Abstract
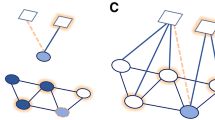
Self-harm has proven social contagion effects among young people. However, a comprehensive understanding of the complex dynamics that contribute to self-harm contagion in adolescents is lacking. In this Review, we synthesize evidence regarding the social contagion of self-harm in young people using a social ecological approach. At the individual level, psychological and neurobiological vulnerabilities increase young people’s susceptibility to social contagion. At the interpersonal level, social contagion of self-harm occurs through peer interactions and social media connections, as well as through family ties including parental, sibling and grandparental relationships. At the community level, social contagion is evident in high-risk clusters of young people in institutional settings (schools, universities, psychiatric hospitals and justice-involved youth institutes), on social media and in digital spaces, and in neighbourhoods, where socioeconomic disadvantage is a key structural constraint that amplifies self-harm contagion. At the societal level, media-regulation challenges, global pandemics and political context exacerbate the social contagion of self-harm by intensifying pre-existing risk factors across individual, interpersonal and community levels. We address these multilevel factors to bridge psychological and public health perspectives of social contagion dynamics and describe prevention and intervention efforts that might offer scalable, evidence-based solutions for mitigating self-harm among youth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bilello, D., Townsend, E., Broome, M. R., Armstrong, G. & Heyes, S. B. Friendships and peer relationships and self-harm ideation and behaviour among young people: a systematic review and narrative synthesis. Lancet Psychiatry 11, 633–657 (2024). This review provides quantitative research evidence of self-harm contagion through peer interactions among young people.
Geoffroy, M.-C. et al. Prevalence of suicidal ideation and self-harm behaviours in children aged 12 years and younger: a systematic review and meta-analysis. Lancet Psychiatry 9, 703–714 (2022).
Glenn, C. R. et al. Annual research review: a meta-analytic review of worldwide suicide rates in adolescents. J. Child Psychol. Psychiatry 61, 294–308 (2020).
Hawton, K. et al. Clustering of suicides in children and adolescents. Lancet Child Adolesc. Health 4, 58–67 (2020). This review explores suicide clusters in children and adolescents and discusses potential underlying mechanisms.
Jarvi, S., Jackson, B., Swenson, L. & Crawford, H. The impact of social contagion on non-suicidal self-injury: a review of the literature. Arch. Suicide Res. 17, 1–19 (2013). This article synthesizes empirical evidence on the prevalence, risk factors and underlying mechanisms by which social contagion influences the transmission of non-suicidal self-injury.
Benson, R. et al. Quantitative methods to detect suicide and self-harm clusters: a systematic review. Int. J. Environ. Res. Publ. Health 19, 5313 (2022).
Fuhrmann, D., Knoll, L. J. & Blakemore, S.-J. Adolescence as a sensitive period of brain development. Trends Cogn. Sci. 19, 558–566 (2015).
Christie, D. & Viner, R. Adolescent development. BMJ 330, 301–304 (2005).
Steinberg, L. & Morris, A. S. Adolescent development. Annu. Rev. Psychol. 52, 83–110 (2001).
Corzine, A. & Harrison, V. Social contagion, from suicide to online challenges to eating disorders: current research and harm mitigation strategies for youth online. J. Online Trust Saf. https://doi.org/10.54501/jots.v2i1.145 (2023).
Walling, M. A. Suicide contagion. Curr. Trauma. Rep. 7, 103–114 (2021).
Golden, S. D., McLeroy, K. R., Green, L. W., Earp, J. A. L. & Lieberman, L. D. Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health Educ. Behav. 42, 8S–14S (2015).
Richard, L., Gauvin, L. & Raine, K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu. Rev. Publ. Health 32, 307–326 (2011).
Matsick, J. L., Sullivan, J. T., Todd, E., Kruk, M. & Cook, J. E. A social ecological approach to belonging in LGBTQ+ people. Nat. Rev. Psychol. 3, 181–197 (2024).
Stokols, D. Translating social ecological theory into guidelines for community health promotion. Am. J. Health Prom. 10, 282–298 (1996).
Stokols, D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am. Psychol. 47, 6–22 (1992).
Lewis, S. P. & Hasking, P. A. Understanding Self-Injury: A Person-Centered Approach (Oxford Univ. Press, 2023).
Cheng, Q., Li, H., Silenzio, V. & Caine, E. D. Suicide contagion: a systematic review of definitions and research utility. PLoS ONE 9, e108724 (2014).
Nock, M. K. Why do people hurt themselves?: new insights into the nature and functions of self-injury. Curr. Dir. Psychol. Sci. 18, 78–83 (2009).
Rogier, G. et al. The multifaceted role of emotion regulation in suicidality: systematic reviews and meta-analytic evidence. Psychol. Bull. 150, 45–81 (2024).
McEvoy, D. et al. Risk and protective factors for self-harm in adolescents and young adults: an umbrella review of systematic reviews. J. Psychiat. Res. 168, 353–380 (2023).
Wolff, J. C. et al. Emotion dysregulation and non-suicidal self-injury: a systematic review and meta-analysis. Eur. Psychiatry 59, 25–36 (2019).
Kiekens, G. et al. Fluctuations in affective states and self-efficacy to resist non-suicidal self-injury as real-time predictors of non-suicidal self-injurious thoughts and behaviors. Front. Psychiatry 11, 214 (2020).
Wen, X. et al. The transition trajectories of self-injurious thoughts and behaviours among children from a biopsychosocial perspective. Nat. Ment. Health 1, 782–791 (2023). This is a study of intergenerational transmission of suicidal behaviours across grandparents, parents and children and related psychological and neurobiological mechanisms.
Wen, X. et al. Brain structural and functional signatures of multi-generational family history of suicidal behaviors in preadolescent children. Mol. Psychiatry 29, 484–495 (2023).
Owens, D., Horrocks, J. & House, A. Fatal and non-fatal repetition of self-harm: systematic review. Br. J. Psychiatry 181, 193–199 (2002).
Schwartz-Mette, R. A. & Lawrence, H. R. Peer socialization of non-suicidal self-injury in adolescents’ close friendships. J. Abnorm. Child Psychol. 47, 1851–1862 (2019).
Zelkowitz, R. L., Porter, A. C., Heiman, E. R. & Cole, D. A. Social exposure and emotion dysregulation: main effects in relation to nonsuicidal self-injury. J. Adolesc. 60, 94–103 (2017).
Mueller, A. S. & Abrutyn, S. Suicidal disclosures among friends: using social network data to understand suicide contagion. J. Health Soc. Behav. 56, 131–148 (2015).
Bandura, A. & Walters, R. H. Social Learning Theory Vol. 1 (Prentice-Hall, 1977).
Hasking, P. & Rose, A. A preliminary application of social cognitive theory to nonsuicidal self-injury. J. Youth Adolesc. 45, 1560–1574 (2016).
Bandura, A. & National Institute of Mental Health Social Foundations of Thought and Action: A Social Cognitive Theory (Prentice-Hall, 1986).
Zimmerman, G. M., Rees, C., Posick, C. & Zimmerman, L. A. The power of (mis)perception: rethinking suicide contagion in youth friendship networks. Soc. Sci. Med. 157, 31–38 (2016).
Ortin-Peralta, A. et al. Negative and positive urgency as pathways in the intergenerational transmission of suicide risk in childhood. Front. Psychiatry 15, 1417991 (2024).
Brent, D. A. et al. Familial pathways to early-onset suicide attempt: a 5.6-year prospective study. JAMA Psychiatry 72, 160–168 (2015).
Brent, D. A. & Melhem, N. Familial transmission of suicidal behavior. Psychiat. Clin. North. Am. 31, 157–177 (2008).
Brent, D. A. et al. Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. Am. J. Psychiatry 160, 1486–1493 (2003).
Ciranka, S. & van den Bos, W. Adolescent risk-taking in the context of exploration and social influence. Dev. Rev. 61, 100979 (2021).
Kilford, E. J., Garrett, E. & Blakemore, S.-J. The development of social cognition in adolescence: an integrated perspective. Neurosci. Biobehav. Rev. 70, 106–120 (2016).
Crone, E. A. & Dahl, R. E. Understanding adolescence as a period of social–affective engagement and goal flexibility. Nat. Rev. Neurosci. 13, 636–650 (2012).
Schriber, R. A. & Guyer, A. E. Adolescent neurobiological susceptibility to social context. Dev. Cogn. Neurosci. 19, 1–18 (2016).
Pollak, O. H. et al. Neural reactivity to social punishment predicts future engagement in nonsuicidal self-injury among peer-rejected adolescents. Biol. Psychiatry 94, 40–49 (2023).
Perini, I. et al. Brain-based classification of negative social bias in adolescents with nonsuicidal self-injury: findings from simulated online social interaction. eClinicalMedicine 13, 81–90 (2019).
Cummings, L. R., Mattfeld, A. T., Pettit, J. W. & McMakin, D. L. Viewing nonsuicidal self-injury in adolescence through a developmental neuroscience lens: the impact of neural sensitivity to socioaffective pain and reward. Clin. Psychol. Sci. 9, 767–790 (2021). This study proposes that an imbalance between heightened emotional salience and lagging regulatory capacity might be a neurobiological susceptibility factor for self-harm contagion in adolescents.
Eisenberger, N. I. & Lieberman, M. D. in The Social Outcast: Ostracism, Social Exclusion, Rejection, and Bullying (eds Williams, K. D. et al.) 109–127 (Psychology Press, 2005).
Zilverstand, A., Parvaz, M. A. & Goldstein, R. Z. Neuroimaging cognitive reappraisal in clinical populations to define neural targets for enhancing emotion regulation. A systematic review. NeuroImage 151, 105–116 (2017).
Nelson, E. E., Jarcho, J. M. & Guyer, A. E. Social re-orientation and brain development: an expanded and updated view. Dev. Cogn. Neurosci. 17, 118–127 (2016).
Blakemore, S.-J. & Mills, K. L. Is adolescence a sensitive period for sociocultural processing? Annu. Rev. Psychol. 65, 187–207 (2014).
Dai, J., Kwon, S.-J., Prinstein, M. J., Telzer, E. H. & Lindquist, K. A. Neural similarity in nucleus accumbens during decision-making for the self and a best friend: links to adolescents’ self-reported susceptibility to peer influence and risk taking. Hum. Brain Mapp. 44, 3972–3985 (2023).
Liu, H.-C., Huang, Y.-H., Tjung, J.-J., Sun, F.-J. & Liu, S.-I. Recent exposure to others’ confided suicidal thoughts and risk of self-harm and suicidality among adolescents. Curr. Psychol. 42, 19786–19794 (2023).
Baller, R. D. & Richardson, K. K. The “dark side” of the strength of weak ties: the diffusion of suicidal thoughts. J. Health Soc. Behav. 50, 261–276 (2009).
Wyman, P. A. et al. Peer–adult network structure and suicide attempts in 38 high schools: implications for network-informed suicide prevention. J. Child. Psychol. Psychiatry 60, 1065–1075 (2019).
Granovetter, M. S. The strength of weak ties. Am. J. Sociol. 78, 1360–1380 (1973).
Granovetter, M. The strength of weak ties: a network theory revisited. Sociol. Theory 1, 201–233 (1983).
Crudgington, H., Wilson, E., Copeland, M., Morgan, C. & Knowles, G. Peer-friendship networks and self-injurious thoughts and behaviors in adolescence: a systematic review of sociometric school-based studies that use social network analysis. Adolesc. Res. Rev. 8, 21–43 (2023).
You, J., Lin, M. P., Fu, K. & Leung, F. The best friend and friendship group influence on adolescent nonsuicidal self-injury. J. Abnorm. Child Psychol. 41, 993–1004 (2013).
Copeland, M., Siennick, S. E., Feinberg, M. E., Moody, J. & Ragan, D. T. Social ties cut both ways: self-harm and adolescent peer networks. J. Youth Adolesc. 48, 1506–1518 (2019).
You, J., Zheng, C., Lin, M.-P. & Leung, F. Peer group impulsivity moderated the individual-level relationship between depressive symptoms and adolescent nonsuicidal self-injury. J. Adolesc. 47, 90–99 (2016).
Giletta, M., Burk, W. J., Scholte, R. H. J., Engels, R. C. M. E. & Prinstein, M. J. Direct and indirect peer socialization of adolescent nonsuicidal self-injury. J. Res. Adolesc. 23, 450–463 (2013).
Prinstein, M. J. et al. Peer influence and nonsuicidal self injury: longitudinal results in community and clinically-referred adolescent samples. J. Abnorm. Child Psychol. 38, 669–682 (2010).
Gould, M. S. et al. Exposure to suicide in high schools: impact on serious suicidal ideation/behavior, depression, maladaptive coping strategies, and attitudes toward help-seeking. Int. J. Environ. Res. Publ. Health 15, 455 (2018).
Brent, D. A., Moritz, G., Bridge, J., Perper, J. & Canobbio, R. Long-term impact of exposure to suicide: a three-year controlled follow-up. J. Am. Acad. Child Adolesc. Psychiatry 35, 646–653 (1996).
Ortiz, P. & Khin Khin, E. Traditional and new media’s influence on suicidal behavior and contagion. Behav. Sci. Law 36, 245–256 (2018).
Nesi, J. et al. Social media use and self-injurious thoughts and behaviors: a systematic review and meta-analysis. Clin. Psychol. Rev. 87, 102038 (2021). This systematic review and meta-analysis synthesizes evidence on the dose–response relationship between active versus passive social media exposure to self-harm content and subsequent risks of self-injurious thoughts and behaviors.
Haltigan, J. D., Pringsheim, T. M. & Rajkumar, G. Social media as an incubator of personality and behavioral psychopathology: symptom and disorder authenticity or psychosomatic social contagion? Compr. Psychiatry 121, 152362 (2023).
Susi, K., Glover-Ford, F., Stewart, A., Knowles Bevis, R. & Hawton, K. Research review: viewing self-harm images on the internet and social media platforms: systematic review of the impact and associated psychological mechanisms. J. Child Psychol. Psychiatry 64, 1115–1139 (2023).
Lavis, A. & Winter, R. Online harms or benefits? An ethnographic analysis of the positives and negatives of peer-support around self-harm on social media. J. Child Psychol. Psychiatry 61, 842–854 (2020).
Calvo, S., Carrasco, J. P., Conde-Pumpido, C., Esteve, J. & Aguilar, E. J. Does suicide contagion (Werther effect) take place in response to social media? A systematic review. Span. J. Psychiatry Ment. Health https://doi.org/10.1016/j.sjpmh.2024.05.003 (2024).
Jacob, N., Evans, R. & Scourfield, J. The influence of online images on self-harm: a qualitative study of young people aged 16–24. J. Adolesc. 60, 140–147 (2017).
Baker, T. G. & Lewis, S. P. Responses to online photographs of non-suicidal self-injury: a thematic analysis. Arch. Suicide Res. 17, 223–235 (2013).
Arendt, F., Scherr, S. & Romer, D. Effects of exposure to self-harm on social media: evidence from a two-wave panel study among young adults. N. Media Soc. 21, 2422–2442 (2019).
Cha, C. B. et al. Examining potential iatrogenic effects of viewing suicide and self-injury stimuli. Psychol. Assess. 28, 1510–1515 (2016).
Brown, R. C. et al. #cutting: non-suicidal self-injury (NSSI) on Instagram. Psychol. Med. 48, 337–346 (2018).
Brown, R. C., Fischer, T., Goldwich, D. A. & Plener, P. L. “I just finally wanted to belong somewhere” — qualitative analysis of experiences with posting pictures of self-injury on instagram. Front. Psychiatry 11, 274 (2020).
Hetrick, S. E. et al. Understanding the needs of young people who engage in self-harm: a qualitative investigation. Front. Psychol. 10, 2916 (2020).
Seko, Y., Kidd, S. A., Wiljer, D. & McKenzie, K. J. On the creative edge: exploring motivations for creating non-suicidal self-injury content online. Qual. Health Res. 25, 1334–1346 (2015).
Sternudd, H. T. Photographs of self-injury: production and reception in a group of self-injurers. J. Youth Stud. 15, 421–436 (2012).
Bakian, A. V. et al. A population-wide analysis of the familial risk of suicide in Utah, USA. Psychol. Med. 53, 1448–1457 (2021).
Bowen, M. The use of family theory in clinical practice. Compr. Psychiatry 7, 345–374 (1966).
Ortin-Peralta, A. et al. Parental suicide attempts and offspring’s risk of attempting or dying by suicide: does the timing of a parental suicide attempt matter? Psychol. Med. 53, 977–986 (2023).
Calderaro, M. et al. Offspring’s risk for suicidal behaviour in relation to parental death by suicide: systematic review and meta-analysis and a model for familial transmission of suicide. Br. J. Psychiatry 220, 121–129 (2022). This systematic review and meta-analysis synthesizes evidence on the familial transmission of suicidal behaviour following parental suicide and discusses possible mechanisms.
Perez, N. M., Jennings, W. G., Piquero, A. R. & Baglivio, M. T. Adverse childhood experiences and suicide attempts: the mediating influence of personality development and problem behaviors. J. Youth Adolesc. 45, 1527–1545 (2016).
Geulayov, G., Metcalfe, C., Heron, J., Kidger, J. & Gunnell, D. Parental suicide attempt and offspring self-harm and suicidal thoughts: results from the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort. J. Am. Acad. Child Adolesc. Psychiatry 53, 509–517.e2 (2014).
Branje, S. et al. Intergenerational transmission: theoretical and methodological issues and an introduction to four Dutch cohorts. Dev. Cogn. Neurosci. 45, 100835 (2020).
Ranning, A., Madsen, T., Hawton, K., Nordentoft, M. & Erlangsen, A. Transgenerational concordance in parent-to-child transmission of suicidal behaviour: a retrospective, nationwide, register-based cohort study of 4,419,642 individuals in Denmark. Lancet Psychiatry 9, 363–374 (2022).
Ranning, A. et al. Intergenerational transmission of suicide attempt in a cohort of 4.4 million children. Psychol. Med. 52, 1–8 (2021).
Edwards, A. C. et al. Geographic proximity is associated with transmission of suicidal behaviour among siblings. Acta Psychiat. Scand. 140, 30–38 (2019).
Morris, A. S., Silk, J. S., Steinberg, L., Myers, S. S. & Robinson, L. R. The role of the family context in the development of emotion regulation. Soc. Dev. 16, 361–388 (2007).
Eisenberg, N., Cumberland, A. & Spinrad, T. L. Parental socialization of emotion. Psychol. Inq. 9, 241–273 (1998).
Voracek, M. & Loibl, L. M. Genetics of suicide: a systematic review of twin studies. Wien. Klin. Wochenschr. 119, 463–475 (2007).
Baldessarini, R. J. & Hennen, J. Genetics of suicide: an overview. Harv. Rev. Psychiatry 12, 1–13 (2004).
Docherty, A. R. et al. GWAS meta-analysis of suicide attempt: identification of 12 genome-wide significant loci and implication of genetic risks for specific health factors. Am. J. Psychiatry 180, 723–738 (2023).
Docherty, A. R., Adkins, D. E., Darlington, T. M., Klein, M. & McIntosh, A. Genome-wide association study of suicide death and polygenic prediction of clinical antecedents. Am. J. Psychiatry 177, 917–927 (2020).
O’Reilly, L. M. et al. The intergenerational transmission of suicidal behavior: an offspring of siblings study. Transl. Psychiatry 10, 173 (2020). This study quantifies the relative contributions of genetic and shared environmental factors to the parent–offspring transmission of suicidal behavior.
Buckholdt, K. E., Parra, G. R. & Jobe-Shields, L. Emotion regulation as a mediator of the relation between emotion socialization and deliberate self-harm. Am. J. Orthopsychiatry 79, 482–490 (2009).
Aldridge, J. M. & McChesney, K. The relationships between school climate and adolescent mental health and wellbeing: a systematic literature review. Int. J. Educ. Res. 88, 121–145 (2018).
Mueller, A. S., Pearson, J., Muller, C., Frank, K. & Turner, A. Sizing up peers: adolescent girls’ weight control and social comparison in the school context. J. Health Soc. Behav. 51, 64–78 (2010).
Cotterell, J. Social Networks in Youth and Adolescence (Routledge, 2013).
MacKenzie, D. W. Applying the Anderson–Darling test to suicide clusters: evidence of contagion at U.S. universities? Crisis 34, 434–437 (2013).
Brent, D. A. et al. An outbreak of suicide and suicidal behavior in a high school. J. Am. Acad. Child Adolesc. Psychiatry 28, 918–924 (1989).
Pérez-Izaguirre, E. Can transgression define identity in educational settings? A Basque-based framework for identity-in-interaction. Front. Psychol. 10, 1741 (2019).
Muniz, J. P. C., Finger, K. B., Davi, W. S., Araújo, K. S. S. D. & Côrtes, M. A. Mental vulnerability and suicide by contagion during the academic experience. Rev. Med. 100, 351–357 (2021).
Qu, D. et al. Non-suicidal self-injury in Chinese population: a scoping review of prevalence, method, risk factors and preventive interventions. Lancet Reg. Health West. Pacif. 37, 100794 (2023).
Uddin, R., Burton, N. W., Maple, M., Khan, S. R. & Khan, A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child Adolesc. Health 3, 223–233 (2019).
Russell, K. et al. Sleep problem, suicide and self-harm in university students: a systematic review. Sleep Med. Rev. 44, 58–69 (2019).
Sivertsen, B. et al. Suicide attempts and non-suicidal self-harm among university students: prevalence study. BJPsych Open. 5, e26 (2019).
Okechukwu, F. O. et al. Academic stress and suicidal ideation: moderating roles of coping style and resilience. BMC Psychiatry 22, 546 (2022).
Copeland, M. et al. When friends bring you down: peer stress proliferation and suicidality. Arch. Suicide Res. 25, 672–689 (2021).
Reynolds, A. D. & Crea, T. M. Peer influence processes for youth delinquency and depression. J. Adolesc. 43, 83–95 (2015).
Mueller, A. S. & Abrutyn, S. Suicidal disclosures among friends. J. Health Soc. Behav. https://doi.org/10.1177/0022146514568793 (2015).
Abrutyn, S., Mueller, A. S. & Osborne, M. Rekeying cultural scripts for youth suicide: how social networks facilitate suicide diffusion and suicide clusters following exposure to suicide. Soc. Ment. Health 10, 112–135 (2020).
Mueller, A. S. & Abrutyn, S. Adolescents under pressure: a new Durkheimian framework for understanding adolescent suicide in a cohesive community. Am. Sociol. Rev. 81, 877–899 (2016).
Zhu, C. et al. The Blue Whale Challenge from urban legend to real harm: case study analyses of Chinese suicide attempters. Curr. Psychol. 42, 15295–15306 (2023).
Khasawneh, A. et al. Examining the self-harm and suicide contagion effects of the Blue Whale Challenge on Youtube and Twitter: qualitative study. JMIR Ment. Health 7, e15973 (2020).
Lupariello, F., Curti, S. M., Coppo, E., Racalbuto, S. S. & Di Vella, G. Self-harm risk among adolescents and the phenomenon of the “Blue Whale Challenge”: case series and review of the literature. J. Forensic Sci. 64, 638–642 (2019).
Sumner, S. A. et al. Temporal and geographic patterns of social media posts about an emerging suicide game. J. Adolesc. Health 65, 94–100 (2019).
Balhara, Y. P. S., Bhargava, R., Pakhre, A. & Bhati, N. The “Blue Whale Challenge”?: the first report on a consultation from a health care setting for carrying out “tasks” accessed through a mobile phone application. Asia-Pacif. Psychiatry 10, e12317 (2018).
‘Blue Whale’ suicide game linked to 130 teen deaths is just tip of the iceberg in Russia. The Sun https://www.thesun.co.uk/news/3002981/blue-whale-game-suicide-russia-rules-challenge-social-media/ (3 March 2017).
Kobilke, L. & Markiewitz, A. The Momo Challenge: measuring the extent to which YouTube portrays harmful and helpful depictions of a suicide game. SN Soc. Sci. 1, 86 (2021).
Niederkrotenthaler, T. et al. Association of increased youth suicides in the United States with the release of 13 Reasons Why. JAMA Psychiatry 76, 933–940 (2019).
da Rosa, G. S. et al. Thirteen Reasons Why: the impact of suicide portrayal on adolescents’ mental health. J. Psychiatr. Res. 108, 2–6 (2019).
Hong, V. et al. 13 reasons why: viewing patterns and perceived impact among youths at risk of suicide. Psychiat. Serv. 70, 107–114 (2019).
Till, B., Vesely, C., Mairhofer, D., Braun, M. & Niederkrotenthaler, T. Reports of adolescent psychiatric outpatients on the impact of the TV series “13 Reasons Why”: a qualitative study. J. Adolesc. Health 64, 414–415 (2019).
Zimerman, A. et al. Revisiting the Werther effect in the 21st century: bullying and suicidality among adolescents who watched 13 Reasons Why. J. Am. Acad. Child Adolesc. Psychiatry 57, 610–613.e2 (2018).
Cooper, M. T., Bard, D., Wallace, R., Gillaspy, S. & Deleon, S. Suicide attempt admissions from a single children’s hospital before and after the introduction of Netflix series 13 Reasons Why. J. Adolesc. Health 63, 688–693 (2018).
Feuer, V. & Havens, J. Teen suicide: fanning the flames of a public health crisis. J. Am. Acad. Child Adolesc. Psychiatry 56, 723–724 (2017).
Schmidtke, A. & Häfner, H. The Werther effect after television films: new evidence for an old hypothesis. Psychol. Med. 18, 665–676 (1988).
Lee, T., Park, H., Ryu, J.-M., Kim, N. & Kim, H.-W. The association between media-based exposure to nonsuicidal self-injury and emergency department visits for self-harm. J. Am. Acad. Child Adolesc. Psychiatry 62, 656–664 (2023).
Park, D.-h. Youth self-injury counseling has tripled in a year. Hani http://www.hani.co.kr/arti/society/rights/895831.html (2019).
Phillips, D. P. The influence of suggestion on suicide: substantive and theoretical implications of the Werther effect. Am. Sociol. Rev. 39, 340–354 (1974).
Tellis, G. J., MacInnis, D. J., Tirunillai, S. & Zhang, Y. What drives virality (sharing) of online digital content? The critical role of information, emotion, and brand prominence. J. Mark. 83, 1–20 (2019).
Shaman, J. et al. Quantifying suicide contagion at population scale. Sci. Adv. https://doi.org/10.1126/sciadv.adq4074 (2024). This study develops a framework to quantify suicidal contagion at a population level following celebrity suicides.
Asharani, P. V. et al. The impact of media reporting of suicides on subsequent suicides in Asia: a systematic review. Ann. Acad. Med. Singapore 53, 152–169 (2024).
Niederkrotenthaler, T. et al. Association between suicide reporting in the media and suicide: systematic review and meta-analysis. BMJ 368, m575 (2020). This systematic review and meta-analysis evaluates the association between and the potential explanatory mechanisms of media reporting of suicide and subsequent suicide rates.
Choi, Y. J. & Oh, H. Does media coverage of a celebrity suicide trigger copycat suicides?: evidence from Korean cases. J. Media Econ. 29, 92–105 (2016).
Niederkrotenthaler, T. et al. Copycat effects after media reports on suicide: a population-based ecologic study. Soc. Sci. Med. 69, 1085–1090 (2009).
Stack, S. in Life Span Perspectives of Suicide (ed. Leenaars, A. A.) 187–213 (Springer, 1991).
Niederkrotenthaler, T., Reidenberg, D. J., Till, B. & Gould, M. S. Increasing help-seeking and referrals for individuals at risk for suicide by decreasing stigma: the role of mass media. Am. J. Prev. Med. 47, S235–S243 (2014).
Kim, E. & Kim, S. Spatially clustered patterns of suicide mortality rates in South Korea: a geographically weighted regression analysis. BMC Publ. Health 24, 2380 (2024).
Choi, W.-S. et al. An exploratory study on spatiotemporal clustering of suicide in Korean adolescents. Child Adolesc. Psychiatry Ment. Health 18, 54 (2024).
Lu, F.-W. et al. Space–time self-harm and suicide clusters in two cities in Taiwan. Epidemiol. Psychiat. Sci. 32, e37 (2023).
Yeung, C. Y., Men, V. Y., Guo, Y. & Yip, P. S. F. Spatial–temporal analysis of suicide clusters for suicide prevention in Hong Kong: a territory-wide study using 2014–2018 Hong Kong Coroner’s court reports. Lancet Reg. Health West. Pacif. 39, 100820 (2023).
Sugg, M. M., Woolard, S., Lawrimore, M., Michael, K. D. & Runkle, J. D. Spatial clustering of suicides and neighborhood determinants in North Carolina, 2000 to 2017. Appl. Spat. Anal. Policy 14, 395–413 (2021).
Hill, N. T. M., Spittal, M. J., Pirkis, J., Torok, M. & Robinson, J. Risk factors associated with suicide clusters in Australian youth: identifying who is at risk and the mechanisms associated with cluster membership. eClinicalMedicine 29, 100631 (2020).
Yamaoka, K., Suzuki, M., Inoue, M., Ishikawa, H. & Tango, T. Spatial clustering of suicide mortality and associated community characteristics in Kanagawa prefecture, Japan, 2011–2017. BMC Psychiatry 20, 74 (2020).
Kassem, A. M., Carter, K. K., Johnson, C. J. & Hahn, C. G. Spatial clustering of suicide and associated community characteristics, Idaho, 2010–2014. Prev. Chronic. Dis. 16, E37 (2019).
Fontanella, C. A. et al. Mapping suicide mortality in Ohio: a spatial epidemiological analysis of suicide clusters and area level correlates. Prev. Med. 106, 177–184 (2018).
Johnson, A. M., Woodside, J. M., Johnson, A. & Pollack, J. M. Spatial patterns and neighborhood characteristics of overall suicide clusters in Florida from 2001 to 2010. Am. J. Prev. Med. 52, e1–e7 (2017).
Too, L. S., Pirkis, J., Milner, A. & Spittal, M. J. Clusters of suicides and suicide attempts: detection, proximity and correlates. Epidemiol. Psychiat. Sci. 26, 491–500 (2017).
Robinson, J., Too, L. S., Pirkis, J. & Spittal, M. J. Spatial suicide clusters in Australia between 2010 and 2012: a comparison of cluster and non-cluster among young people and adults. BMC Psychiatry 16, 417 (2016).
Derek Cheung, Y. T., Spittal, M. J., Williamson, M. K., Tung, S. J. & Pirkis, J. Predictors of suicides occurring within suicide clusters in Australia, 2004–2008. Soc. Sci. Med. 118, 135–142 (2014).
Laliberté, A. & Tousignant, M. Alcohol and other contextual factors of suicide in four Aboriginal communities of Quebec, Canada. Crisis 30, 215–221 (2009).
Hanssens, L. & Hanssens, P. Research into the clustering effect of suicide within indigenous communities, Northern Territory, Australia. Aborig. Islander Health Work. J. 31, 6–10 (2007).
Wissow, L. S., Walkup, J., Barlow, A., Reid, R. & Kane, S. Cluster and regional influences on suicide in a southwestern American Indian tribe. Soc. Sci. Med. 53, 1115–1124 (2001).
Kim, K., Lee, D. W. & Jung, S. J. Role of individual deprivation and community-level deprivation on suicidal behaviors: insights from the UK Biobank study. SSM - Popul. Health 26, 101654 (2024).
Qian, J., Zeritis, S., Larsen, M. & Torok, M. The application of spatial analysis to understanding the association between area-level socio-economic factors and suicide: a systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 58, 843–859 (2023).
Cairns, J.-M., Graham, E. & Bambra, C. Area-level socioeconomic disadvantage and suicidal behaviour in Europe: a systematic review. Soc. Sci. Med. 192, 102–111 (2017).
Rehkopf, D. H. & Buka, S. L. The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. Psychol. Med. 36, 145–157 (2006).
Rosoff, D. B., Kaminsky, Z. A., McIntosh, A. M., Davey Smith, G. & Lohoff, F. W. Educational attainment reduces the risk of suicide attempt among individuals with and without psychiatric disorders independent of cognition: a bidirectional and multivariable Mendelian randomization study with more than 815,000 participants. Transl. Psychiatry 10, 388 (2020).
Pamela, S. et al. Research review: intergenerational transmission of disadvantage: epigenetics and parents’ childhoods as the first exposure. J. Child Psychol. Psychiatry 60, 119–132 (2018).
Mok, P. L. H. et al. Family income inequalities and trajectories through childhood and self-harm and violence in young adults: a population-based, nested case-control study. Lancet Publ. Health 3, e498–e507 (2018).
Iemmi, V. et al. Suicide and poverty in low-income and middle-income countries: a systematic review. Lancet Psychiatry 3, 774–783 (2016).
Yu, M. et al. The familial transmission of suicide and non-suicidal self-injury in different income levels in town. Int. J. Soc. Psychiatry 70, 988–998 (2024).
Wickham, S., Whitehead, M., Taylor-Robinson, D. & Barr, B. The effect of a transition into poverty on child and maternal mental health: a longitudinal analysis of the UK millennium cohort study. Lancet Publ. Health 2, e141–e148 (2017).
Conger, R. D., Conger, K. J. & Martin, M. J. Socioeconomic status, family processes, and individual development. J. Marriage Fam. 72, 685–704 (2010).
Green, J. G. et al. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) I: associations with first onset of DSM-IV disorders. Arch. Gen. Psychiatry 67, 113–123 (2010).
Dunn, M. S., Goodrow, B., Givens, C. & Austin, S. Substance use behavior and suicide indicators among rural middle school students. J. Sch. Health 78, 26–31 (2008).
Searles, V. B., Valley, M. A., Hedegaard, H. & Betz, M. E. Suicides in urban and rural counties in the United States, 2006–2008. Crisis 35, 18–26 (2014).
Shah, A., Sinha, T. & Makena, R. The relationship between elderly suicide rates, population density and room density. Int. Psychogeriatr. 21, 1197–1198 (2009).
Denney, J. T., Wadsworth, T., Rogers, R. G. & Pampel, F. C. Suicide in the city: do characteristics of place really influence risk? Soc. Sci. Q. 96, 313–329 (2015).
Cohen, P. N. The rise of one-person households. Socius https://doi.org/10.1177/23780231211062315 (2021).
Hoffmann, J. A. et al. Association of youth suicides and county-level mental health professional shortage areas in the US. JAMA Pediat. 177, 71–80 (2023).
Nakanishi, M. & Endo, K. National suicide prevention, local mental health resources, and suicide rates in Japan. Crisis 38, 384–392 (2017).
Walsh, B. W. & Rosen, P. Self-mutilation and contagion: an empirical test. Am. J. Psychiatry 142, 119–120 (1985).
Rosen, P. M. & Walsh, B. W. Patterns of contagion in self-mutilation epidemics. Am. J. Psychiatry 146, 656–658 (1989).
Taiminen, T. J., Kallio-soukainen, K., Nokso-koivisto, H., Kaljonen, A. & Helenius, H. Contagion of deliberate self-harm among adolescent inpatients. J. Am. Acad. Child Adolesc. Psychiatry 37, 211–217 (1998).
Beck, N. C. et al. Contagion of violence and self-harm behaviors on a psychiatric ward. J. Forens. Psychiatry Psychol. 29, 989–1006 (2018).
Jacobs, R., Grobler, C. & Strumpher, J. Identifying a probable suicide cluster in an acute care psychiatric hospital in the Eastern Cape, South Africa. South. Afr. J. Psychiatry 27, 1646 (2021).
Hawton, K., Linsell, L., Adeniji, T., Sariaslan, A. & Fazel, S. Self-harm in prisons in England and Wales: an epidemiological study of prevalence, risk factors, clustering, and subsequent suicide. Lancet 383, 1147–1154 (2014).
Hales, H., Edmondson, A., Davison, S., Maughan, B. & Taylor, P. J. The impact of contact with suicide-related behavior in prison on young offenders. Crisis 36, 21–30 (2015).
Hales, H., Davison, S., Misch, P. & Taylor, P. J. Young male prisoners in a Young Offenders’ Institution: their contact with suicidal behaviour by others. J. Adolesc. 26, 667–685 (2003).
Scherr, S. & Steinleitner, A. Zwischen dem Werther- und Papageno-effekt. Nervenarzt 86, 557–565 (2015).
Niederkrotenthaler, T. et al. Role of media reports in completed and prevented suicide: Werther v. Papageno effects. Br. J. Psychiatry 197, 234–243 (2010).
Arendt, F., Till, B., Gutsch, A. & Niederkrotenthaler, T. Social media influencers and the Papageno effect: experimental evidence for the suicide-preventive impact of social media posts on hope, healing, and recovery. Soc. Sci. Med. 370, 117852 (2025).
Till, B., Arendt, F., Scherr, S. & Niederkrotenthaler, T. Effect of educative suicide prevention news articles featuring experts with vs without personal experience of suicidal ideation: a randomized controlled trial of the Papageno effect. J. Clin. Psychiatry 80, 17m11975 (2018).
Niederkrotenthaler, T. & Till, B. Effects of suicide awareness materials on individuals with recent suicidal ideation or attempt: online randomised controlled trial. Br. J. Psychiatry 217, 693–700 (2020).
Ng, Y. P., Panirselvam, R. R. & Chan, L. F. in Suicide by Self-Immolation: Biopsychosocial and Transcultural Aspects (eds Alfonso, C. A. et al.) 231–246 (Springer, 2021).
Guidry, J. P. D., O’Donnell, N. H., Miller, C. A., Perrin, P. B. & Carlyle, K. E. Pinning despair and distress — suicide-related content on visual social media platform Pinterest. Crisis 42, 270–277 (2021) .
Pirkis, J. et al. Public health measures related to the transmissibility of suicide. Lancet Publ. Health 9, e807–e815 (2024). This review discusses the transmission of suicide risk through news and/or entertainment media, social media, media campaigns, secondary schools and suicide clusters, and proposes preventive approaches.
#chatsafe: A young person’s guide to communicating safely online about self-harm and suicide. Orygen https://www.orygen.org.au/chatsafe (2023).
APA panel issues recommendations for adolescent social media use. American Psychological Association https://www.apa.org/news/press/releases/2023/05/adolescent-social-media-use-recommendations (2023).
Preventing suicide: a resource for media professionals, update 2023. World Health Organization & International Association for Suicide Prevention https://who.int/publications/i/item/9789240076846 (2023).
Recommendations on suicide reporting & online information dissemination for media professionals. CSRP https://csrp.hku.hk/suicide-reporting-for-media-professionals/ (2022).
Mindset: reporting on mental health. Mindset https://www.mindset-mediaguide.ca (2020).
Best practices and recommendations for reporting on suicide. Reporting on Suicide https://reportingonsuicide.org (2024).
Samaritans’ media guidelines for reporting suicide. Samaritans https://www.samaritans.org/about-samaritans/media-guidelines/media-guidelines-reporting-suicide/ (2020).
Reporting suicide and mental ill-health: a Mindframe resource for media professionals. Mindframe https://mindframe.org.au/guidelines (2020).
Media guidelines for reporting suicides. Centre for Mental Health Law & Policy https://cmhlp.org/wp-content/uploads/2021/04/Resource-2-SPIRIT-Media-Guidelines-for-Reporting-Suicides.pdf (2019).
Sala, L. L. et al. Acceptability and potential impact of the #chatsafe suicide postvention response among young people who have been exposed to suicide: pilot study. JMIR Hum. Factors 10, e44535 (2023).
Sala, L. L. et al. Can a social media intervention improve online communication about suicide? A feasibility study examining the acceptability and potential impact of the #chatsafe campaign. PLoS ONE 16, e0253278 (2021).
Niederkrotenthaler, T. & Sonneck, G. Assessing the impact of media guidelines for reporting on suicides in Austria: interrupted time series analysis. Aust. NZ J. Psychiatry 41, 419–428 (2007).
Jang, J. et al. Effect of suicide prevention law and media guidelines on copycat suicide of general population following celebrity suicides in South Korea, 2005–2017. Aust. NZ J. Psychiatry 56, 542–550 (2022).
Cheng, Q., Chen, F., Lee, E. S. T. & Yip, P. S. F. The role of media in preventing student suicides: a Hong Kong experience. J. Affect. Disord. 227, 643–648 (2018).
Barker, E., Kolves, K. & De Leo, D. Rail-suicide prevention: systematic literature review of evidence-based activities. Asia-Pacif. Psychiatry 9, e12246 (2017).
Bohanna, I. & Wang, X. Media guidelines for the responsible reporting of suicide. Crisis 33, 190–198 (2012).
Sorensen, C. C. et al. The Tool for Evaluating Media Portrayals Of Suicide (TEMPOS): development and application of a novel rating scale to reduce suicide contagion. Int. J. Environ. Res. Public. Health 19, 2994 (2022). This study introduces a quantitative tool (TEMPOS) to assess adherence to media guidelines for suicide reporting.
Niederkrotenthaler, T. et al. Effects of media stories of hope and recovery on suicidal ideation and help-seeking attitudes and intentions: systematic review and meta-analysis. Lancet Publ. Health 7, e156–e168 (2022).
Banerjee, D., Kosagisharaf, J. R. & Sathyanarayana Rao, T. S. ‘The dual pandemic’ of suicide and COVID-19: a biopsychosocial narrative of risks and prevention. Psychiatry Res. 295, 113577 (2021). This article adopts a biopsychosocial perspective to analyse the potential impact of COVID-19 on suicide contagion and discusses mechanisms for prevention.
Moore, J. B. & June, C. H. Cytokine release syndrome in severe COVID-19. Science 368, 473–474 (2020).
Zhang, C., Wu, Z., Li, J.-W., Zhao, H. & Wang, G.-Q. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int. J. Antimicrob. Agents 55, 105954 (2020).
Isung, J. et al. High interleukin-6 and impulsivity: determining the role of endophenotypes in attempted suicide. Transl. Psychiatry 4, e470 (2014).
Lindqvist, D. et al. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol. Psychiatry 66, 287–292 (2009).
TikTok’s viral challenges keep luring young kids to their deaths. Bloomberg https://www.bloomberg.com/news/features/2022-11-30/is-tiktok-responsible-if-kids-die-doing-dangerous-viral-challenges? (2022).
Moutier, C. Suicide prevention in the COVID-19 era: transforming threat into opportunity. JAMA Psychiatry 78, 433–438 (2021).
Reger, M. A., Stanley, I. H. & Joiner, T. E. Suicide mortality and coronavirus disease 2019 — a perfect storm? JAMA Psychiatry 77, 1093–1094 (2020).
Dudgeon, P., Calma, T. & Holland, C. The context and causes of the suicide of Indigenous people in Australia. J. Indig. Wellbeing Te Mauri 2, 5–15 (2017). This article attributes Indigenous suicide clusters to systemic historical trauma and ongoing inequities, advocating for community-led prevention.
Leenaars, A. A. & Avenue, O. Genocide and suicide among indigenous people: the North meets the South. Can. J. Native Stud. 19, 337–363 (1999).
Atkinson, J. Educaring: a trauma informed approach to healing generational trauma for aboriginal Australians. Goolmangar NSW We Al-Li https://www.oics.wa.gov.au/wp-content/uploads/2017/07/Judy-Atkinson-Healing-From-Generational-Trauma-Workbook-We-Al-li.pdf (2012).
McLachlan, R., Gilfillan, G. & Gordon, J. Deep and Persistent Disadvantage in Australia (Productivity Commission, 2013).
Chandler, M. J. & Lalonde, C. Cultural continuity as a hedge against suicide in Canada’s First Nations. Transcult. Psychiatry 35, 191–219 (1998).
Chandler, M. J. & Lalonde, C. E. Cultural continuity as a protective factor against suicide in first nations youth. Horizons 10, 68–72 (2008).
Heilbron, N. & Prinstein, M. J. Peer influence and adolescent nonsuicidal self-injury: a theoretical review of mechanisms and moderators. Appl. Prev. Psychol. 12, 169–177 (2008).
Calear, A. L., Morse, A. R., Batterham, P. J., Forbes, O. & Banfield, M. Silence is deadly: a controlled trial of a public health intervention to promote help-seeking in adolescent males. Suicide Life-Threat. Behav. 51, 274–288 (2021).
Tyler, P. M., Hillman, D. S. & Ringle, J. L. Peer relations training moderates trauma symptoms and suicide ideation for youth in a residential program. J. Child Fam. Stud. 31, 447–458 (2022).
Hart, L. M., Cropper, P., Morgan, A. J., Kelly, C. M. & Jorm, A. F. Teen mental health first aid as a school-based intervention for improving peer support of adolescents at risk of suicide: outcomes from a cluster randomised crossover trial. Aust. NZ J. Psychiatry 54, 382–392 (2019).
Cha, J. M. et al. Five months follow-up study of school-based crisis intervention for Korean high school students who experienced a peer suicide. J. Korean Med. Sci. 33, e192 (2018).
Zhang, N., Sandler, I., Tein, J.-Y. & Wolchik, S. Reducing suicide risk in parentally bereaved youth through promoting effective parenting: testing a developmental cascade model. Dev. Psychopathol. 35, 433–446 (2023).
Kalafat, J. & Gagliano, C. The use of simulations to assess the impact of an adolescent suicide response curriculum. Suicide Life-Threat. Behav. 26, 359–364 (1996).
Kalafat, J. & Elias, M. An evaluation of a school-based suicide awareness intervention. Suicide Life-Threat. Behav. 24, 224–233 (1994).
Gleason, L. L. et al. Under the surface: the role of covert cues in peer suicide risk referrals. Sch. Ment. Health 14, 125–135 (2022).
Tiedemann, B. L. School-based mental health programs for preadolescent girls: mitigating social contagion of non-suicidal self-injury. Can. J. Couns. Psychother. 56, 24–46 (2022).
Gooda, M. & Dudgeon, P. The Elders’ report into preventing Indigenous self-harm and youth suicide. Australian Policy Online https://apo.org.au/node/266421 (2018).
Garcia, D., Mavrodiev, P., Casati, D. & Schweitzer, F. Understanding popularity, reputation, and social influence in the Twitter society. Policy Internet 9, 343–364 (2017).
Mercken, L., Snijders, T. A. B., Steglich, C., Vertiainen, E. & De Vries, H. Smoking-based selection and influence in gender-segregated friendship networks: a social network analysis of adolescent smoking. Addiction 105, 1280–1289 (2010).
Acknowledgements
The authors thank the Humanity and Social Science Youth foundation of the Ministry of Education (grant 22YJCZH018) for support.
Author information
Authors and Affiliations
Contributions
X.W., W.Y. and R.C. conceived the paper. X.W. conducted the literature review, drafted the initial full manuscript, and created all tables and figures. S.S., D.L., W.Y. and R.C. provided comprehensive revisions to the manuscript, critically refining its structure and theoretical arguments. All authors reviewed the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Psychology thanks Delfina Bilello, Massimiliano Orri and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wen, X., Sun, S., Lin, D. et al. A social ecological approach to social contagion of self-harm among young people. Nat Rev Psychol 4, 718–736 (2025). https://doi.org/10.1038/s44159-025-00495-1
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44159-025-00495-1