Abstract
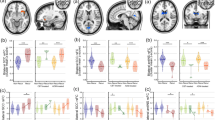
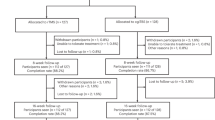
Repetitive transcranial magnetic stimulation is an effective treatment for depression that modulates resting-state functional connectivity (RSFC) of depression-relevant neural circuits. So far, however, few studies have investigated whether individual treatment-related symptom changes are predictable from pretreatment RSFC. Here we use machine learning to predict dimensional changes in depressive symptoms using pretreatment RSFC. We hypothesized that changes in dimensional depressive symptoms would be predicted more accurately than scale total scores. Patients with depression (n = 26) underwent pretreatment RSFC magnetic resonance imaging. Depressive symptoms were assessed with the 17-item Hamilton Depression Rating Scale (HDRS-17). Random forest regression models were trained to predict treatment-related symptom changes captured by the HDRS-17, HDRS-6 and three previously identified HDRS subscales: core mood and anhedonia (CMA), somatic disturbances and insomnia. Changes along the CMA, HDRS-17 and HDRS-6 were predicted significantly above chance, with 9%, 2% and 2% of out-of-sample outcome variance explained, respectively (all P values <0.001). CMA changes were predicted more accurately than the HDRS-17 (P < 0.05). Higher baseline global connectivity (GC) of default mode network subregions and the somatomotor network predicted poorer outcomes, while higher GC of the right dorsal attention frontoparietal control and visual networks predicted reduced CMA symptoms. HDRS-17 and HDRS-6 changes were predicted with similar GC patterns. These results suggest that RSFC spanning the default mode, somatomotor, dorsal attention, frontoparietal control and visual network subregions predict dimensional changes with significantly greater accuracy than syndromal changes after repetitive transcranial magnetic stimulation. These findings highlight the need to assess more granular clinical dimensions in therapeutic studies and echo earlier studies supporting that dimensional outcomes improve model accuracy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The dataset used for this study is not publicly available due to patient privacy concerns but may be made available from the corresponding author on request.
Code availability
Code used for this study is available via GitHub at https://github.com/bscwade/tms_moa_dimensional_predictions.
References
George, M. S., Taylor, J. J. & Short, E. B. The expanding evidence base for rTMS treatment of depression. Curr. Opin. Psychiatry 26, 13–18 (2013).
Cole, E. J. et al. Stanford Neuromodulation Therapy (SNT): a double-blind randomized controlled trial. Am. J. Psychiatry 179, 132–141 (2022).
Camprodon, J. A., Rauch, S. L., Greenberg, B. D., & Dougherty, D. D. (eds) Psychiatric Neurotherapeutics: Contemporary Surgical and Device-Based Treatments 1st edn (Springer, 2016).
Harika-Germaneau, G. et al. Baseline clinical and neuroimaging biomarkers of treatment response to high-frequency rTMS over the left DLPFC for resistant depression. Front. Psychiatry 13, 894473 (2022).
Brunoni, A. R. et al. Repetitive transcranial magnetic stimulation for the acute treatment of major depressive episodes: a systematic review with network meta-analysis. JAMA Psychiatry 74, 143–152 (2017).
Chervyakov, A. V., Chernyavsky, A. Y., Sinitsyn, D. O. & Piradov, M. A. Possible mechanisms underlying the therapeutic effects of transcranial magnetic stimulation. Front. Hum. Neurosci. 9, 303 (2015).
Camprodon, J. A. & Pascual-Leone, A. Multimodal applications of transcranial magnetic stimulation for circuit-based psychiatry. JAMA Psychiatry 73, 407–408 (2016).
Fox, M. D., Buckner, R. L., White, M. P., Greicius, M. D. & Pascual-Leone, A. Efficacy of transcranial magnetic stimulation targets for depression is related to intrinsic functional connectivity with the subgenual cingulate. Biol. Psychiatry 72, 595–603 (2012).
Drevets, W. C., Savitz, J. & Trimble, M. The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 13, 663–681 (2008).
Mayberg, H. S. Defining the neural circuitry of depression: toward a new nosology with therapeutic implications. Biol. Psychiatry 61, 729–730 (2007).
Pizzagalli, D. A. Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacology 36, 183–206 (2011).
Cash, R. F. H. et al. A multivariate neuroimaging biomarker of individual outcome to transcranial magnetic stimulation in depression. Hum. Brain Mapp. 40, 4618–4629 (2019).
Liston, C. et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol. Psychiatry 76, 517–526 (2014).
Boes, A. D. et al. Rostral anterior cingulate cortex is a structural correlate of repetitive TMS treatment response in depression. Brain Stimul. 11, 575–581 (2018).
Baeken, C., van Beek, V., Vanderhasselt, M. A., Duprat, R. & Klooster, D. Cortical thickness in the right anterior cingulate cortex relates to clinical response to left prefrontal accelerated intermittent theta burst stimulation: an exploratory study. Neuromodulation 24, 938–949 (2021).
Buch, A. M. & Liston, C. Dissecting diagnostic heterogeneity in depression by integrating neuroimaging and genetics. Neuropsychopharmacology 46, 156–175 (2021).
Drysdale, A. T. et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat. Med. 23, 28–38 (2017).
Siddiqi, S. H. et al. Distinct symptom-specific treatment targets for circuit-based neuromodulation. Am. J. Psychiatry 177, 435–446 (2020).
Bagby, R. M., Ryder, A. G., Schuller, D. R. & Marshall, M. B. The Hamilton Depression Rating Scale: has the gold standard become a lead weight? Am. J. Psychiatry 161, 2163–2177 (2004).
Maier, W., Heuser, I., Philipp, M., Frommberger, U. & Demuth, W. Improving depression severity assessment–II. Content, concurrent and external validity of three observer depression scales. J. Psychiatr. Res. 22, 13–19 (1988).
Bech, P. et al. The Hamilton depression scale. Evaluation of objectivity using logistic models. Acta Psychiatr. Scand. 63, 290–299 (1981).
Boone, W. J. Rasch analysis for instrument development: why, when, and how? CBE Life Sci. Educ. 15, rm4 (2016).
Timmerby, N., Andersen, J. H., Sondergaard, S., Ostergaard, S. D. & Bech, P. A systematic review of the clinimetric properties of the 6-Item Version of the Hamilton Depression Rating Scale (HAM-D6). Psychother. Psychosom. 86, 141–149 (2017).
Wade, B. S. C. et al. Accounting for symptom heterogeneity can improve neuroimaging models of antidepressant response after electroconvulsive therapy. Hum. Brain Mapp. 42, 5322–5333 (2021).
Wade, B. S. C. et al. Anterior default mode network and posterior insular connectivity is predictive of depressive symptom reduction following serial ketamine infusion—CORRIGENDUM. Psychol. Med. 52, 2399 (2022).
Razza, L. B. et al. A systematic review and meta-analysis on placebo response to repetitive transcranial magnetic stimulation for depression trials. Prog. Neuropsychopharmacol. Biol. Psychiatry 81, 105–113 (2018).
Andrews-Hanna, J. R., Reidler, J. S., Sepulcre, J., Poulin, R. & Buckner, R. L. Functional–anatomic fractionation of the brain’s default network. Neuron 65, 550–562 (2010).
Ochsner, K. N. et al. Reflecting upon feelings: an fMRI study of neural systems supporting the attribution of emotion to self and other. J. Cogn. Neurosci. 16, 1746–1772 (2004).
Buckner, R. L. & DiNicola, L. M. The brain’s default network: updated anatomy, physiology and evolving insights. Nat. Rev. Neurosci. 20, 593–608 (2019).
Mulders, P. C. et al. Default mode network coherence in treatment-resistant major depressive disorder during electroconvulsive therapy. J. Affect. Disord. 205, 130–137 (2016).
Zhou, H. X. et al. Rumination and the default mode network: meta-analysis of brain imaging studies and implications for depression. NeuroImage 206, 116287 (2020).
Hamilton, J. P., Farmer, M., Fogelman, P. & Gotlib, I. H. Depressive rumination, the default-mode network, and the dark matter of clinical neuroscience. Biol. Psychiatry 78, 224–230 (2015).
Sheline, Y. I. et al. The default mode network and self-referential processes in depression. Proc. Natl Acad. Sci. USA 106, 1942–1947 (2009).
Foroughi, A. et al. The effectiveness of mindfulness-based cognitive therapy for reducing rumination and improving mindfulness and self-compassion in patients with treatment-resistant depression. Trends Psychiatry Psychother. 42, 138–146 (2020).
Dunlop, K. et al. MRI-guided dmPFC-rTMS as a treatment for treatment-resistant major depressive disorder. J. Vis. Exp. 11, e53129 (2015).
Muller, V. I., Langner, R., Cieslik, E. C., Rottschy, C. & Eickhoff, S. B. Interindividual differences in cognitive flexibility: influence of gray matter volume, functional connectivity and trait impulsivity. Brain Struct. Funct. 220, 2401–2414 (2015).
Kuhn, S., Gallinat, J. & Brass, M. ‘Keep calm and carry on’: structural correlates of expressive suppression of emotions. PLoS ONE 6, e16569 (2011).
Jung, Y. C. et al. Synchrony of anterior cingulate cortex and insular-striatal activation predicts ambiguity aversion in individuals with low impulsivity. Cereb. Cortex 24, 1397–1408 (2014).
Downar, J. & Daskalakis, Z. J. New targets for rTMS in depression: a review of convergent evidence. Brain Stimul. 6, 231–240 (2013).
Dunlop, K. et al. Reductions in cortico-striatal hyperconnectivity accompany successful treatment of obsessive–compulsive disorder with dorsomedial prefrontal rTMS. Neuropsychopharmacology 41, 1395–1403 (2016).
Feffer, K. et al. Dorsomedial prefrontal rTMS for depression in borderline personality disorder: a pilot randomized crossover trial. J. Affect. Disord. 301, 273–280 (2022).
Mulders, P. C., van Eijndhoven, P. F., Schene, A. H., Beckmann, C. F. & Tendolkar, I. Resting-state functional connectivity in major depressive disorder: a review. Neurosci. Biobehav. Rev. 56, 330–344 (2015).
Greicius, M. D. et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol. Psychiatry 62, 429–437 (2007).
Zhu, X. et al. Evidence of a dissociation pattern in resting-state default mode network connectivity in first-episode, treatment-naive major depression patients. Biol. Psychiatry 71, 611–617 (2012).
Salomons, T. V. et al. Resting-state cortico-thalamic-striatal connectivity predicts response to dorsomedial prefrontal rTMS in major depressive disorder. Neuropsychopharmacology 39, 488–498 (2014).
Cano, M. et al. Brain volumetric correlates of electroconvulsive therapy versus transcranial magnetic stimulation for treatment-resistant depression. J. Affect. Disord. 333, 140–146 (2023).
Buckner, R. L., Andrews-Hanna, J. R. & Schacter, D. L. The brain’s default network: anatomy, function, and relevance to disease. Ann. N. Y. Acad. Sci. 1124, 1–38 (2008).
Raichle, M. E. The brain’s default mode network. Annu. Rev. Neurosci. 38, 433–447 (2015).
Gusnard, D. A., Akbudak, E., Shulman, G. L. & Raichle, M. E. Medial prefrontal cortex and self-referential mental activity: relation to a default mode of brain function. Proc. Natl Acad. Sci. USA 98, 4259–4264 (2001).
Leech, R. & Sharp, D. J. The role of the posterior cingulate cortex in cognition and disease. Brain 137, 12–32 (2014).
Leech, R., Braga, R. & Sharp, D. J. Echoes of the brain within the posterior cingulate cortex. J. Neurosci. 32, 215–222 (2012).
Leech, R., Kamourieh, S., Beckmann, C. F. & Sharp, D. J. Fractionating the default mode network: distinct contributions of the ventral and dorsal posterior cingulate cortex to cognitive control. J. Neurosci. 31, 3217–3224 (2011).
van Tol, M. J. et al. Local cortical thinning links to resting-state disconnectivity in major depressive disorder. Psychol. Med. 44, 2053–2065 (2014).
Wise, T. et al. Instability of default mode network connectivity in major depression: a two-sample confirmation study. Transl. Psychiatry 7, e1105 (2017).
Berman, M. G. et al. Depression, rumination and the default network. Soc. Cogn. Affect. Neurosci. 6, 548–555 (2011).
Zhou, Y. et al. Increased neural resources recruitment in the intrinsic organization in major depression. J. Affect. Disord. 121, 220–230 (2010).
Bluhm, R. et al. Resting state default-mode network connectivity in early depression using a seed region-of-interest analysis: decreased connectivity with caudate nucleus. Psychiatry Clin. Neurosci. 63, 754–761 (2009).
Treynor, W., Gonzalez, R. & Nolen-Hoeksema, S. Rumination reconsidered: a psychometric analysis. Cogn. Ther. Res. 27, 247–259 (2003).
Yan, C. G. et al. Reduced default mode network functional connectivity in patients with recurrent major depressive disorder. Proc. Natl Acad. Sci. USA 116, 9078–9083 (2019).
Sacchet, M. D. et al. Large-scale hypoconnectivity between resting-state functional networks in unmedicated adolescent major depressive disorder. Neuropsychopharmacology 41, 2951–2960 (2016).
Korgaonkar, M. S., Goldstein-Piekarski, A. N., Fornito, A. & Williams, L. M. Intrinsic connectomes are a predictive biomarker of remission in major depressive disorder. Mol. Psychiatry 25, 1537–1549 (2020).
Leaver, A. M. et al. Fronto-temporal connectivity predicts ECT outcome in major depression. Front. Psychiatry 9, 92 (2018).
Kaiser, R. H., Andrews-Hanna, J. R., Wager, T. D. & Pizzagalli, D. A. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry 72, 603–611 (2015).
Sambataro, F. et al. Altered dynamics of brain connectivity in major depressive disorder at-rest and during task performance. Psychiatry Res. Neuroimaging 259, 1–9 (2017).
Armstrong, T. & Olatunji, B. O. Eye tracking of attention in the affective disorders: a meta-analytic review and synthesis. Clin. Psychol. Rev. 32, 704–723 (2012).
Golomb, J. D. et al. Enhanced visual motion perception in major depressive disorder. J. Neurosci. 29, 9072–9077 (2009).
Chen, C. et al. Decreased cortical folding of the fusiform gyrus and its hypoconnectivity with sensorimotor areas in major depressive disorder. J. Affect. Disord. 295, 657–664 (2021).
Ho, T. C. et al. Fusiform gyrus dysfunction is associated with perceptual processing efficiency to emotional faces in adolescent depression: a model-based approach. Front. Psychol. 7, 40 (2016).
Sahib, A. K. et al. Modulation of the functional connectome in major depressive disorder by ketamine therapy. Psychol. Med. 52, 2596–2605 (2022).
Moreno-Ortega, M. et al. Resting state functional connectivity predictors of treatment response to electroconvulsive therapy in depression. Sci. Rep. 9, 5071 (2019).
Doehrmann, O. et al. Predicting treatment response in social anxiety disorder from functional magnetic resonance imaging. JAMA Psychiatry 70, 87–97 (2013).
Chen, H. et al. More optimal but less regulated dorsal and ventral visual networks in patients with major depressive disorder. J. Psychiatr. Res. 110, 172–178 (2019).
Whitfield-Gabrieli, S. et al. Brain connectomics predict response to treatment in social anxiety disorder. Mol. Psychiatry 21, 680–685 (2016).
Wu, F., Lu, Q., Kong, Y. & Zhang, Z. A comprehensive overview of the role of visual cortex malfunction in depressive disorders: opportunities and challenges. Neurosci. Bull. 39, 1426–1438 (2023).
Stephan-Otto, C. et al. Neural activity during object perception in schizophrenia patients is associated with illness duration and affective symptoms. Schizophr. Res. 175, 27–34 (2016).
Marek, S. & Dosenbach, N. U. F. The frontoparietal network: function, electrophysiology, and importance of individual precision mapping. Dialogues Clin. Neurosci. 20, 133–140 (2018).
Cole, M. W., Repovs, G. & Anticevic, A. The frontoparietal control system: a central role in mental health. Neuroscientist 20, 652–664 (2014).
Zweerings, J. et al. Fronto-parietal and temporal brain dysfunction in depression: a fMRI investigation of auditory mismatch processing. Hum. Brain Mapp. 40, 3657–3668 (2019).
Schultz, D. H. et al. Global connectivity of the fronto-parietal cognitive control network is related to depression symptoms in the general population. Netw. Neurosci. 3, 107–123 (2019).
Zhang, H., Nettleton, D. & Zhu, Z. Regression-enhanced random forests. In Joint Statistical Meetings Proc. 636–647 (ASA, 2017).
Elbau, I. G. et al. Functional connectivity mapping for rTMS target selection in depression. Am. J. Psychiatry 180, 230–240 (2023).
Esteban, O. et al. fMRIPrep: a robust preprocessing pipeline for functional MRI. Nat. Methods 16, 111–116 (2019).
Tustison, N. J. et al. N4ITK: improved N3 bias correction. IEEE Trans. Med. Imaging 29, 1310–1320 (2010).
Klein, A. et al. Mindboggling morphometry of human brains. PLoS Comput. Biol. 13, e1005350 (2017).
Cox, R. W. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput. Biomed. Res. 29, 162–173 (1996).
Jenkinson, M., Bannister, P., Brady, M. & Smith, S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. NeuroImage 17, 825–841 (2002).
Behzadi, Y., Restom, K., Liau, J. & Liu, T. T. A component based noise correction method (CompCor) for BOLD and perfusion based fMRI. NeuroImage 37, 90–101 (2007).
Schaefer, A. et al. Local–global parcellation of the human cerebral cortex from intrinsic functional connectivity MRI. Cereb. Cortex 28, 3095–3114 (2018).
Kelly, C. et al. A convergent functional architecture of the insula emerges across imaging modalities. NeuroImage 61, 1129–1142 (2012).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31, 968–980 (2006).
Pauli, W. M., Nili, A. N. & Tyszka, J. M. A high-resolution probabilistic in vivo atlas of human subcortical brain nuclei. Sci. Data 5, 180063 (2018).
Tyszka, J. M. & Pauli, W. M. In vivo delineation of subdivisions of the human amygdaloid complex in a high-resolution group template. Hum. Brain Mapp. 37, 3979–3998 (2016).
Abraham, A. et al. Machine learning for neuroimaging with scikit-learn. Front. Neuroinform. 8, 14 (2014).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62 (1960).
O’Sullivan, R. L., Fava, M., Agustin, C., Baer, L. & Rosenbaum, J. F. Sensitivity of the six-item Hamilton Depression Rating Scale. Acta Psychiatr. Scand. 95, 379–384 (1997).
Wade, B. S. C. et al. Depressive symptom dimensions in treatment-resistant major depression and their modulation with electroconvulsive therapy. J. ECT 36, 123–129 (2020).
Snaith, R. P. et al. A scale for the assessment of hedonic tone the Snaith–Hamilton Pleasure Scale. Br. J. Psychiatry 167, 99–103 (1995).
Dietterich, T. G. Ensemble Methods in Machine Learning. In Multiple Classifier Systems: First International Workshop, Lecture notes in Computer Science, 1-15 (MCS, 2000).
Grinsztajn, L., Oyallon, E. & Varoquaux, G. Why do tree-based models still outperform deep learning on typical tabular data? Adv. Neural Inf. Process. Syst. 35, 507–520 (2022).
Wade, B. S. C., Joshi, S. H., Gutman, B. A. & Thompson, P. M. Machine learning on high dimensional shape data from subcortical brain surfaces: a comparison of feature selection and classification methods. Pattern Recogn. 63, 731–739 (2017).
Statnikov, A., Wang, L. & Aliferis, C. F. A comprehensive comparison of random forests and support vector machines for microarray-based cancer classification. BMC Bioinf. 9, 319 (2008).
Poldrack, R. A., Huckins, G. & Varoquaux, G. Establishment of best practices for evidence for prediction: a review. JAMA Psychiatry 77, 534–540 (2020).
Phipson, B. & Smyth, G. K. Permutation P-values should never be zero: calculating exact P-values when permutations are randomly drawn. Stat. Appl. Genet. Mol. Biol. 9, Article39 (2010).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
Altmann, A., Tolosi, L., Sander, O. & Lengauer, T. Permutation importance: a corrected feature importance measure. Bioinformatics 26, 1340–1347 (2010).
Acknowledgements
This work was supported by a K99/R00 Pathway to Independence Award (MH119314 to B.S.C.W.) and NIH grants R01MH112737 and R61MH132869 to J.A.C.
Author information
Authors and Affiliations
Contributions
B.S.C.W. designed the study’s machine learning and statistical methods, interpreted the findings and drafted the paper. J.A.C. oversaw and funded data acquisition efforts. T.A.B., K.K.E. and J.A.C. assisted in interpreting the findings and drafting the paper.
Corresponding author
Ethics declarations
Competing interests
J.A.C. is listed as an inventor on patents and patent applications on neuromodulation targeting methods held by Massachusetts General Hospital. He is a member of the scientific advisory board of Hyka and Flow Neuroscience, and has been a paid consultant for Mifu Technologies, Neuroelectrics, and LivaNova. The other authors report no conflicts of interest.
Peer review
Peer review information
Nature Mental Health thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Tables
Supplementary Table 1. Tabulation of atlas-based parcellations used in the analysis. Supplementary Table 2. Tabulation of Hamilton Depression Rating Scale items present in each subscale.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wade, B.S.C., Barbour, T.A., Ellard, K.K. et al. Predicting dimensional antidepressant response to repetitive transcranial magnetic stimulation using pretreatment resting-state functional connectivity. Nat. Mental Health 3, 1046–1056 (2025). https://doi.org/10.1038/s44220-025-00469-5
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-025-00469-5