Abstract
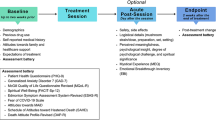
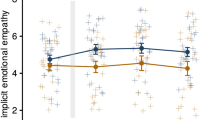
Psilocybin-assisted psychotherapy (PAP) has shown promise in treating mood and anxiety disorders in patients with cancer. However, patients with cancer often suffer from more than just depression and anxiety, and so far, PAP’s effect on other psychiatric symptoms remains largely unknown. To address this gap, we pooled previously unpublished data from two phase II, randomized, placebo-controlled crossover trials involving 79 participants with cancer-related distress and analyzed PAP’s effect on 9 psychiatric symptom dimensions: anxiety, depression, interpersonal sensitivity, hostility, obsession–compulsion, somatization, phobia, paranoia and psychosis. PAP significantly improved anxiety, depression, interpersonal sensitivity, hostility, obsession–compulsion and somatization without inducing any lasting phobia, paranoia or psychosis. Clinical improvements were consistent between trials. Together, our findings suggest that PAP has the potential to be a comprehensive mental health treatment for patients with cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The clinical trial participants of both studies used in this Analysis did not consent to the public sharing of their raw data. However, anonymized individual participant data can be made available provided the following conditions are met: (1) there is a data-sharing agreement and (2) an analysis plan in place. Upon data sharing, data can only be used for the specified purposes. Requests for data can be made by contacting the corresponding author.
Code availability
There was no custom code used in this Analysis.
References
Derogatis, L. R. et al. The prevalence of psychiatric disorders among cancer patients. JAMA 249, 751–757 (1983).
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C. & Piantadosi, S. The prevalence of psychological distress by cancer site. Psychooncology 10, 19–28 (2001).
Peters, L., Brederecke, J., Franzke, A., de Zwaan, M. & Zimmermann, T. Psychological distress in a sample of inpatients with mixed cancer—a cross-sectional study of routine clinical data. Front Psychol 11, 591771 (2020).
Mitchell, A. J. et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 12, 160–174 (2011).
Pitman, A., Suleman, S., Hyde, N. & Hodgkiss, A. Depression and anxiety in patients with cancer. Br. Med. J. 361, k1415 (2018).
Andersen, B. L. et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J. Clin. Oncol. 32, 1605–1619 (2014).
Derogatis, L. R., Abeloff, M. D. & Melisaratos, N. Psychological coping mechanisms and survival time in metastatic breast cancer. JAMA 242, 1504–1508 (1979).
Grassi, L. et al. Hostility in cancer patients as an underexplored facet of distress. Psychooncology 30, 493–503 (2021).
Grassi, L., Caruso, R. & Nanni, M. G. Somatization and somatic symptom presentation in cancer: a neglected area. Int. Rev. Psychiatry 25, 41–51 (2013).
Andersen, B. L. et al. Management of anxiety and depression in adult survivors of cancer: ASCO guideline update. J. Clin. Oncol. 41, 3426–3453 (2023).
Zhang, L. et al. Cognitive behavioral therapy for anxiety and depression in cancer survivors: a meta-analysis. Sci. Rep. 12, 21466 (2022).
Taylor, S. E., Falke, R. L., Shoptaw, S. J. & Lichtman, R. R. Social support, support groups, and the cancer patient. J. Consult. Clin. Psychol. 54, 608–615 (1986).
Cain, E. N., Kohorn, E. I., Quinlan, D. M., Latimer, K. & Schwartz, P. E. Psychosocial benefits of a cancer support group. Cancer 57, 183–189 (1986).
Salsman, J. M. et al. Psychosocial interventions for cancer survivors: a meta-analysis of effects on positive affect. J. Cancer Surviv. 13, 943–955 (2019).
Ostuzzi, G., Matcham, F., Dauchy, S., Barbui, C. & Hotopf, M. Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst. Rev. 4, CD011006 (2018).
Miovic, M. & Block, S. Psychiatric disorders in advanced cancer. Cancer 110, 1665–1676 (2007).
Ng, C. G., Boks, M. P., Zainal, N. Z. & de Wit, N. J. The prevalence and pharmacotherapy of depression in cancer patients. J. Affect. Disord. 131, 1–7 (2011).
Azari, L. et al. The efficacy and safety of ketamine for depression in patients with cancer: a systematic review. Int. J. Clin. Health Psychol. 24, 100428 (2024).
Culp, C., Kim, H. K. & Abdi, S. Ketamine use for cancer and chronic pain management. Front. Pharmacol. 11, 599721 (2020).
Falk, E. et al. A rapid positive influence of S-ketamine on the anxiety of patients in palliative care: a retrospective pilot study. BMC Palliative Care 19, 1 (2020).
Ross, S. Therapeutic use of classic psychedelics to treat cancer-related psychiatric distress. Int. Rev. Psychiatry 30, 317–330 (2018).
Carhart-Harris, R. L. & Goodwin, G. M. The therapeutic potential of psychedelic drugs: past, present, and future. Neuropsychopharmacology 42, 2105–2113 (2017).
Ross, S. et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J. Psychopharmacol. 30, 1165–1180 (2016).
Griffiths, R. R. et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J. Psychopharmacol. 30, 1181–1197 (2016).
Goodwin, G. M. et al. Single-dose psilocybin for a treatment-resistant episode of major depression. N. Engl. J. Med. 387, 1637–1648 (2022).
Raison, C. L. et al. Single-dose psilocybin treatment for major depressive disorder: a randomized clinical trial. JAMA 330, 843–853 (2023).
Johnson, M. W., Garcia-Romeu, A., Cosimano, M. P. & Griffiths, R. R. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J. Psychopharmacol. 28, 983–992 (2014).
Bogenschutz, M. P. et al. Percentage of heavy drinking days following psilocybin-assisted psychotherapy vs placebo in the treatment of adult patients with alcohol use disorder: a randomized clinical trial. JAMA Psychiatry 79, 953–962 (2022).
Ehrmann, K., Allen, J. J. B. & Moreno, F. A. Psilocybin for the treatment of obsessive–compulsive disorders. Curr. Top. Behav. Neurosci. 56, 247–259 (2022).
Schneier, F. R. et al. Pilot study of single-dose psilocybin for serotonin reuptake inhibitor-resistant body dysmorphic disorder. J. Psychiatr. Res. 161, 364–370 (2023).
Ledwos, N., Rodas, J. D., Husain, M. I., Feusner, J. D. & Castle, D. J. Therapeutic uses of psychedelics for eating disorders and body dysmorphic disorder. J. Psychopharmacol. 37, 3–13 (2023).
Derogatis, L. R. & Melisaratos, N. The Brief Symptom Inventory: an introductory report. Psychol. Med. 13, 595–605 (1983).
Sarparast, A., Thomas, K., Malcolm, B. & Stauffer, C. S. Drug–drug interactions between psychiatric medications and MDMA or psilocybin: a systematic review. Psychopharmacology 239, 1945–1976 (2022).
Kwan, A. C., Olson, D. E., Preller, K. H. & Roth, B. L. The neural basis of psychedelic action. Nat. Neurosci. 25, 1407–1419 (2022).
Carhart-Harris, R. L. & Nutt, D. J. Serotonin and brain function: a tale of two receptors. J. Psychopharmacol. 31, 1091–1120 (2017).
Vollenweider, F. X. & Preller, K. H. Psychedelic drugs: neurobiology and potential for treatment of psychiatric disorders. Nat. Rev. Neurosci. 21, 611–624 (2020).
Petridis, P. D. A psychedelic state arises from desynchronized brain activity. Nature 632, 32–33 (2024).
Yeo, B. T. et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J. Neurophysiol. 106, 1125–1165 (2011).
Siegel, J. S. et al. Psilocybin desynchronizes the human brain. Nature 632, 131–138 (2024).
Smallwood, J. et al. The default mode network in cognition: a topographical perspective. Nat. Rev. Neurosci. 22, 503–513 (2021).
Zhou, H. X. et al. Rumination and the default mode network: meta-analysis of brain imaging studies and implications for depression. NeuroImage 206, 116287 (2020).
Madsen, M. K. et al. Psilocybin-induced changes in brain network integrity and segregation correlate with plasma psilocin level and psychedelic experience. Eur. Neuropsychopharmacol. 50, 121–132 (2021).
Daws, R. E. et al. Increased global integration in the brain after psilocybin therapy for depression. Nat. Med. 28, 844–851 (2022).
Vargas, M. V. et al. Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors. Science 379, 700–706 (2023).
Calder, A. E. & Hasler, G. Towards an understanding of psychedelic-induced neuroplasticity. Neuropsychopharmacology 48, 104–112 (2023).
Agin-Liebes, G. I. et al. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. J. Psychopharmacol. 34, 155–166 (2020).
Gukasyan, N. et al. Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: prospective 12-month follow-up. J. Psychopharmacol. 36, 151–158 (2022).
Yaden, D. B. & Griffiths, R. R. The subjective effects of psychedelics are necessary for their enduring therapeutic effects. ACS Pharmacol. Transl. Sci. 4, 568–572 (2021).
Belser, A. B. et al. Patient experiences of psilocybin-assisted psychotherapy: an interpretative phenomenological analysis. J. Humanist. Psychol. 57, 354–388 (2017).
Swift, T. C. et al. Cancer at the dinner table: experiences of psilocybin-assisted psychotherapy for the treatment of cancer-related distress. J. Humanist. Psychol. 57, 488–519 (2017).
Butler, M., Jelen, L. & Rucker, J. Expectancy in placebo-controlled trials of psychedelics: if so, so what? Psychopharmacology 239, 3047–3055 (2022).
Vodermaier, A., Linden, W. & Siu, C. Screening for emotional distress in cancer patients: a systematic review of assessment instruments. J. Natl Cancer Inst. 101, 1464–1488 (2009).
Pirl, W. F. et al. Recommendations for the implementation of distress screening programs in cancer centers: report from the American Psychosocial Oncology Society (APOS), Association of Oncology Social Work (AOSW), and Oncology Nursing Society (ONS) joint task force. Cancer 120, 2946–2954 (2014).
Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 6, 65–70 (1979).
Acknowledgements
The parent trials included in this Analysis were supported by grants from the Heffter Research Institute (R.R.G. and S.R.), the RiverStyx Foundation (R.R.G. and S.R.), the Betsy Gordon Foundation (R.R.G.), the Fetzer Institute (R.R.G.) and the New York University–Health and Hospitals Corporation–Clinical and Translational Science Institute grant UL1 TR000038 from the National Center for Advancing Translational Sciences, National Institutes of Health (NIH) (S.R.). Additional funding for the parent trials was provided by Carey and Claudia Turnbull (S.R.), W. Linton (R.R.G. and S.R.), R. Barnhart (S.R.), A. Altschul (S.R.), K. Fitzsimmons (S.R.), the McCormick Family (R.R.G.), G. Goldsmith (R.R.G. and S.R) and E. Malievskaia (R.R.G. and S.R.). Funding for the pooled analysis was provided by the Usona Institute scholarship (P.D.P), the NIH T32DA007250 (G.A.-L.) and the Canadian Institutes of Health Research (grant number 202110MFE-472921-HTB-272687) (R.J.Z.). Sponsors did not have roles in the management, analysis or interpretation of the data, nor in the preparation or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
P.D.P. and S.R. conceived of the analysis. R.R.G. and S.R. provided deidentified individual participant data from their respective parent clinical trials. P.D.P. analyzed the data with support from J.G. and M.P.B. P.D.P., J.G., G.A.-L., C.J.K., R.J.Z., M.P.B., R.R.G. and S.R. interpreted the results of the analysis. P.D.P. wrote the paper. P.D.P., J.G., G.A.-L., C.J.K., R.J.Z, M.P.B., R.R.G. and S.R. critically revised the article.
Corresponding author
Ethics declarations
Competing interests
R.J.Z. is a post-doctoral fellow in the NYU Langone Psychedelic Medicine Research Training program funded by MindMed. M.P.B. is principal investigator of the NYU Langone Center for Psychedelic Medicine Research Training Program, funded by MindMed. M.P.B. has received research funding from Tilray Canada, the Multidisciplinary Association for Psychedelic Studies (MAPS) PBC, B.More Inc., the Heffter Research Institute, the Turnbull Family Foundation, the Fournier Family Foundation, Dr. Bronner’s Family Foundation, Bill Linton and the Riverstyx Foundation. M.P.B. serves on the Advisory Board of Ajna Labs LLC, Journey Colab and Bright Minds Biosciences, Inc. He is named as inventor on patent applications relating to the use of psilocybin for alcohol use disorder but has waived all rights and has no prospect of financial benefit. S.R. is the Director of NYU Langone Center for Psychedelic Medicine Research Training Program, which is funded by MindMed. S.R. currently receives, or has received in the past 36 months, grant support for clinical research from the National Institute on Drug Abuse (NIDA), National Cancer Institute (NCI), Heffter Research Institute, Usona Institute, Council on Spiritual Practices (CSP), Multidisciplinary Association of Psychedelic Studies (MAPS) and Reset Pharmaceuticals. S.R. is listed as a coinventor in two provisional patent applications (N420838US and N419987US) related to the use of psilocybin to treat psychiatric and existential distress in cancer. These provisional patent applications were filed by New York University Grossman School of Medicine and licensed by Reset Pharmaceuticals. S.R. has waived all rights in relation to these provisional patent applications and has no prospect of financial gain related to any future commercialization efforts related to these patents. The other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Matthias Emanuel Liechti, Joshua Rosenblat and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Table 1 and Figs. 1 and 2.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Petridis, P.D., Grinband, J., Agin-Liebes, G. et al. Psilocybin-assisted psychotherapy improves psychiatric symptoms across multiple dimensions in patients with cancer. Nat. Mental Health 2, 1408–1414 (2024). https://doi.org/10.1038/s44220-024-00331-0
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-024-00331-0
This article is cited by
-
From relaxed beliefs under psychedelics (REBUS) to revised beliefs after psychedelics (REBAS)
Scientific Reports (2025)
-
End of life for glioblastoma patients
Supportive Care in Cancer (2025)
-
Psilocybin-assisted psychotherapy as an ‘anti-distressant’ with multidimensional properties
Nature Mental Health (2024)