med. 8, S3–S8 (2007).
Harvey, A. G. A cognitive model of insomnia. Behav. Res. Ther. 40, 869–893 (2002).
Lundh, L. G. & Broman, J. E. Insomnia as an interaction between sleep-interfering and sleep-interpreting processes. J. Psychosom. Res. 49, 299–310 (2000).
Hiller, R. M., Lovato, N., Gradisar, M., Oliver, M. & Slater, A. Trying to fall asleep while catastrophising: what sleep-disordered adolescents think and feel. Sleep Med. 15, 96–103 (2014).
Wicklow, A. & Espie, C. A. Intrusive thoughts and their relationship to actigraphic measurement of sleep: towards a cognitive model of insomnia. Behav. Res. Ther. 38, 679–693 (2000). This is the first categorization of unhelpful themes of cognition for those experiencing insomnia.
Saxvig, I. et al. Circadian typology and implications for adolescent sleep health: results from a large, cross-sectional, school-based study. Sleep Med. 83, 63–70 (2021).
Orchard, F. & Reynolds, S. “It was all my fault”: negative interpretation bias in depressed adolescents. J. Abnorm. Child Psychol. 44, 991–998 (2016).
Orchard, F. & Reynolds, S. The combined influence of cognitions in adolescent depression: biases of interpretation, self-evaluation, and memory. Br. J. Clin. Psychol. 57, 420–435 (2018).
Huang, C. et al. The roles of repetitive negative thinking and perfectionism in explaining the relationship between sleep onset difficulties and depressed mood in adolescents. Sleep Health 6, 166–171 (2020).
Crowley, S. & Eastman, C. Human adolescent phase response curves to bright white light. J. Biol. Rhythm. 32, 334–344 (2017).
Auger, R. R. et al. Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep–wake disorders: advanced sleep–wake phase disorder (ASWPD), delayed sleep–wake phase disorder (DSWPD), non-24-h sleep–wake rhythm disorder (N24SWD), and irregular sleep–wake rhythm disorder (ISWRD). An update for 2015: an American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 11, 1199–1236 (2015). This is an expert consensus of the state of evidence for the treatment of circadian rhythm disorders.
Gradisar, M., Smits, M. & Bjorvatn, B. Assessment and treatment of delayed sleep phase disorder in adolescents: recent innovations and cautions. Sleep Med. Clin. 9, 199–210 (2014).
Richardson, C. & Gradisar, M. Depressed mood and repetitive negative thinking in delayed sleep–wake phase disorder: treatment effects and a comparison with good sleepers. J. Sleep. Res. 31, e13452 (2021).
Richardson, C. et al. A randomised controlled trial of bright light therapy and morning activity for adolescents and young adults with delayed sleep-wake phase disorder. Sleep. Med. 45, 114–123 (2018). This clinical trial demonstrates the efficacy of three weeks of bright light therapy aimed at improving adolescent sleep timing.
Saxvig, I. et al. A randomized controlled trial with bright light and melatonin for delayed sleep phase disorder: effects on subjective and objective sleep. Chronobiol. Int. 31, 72–86 (2014).
Danielsson, K., Jansson-Fröjmark, M., Broman, J.-E. & Markström, A. Cognitive behavioral therapy as an adjunct treatment to light therapy for delayed sleep phase disorder in young adults: a randomized controlled feasibility study. Behav. Sleep Med. 14, 212–232 (2016).
Richardson, C. et al. Cognitive performance in adolescents with delayed sleep-wake phase disorder: treatment effects and a comparison with good sleepers. J. Adolesc. 65, 72–84 (2018).
Wilhelmsen-Langeland, A. et al. A randomized controlled trial with bright light and melatonin for the treatment of delayed sleep phase disorder: effects on subjective and objective sleepiness and cognitive function. J. Biol. Rhythm. 28, 306–321 (2013).
Rosenthal, N. E. et al. Phase-shifting effects of bright morning light as treatment for delayed sleep phase syndrome. Sleep. 13, 354–361 (1990).
Wright, H., Lack, L. & Kennaway, D. Differential effects of light wavelength in phase advancing the melatonin rhythm. J. Pineal Res. 36, 140–144 (2004). This is the first study to demonstrate changes in circadian timing caused by different wavelengths of light.
Sharkey, K. M., Carskadon, M. A., Figueiro, M. G., Zhu, Y. & Rea, M. S. Effects of an advanced sleep schedule and morning short wavelength light exposure on circadian phase in young adults with late sleep schedules. Sleep. Med. 12, 685–692 (2011).
Kirschbaum-Lesch, I., Gest, S., Legenbauer, T. & Holtmann, M. Feasibility and efficacy of bright light therapy in depressed adolescent inpatients. Z. Kinder Jugendpsychiatr. Psychother. 46, a000603 (2018).
Danielsson, N., Harvey, A., MacDonald, S., Jansson-Fröjmark, M. & Linton, S. Sleep disturbance and depressive symptoms in adolescence: the role of catastrophic worry. J. Youth Adolesc. 42, 1223–1233 (2013).
Gest, S. et al. Chronotherapeutic treatments for depression in youth. Eur. Child. Adolesc. Psychiat. 25, 151–161 (2016).
Lam, R. et al. Efficacy of bright light treatment, fluoxetine, and the combination in patients with nonseasonal major depressive disorder: a randomized clinical trial. JAMA Psychiat. 73, 56–63 (2016).
Gordon, N. The therapeutics of melatonin: a paediatric perspective. Brain Dev. 22, 213–217 (2000).
Lewy, A. J., Wehr, T. A., Goodwin, F. K., Newsome, D. A. & Markey, S. P. Light suppresses melatonin secretion in humans. Science 210, 1267–1269 (1980).
Bruni, O. et al. Current role of melatonin in pediatric neurology: clinical recommendations. Eur. J. Paediatr. Neuro. 19, 122–133 (2015).
Kayumov, L., Brown, G., Jindal, R., Buttoo, K. & Shapiro, C. M. A randomized, double-blind, placebo-controlled crossover study of the effect of exogenous melatonin on delayed sleep phase syndrome. Psychosom. Med. 63, 40–48 (2001).
Carskadon, M., Wolfson, A., Acebo, C., Tzischinsky, O. & Seifer, R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep 21, 871–881 (1998).
Mindell, J. A. et al. Pharmacologic management of insomnia in children and adolescents: consensus statement. Pediatrics 117, e1223–e1232 (2006).
Mundey, K., Benloucif, S., Harsanyi, K., Dubocovich, M. L. & Zee, P. C. Phase-dependent treatment of delayed sleep phase syndrome with melatonin. Sleep 28, 1271–1278 (2005).
McDonagh, M. S., Holmes, R. & Hsu, F. Pharmacologic treatments for sleep disorders in children: a systematic review. J. Child. Neurol. 34, 237–247 (2019).
Owens, J. A., Rosen, C. L., Mindell, J. A. & Kirchner, H. L. Use of pharmacotherapy for insomnia in child psychiatry practice: a national survey. Sleep. Med. 11, 692–700 (2010).
Wei, S. et al. Efficacy and safety of melatonin for sleep onset insomnia in children and adolescents: a meta-analysis of randomized controlled trials. Sleep. Med. 68, 1–8 (2020). This study demonstrates the efficacy and safety of melatonin treatment for young people.
Rahman, S. A., Kayumov, L. & Shapiro, C. M. Antidepressant action of melatonin in the treatment of delayed sleep phase syndrome. Sleep Med. 11, 131–136 (2010).
Jan, J. E. & Freeman, R. D. Melatonin therapy for circadian rhythm sleep disorders in children with multiple disabilities: what have we learned in the last decade? Dev. Med. Child. Neurol. 46, 776–782 (2004).
van Geijlswijk, I. M., van der Heijden, K. B., Egberts, A. C. G., Korzilius, H. P. & Smits, M. G. Dose finding of melatonin for chronic idiopathic childhood sleep onset insomnia: an RCT. Psychopharmacology 212, 379–391 (2010).
Kennaway, D. J. Potential safety issues in the use of the hormone melatonin in paediatrics. J. Paediatr. Child Health 51, 584–589 (2015). This paper presents a critique of the scientific evidence supporting the use of melatonin as a treatment for paediatric sleep problems.
Bruni, O. et al. Paediatric use of melatonin (Author reply to DJ Kennaway). Eur. J. Paediatr. Neuro. 19, 491–493 (2015). This is a rebuttal to Kennaway (2015) from an expert group of paediatric sleep specialists.
Jamieson, D., Shan, Z., Lagopoulos, J. & Hermens, D. F. The role of adolescent sleep quality in the development of anxiety disorders: a neurobiologically-informed model. Sleep Med. Rev. 59, 101450 (2021).
Richardson, C. et al. Cognitive “insomnia” processes in delayed sleep-wake phase disorder: do they exist and are they responsive to chronobiological treatment? J. Consult. Clin. Psychol. 87, 16–32 (2019).
Blake, M., Latham, M., Blake, L. & Allen, N. Adolescent sleep intervention research: current state and future directions. Curr. Dir. Psychol. Sci. 28, 475–482 (2019).
Blake, M. J. et al. Systematic review and meta-analysis of adolescent cognitive–behavioral sleep interventions. Clin. Child. Fam. Psychol. Rev. 20, 227–249 (2017).
Harvey, A. G. & Tang, N. K. Y. Cognitive behaviour therapy for insomnia: can we rest yet? Sleep Med. Rev. 7, 237–262 (2003).
Bootzin, R. R. & Stevens, S. J. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin. Psychol. Rev. 25, 629–644 (2005).
Blake, M. J. et al. A cognitive-behavioral and mindfulness-based group sleep intervention improves behavior problems in at-risk adolescents by improving perceived sleep quality. Behav. Res. Ther. 99, 147–156 (2017).
Åslund, L., Arnberg, F., Kanstrup, M. & Lekander, M. Cognitive and behavioral interventions to improve sleep in school-age children and adolescents: a systematic review and meta-analysis. J. Clin. Sleep. Med. 14, 1937–1947 (2018). This paper quantifies the results from six randomized controlled trials of CBT for child and adolescent insomnia.
Chan, N. Y. et al. A prevention program for insomnia in at-risk adolescents: a randomized controlled study. Pediatrics 147, e2020006833 (2021).
Gee, B. et al. The effect of non-pharmacological sleep interventions on depression symptoms: a meta-analysis of randomised controlled trials. Sleep Med. Rev. 43, 118–128 (2019). This paper provides one of the clearest indications that non-pharmacological sleep treatments alone improve depression.
Åslund, L., Lekander, M., Wicksell, R. K., Henje, E. & Jernelöv, S. Cognitive-behavioral therapy for insomnia in adolescents with comorbid psychiatric disorders: a clinical pilot study. Clin. Child. Psychol. Psychiat. 25, 958–971 (2020).
De Bruin, U. J., Bögels, S. M., Oort, F. J. & Meijer, A. M. Efficacy of cognitive behavioral therapy for insomnia in adolescents: a randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep 38, 1913–1926 (2015). This is the first randomized controlled trial to evaluate CBT for adolescent insomnia, and compares face-to-face and internet delivery modes.
Gradisar, M. & Richardson, C. CBT-I cannot rest until the sleepy teen can. Sleep 38, 1841–1842 (2015).
Bartel, K., Huang, C., Maddock, B., Williamson, P. & Gradisar, M. Brief school-based interventions to assist adolescents’ sleep-onset latency: comparing mindfulness and constructive worry versus controls. J. Sleep Res. 27, e12668 (2018).
Lever, J. R., Murphy, A. P., Duffield, R. & Fullagar, H. H. K. A combined sleep hygiene and mindfulness intervention to improve sleep and well-being during high-performance youth tennis tournaments. Int. J. Sports Physiol. Perform. 16, 250–258 (2020).
Bartel, K., Scheeren, R. & Gradisar, M. Altering adolescents’ prebedtime phone use to achieve better sleep health. Health Commun. 34, 456–462 (2019). This study finds an increase in sleep quantity when adolescents reduce their evening smartphone use.
Bartel, K. & Gradisar, M. New directions in the link between technology use and sleep in young people. In Sleep Disorders in Children (eds Nevšimalová, S. & Bruni, O.) (Springer, 2017).
Cain, N. & Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep. Med. 11, 735–742 (2010).
Van den Bulck, J. The effects of media on sleep. Adolesc. Med. 21, 418–429 (2010).
Blake, M. J., Trinder, J. A. & Allen, N. B. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin. Psychol. Rev. 63, 25–40 (2018).
Bauducco, S. V., Flink, I. K., Boersma, K. & Linton, S. J. Preventing sleep deficit in adolescents: long-term effects of a quasi-experimental school-based intervention study. J. Sleep. Res. 29, e12940 (2020).
Richardson, C., Ree, M., Bucks, R. S. & Gradisar, M. Paediatric sleep literacy in Australian health professionals. Sleep. Med. 81, 327–335 (2021).
Crowe, K. & Spiro-Levitt, C. Sleep-related problems and pediatric anxiety disorders. Child. Adolesc. Psychiat. Clin. 30, 209–224 (2021).
Garber, J. & Weersing, V. R. Comorbidity of anxiety and depression in youth: implications for treatment and prevention. Clin. Psychol. 17, 293–306 (2010). (2010).
Higuchi, S., Motohashi, Y., Liu, Y. & Maeda, A. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. J. Sleep Res. 14, 267–273 (2005).
Ivarsson, M., Anderson, M., Åkerstedt, T. & Lindblad, F. The effect of violent and nonviolent video games on heart rate variability, sleep, and emotions in adolescents with different violent gaming habits. Psychosom. Med. 75, 390–396 (2013).
Weaver, E. et al. The effect of presleep video-game playing on adolescent sleep. J. Clin. Sleep. Med. 6, 184–189 (2010).
King, D. L. et al. The impact of prolonged violent video-gaming on adolescent sleep: an experimental study. J. Sleep. Res. 22, 137–143 (2013).
Van der Lely, S. et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J. Adolesc. Health 56, 113–119 (2015).
Heath et al. Does one hour of bright or short-wavelength filtered tablet screenlight have a meaningful effect on adolescents’ pre-bedtime alertness, sleep and daytime functioning? Chronobiol. Int. 31, 496–505 (2014). This is the first controlled laboratory study to demonstrate that the effect of blue light emissions from screens on sleep is minimal.
Duraccio, K. M., Zaugg, K. K., Blackburn, R. C. & Jensen, C. D. Does iPhone night shift mitigate negative effects of smartphone use on sleep outcomes in emerging adults? Sleep Health 7, 478–484 (2021). This field study demonstrates that the effect of blue light emissions on sleep are minimal.
Knufinke, M., Fittkau-Kock, L., Møst, E. I. S., Kompier, M. A. J. & Nieuwenhuys, A. Restricting short-wavelength light in the evening to improve sleep in recreational athletes — a pilot study. Eur. J. Sport. Sci. 19, 728–735 (2018).
Smith et al. Mechanisms influencing older adolescents’ bedtimes during videogaming: the roles of game difficulty and flow. Sleep Med. 39, 70–76 (2017).
Exelmans, L. & Van Den Bulck, J. “Glued to the tube”: the interplay between self-control, evening television viewing, and bedtime procrastination. Commun. Res. 48, 594–616 (2017).
Reynolds, C. M. et al. Adolescents who perceive fewer consequences of risk‐taking choose to switch off games later at night. Acta Paediatr. 104, e222–e227 (2015).
Bartel, K., Gradisar, M. & Williamson, P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep. Med. Rev. 21, 72–85 (2015). This paper quantifies all factors known to help and harm adolescent sleep.
Tavernier, R. & Willoughby, T. Sleep problems: predictor or outcome of media use among emerging adults at university? J. Sleep. Res. 23, 389–396 (2014).
Richardson, C. et al. A longitudinal investigation of sleep and technology use in early adolescence: does parental control of technology use protect adolescent sleep? Sleep Med. 84, 368–379 (2021). This longitudinal study suggests that sleep problems might predict technology use.
Eggermont, S. & van den Bulck, J. Nodding off or switching off? The use of popular media as a sleep aid in secondary-school children. J. Paediatr. Child Health 42, 428–433 (2006).
Jansson-Fröjmark, M. & Norell-Clarke, A. The cognitive treatment components and therapies of cognitive behavioral therapy for insomnia: a systematic review. Sleep Med. Rev. 42, 19–36 (2018).
Buda, G., Lukoševičiūtė, J. & Šmigelskas, K. Possible effects of social media use on adolescent health behaviors and perceptions. Psychol. Rep. https://doi.org/10.1177/0033294120922481 (2020).
Acknowledgements
The authors thank the hundreds of families who have participated in the authors’ and colleagues research, sharing their knowledge so that we could provide the reader with this Review.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
M.G. is the CEO of WINK Sleep Pty Ltd, and as such receives income from the sale of online courses for treating adolescent sleep problems. All other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Psychology thanks Melynda Casement and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Polysomnography
-
A comprehensive test used to diagnose sleep disorders that includes measures of brain waves, blood oxygen level, heart rate, breathing and eye and leg movements.
Rights and permissions
About this article
Cite this article
Gradisar, M., Kahn, M., Micic, G. et al. Sleep’s role in the development and resolution of adolescent depression. Nat Rev Psychol 1, 512–523 (2022). https://doi.org/10.1038/s44159-022-00074-8
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s44159-022-00074-8
This article is cited by
-
The association of chronotype on depression in adolescents: the mediating role of sensation seeking and sleep quality
BMC Psychiatry (2025)
-
Symptom network between problematic smartphone use and poor sleep quality in adolescents with depression
BMC Psychiatry (2025)
-
U-shaped association between social media usage frequency and suggestibility by internet health information in Chinese online population with pre-diabetes and diabetes: a cross-sectional study
BMC Public Health (2025)
-
Diagnosis of adolescent depression with sleep disorder based on network topological attributes and functional connectivity
BMC Psychiatry (2025)
-
Sleep trajectories and frequency of non-suicidal self-injury in adolescents: a person-oriented perspective over two years
Scientific Reports (2025)