Abstract
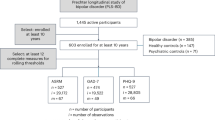
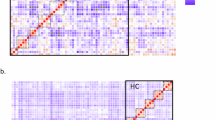
Increasing evidence suggests that bipolar disorders are associated with mood instability even outside the context of mood episodes. Here we use data from the Prechter Longitudinal Study of Bipolar Disorder to identify subgroups of individuals with bipolar disorders based on mood instability, identify biopsychosocial predictors of mood instability and determine whether mood instability predicts future outcomes. In a total of 481 participants, mood was assessed every 2 months (Patient Health Questionnaire and Altman Self-Rating Mania Scale) over 5 years, and clinical and functioning outcomes were assessed in year 6. Low, moderate and high mood instability classes were identified. Neuroticism, sleep quality, childhood emotional neglect and physical abuse, stimulant abuse, hypomania age of onset and number of depressive episodes were the most influential predictors of mood instability. Being in the high instability class (based on mood from years 1 to 5) predicted greater suicidal ideation and functional impairment in year 6. In summary, we show that mood instability represents a core phenotype of bipolar disorder with distinct predictors and long-term implications. Routine assessment may improve personalization in bipolar disorder treatment and research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data collected at the University of Michigan require a fully executed Data Use Agreement to be shared outside of the institution. Longitudinal and outcomes data used in the present study, along with data dictionaries, are available subject to review of the proposed analyses and acceptance of a Data Use Agreement. Enquiries can be addressed at https://medresearch.umich.edu/labs-departments/centers/prechter-program/research/longitudinal-study-bipolar-disorder/data-requests-repositories.
Code availability
All Mplus and R codes are provided on the Open Science Framework webpage: https://osf.io/3ms7b/.
References
Roshanaei-Moghaddam, B. & Katon, W. Premature mortality from general medical illnesses among persons with bipolar disorder: a review. Psychiatr. Serv. 60, 147–156 (2009).
Dilsaver, S. C. An estimate of the minimum economic burden of bipolar I and II disorders in the United States: 2009. J. Affect. Disord. 129, 79–83 (2011).
Yocum, A. K., Friedman, E., Bertram, H. S., Han, P. & McInnis, M. G. Comparative mortality risks in two independent bipolar cohorts. Psychiatry Res. 330, 115601 (2023).
Sperry, S. H., Yocum, A. K. & McInnis, M. G. Mood instability metrics to stratify individuals and measure outcomes in bipolar disorder. Nat. Ment. Health 2, 1111–1119 (2024).
Henry, C. et al. Affective lability and affect intensity as core dimensions of bipolar disorders during euthymic period. Psychiatry Res. 159, 1–6 (2008).
Stanislaus, S. et al. Mood instability in patients with newly diagnosed bipolar disorder, unaffected relatives, and healthy control individuals measured daily using smartphones. J. Affect. Disord. 271, 336–344 (2020).
Stapp, E. K. et al. Specificity of affective dynamics of bipolar and major depressive disorder. Brain Behav. 13, e3134 (2023).
Sperry, S. H. & Kwapil, T. R. Affective dynamics in bipolar spectrum psychopathology: modeling inertia, reactivity, variability, and instability in daily life. J. Affect. Disord. 251, 195–204 (2019).
Sperry, S. H. & Kwapil, T. R. Bipolar spectrum psychopathology is associated with altered emotion dynamics across multiple timescales. Emotion 22, 627 (2022).
Sperry, S. H., Walsh, M. A. & Kwapil, T. R. Emotion dynamics concurrently and prospectively predict mood psychopathology. J. Affect. Disord. 261, 67–75 (2020).
von Hofacker, A. J. et al. Predictors of mood and activity instability in participants with newly diagnosed bipolar disorder—exploratory findings from a prospective cohort study. J. Affect. Disord. Rep. 15, 100708 (2024).
Strejilevich, S. et al. Mood instability and functional recovery in bipolar disorders. Acta Psychiatr. Scand. 128, 194–202 (2013).
Gershon, A. & Eidelman, P. Inter-episode affective intensity and instability: predictors of depression and functional impairment in bipolar disorder. J. Behav. Ther. Exp. Psychiatry 46, 14–18 (2015).
Faurholt-Jepsen, M. et al. Is smartphone-based mood instability associated with stress, quality of life, and functioning in bipolar disorder? Bipolar Disord. 21, 611–620 (2019).
Barnett, J. et al. Personality and bipolar disorder: dissecting state and trait associations between mood and personality. Psychol. Med. 41, 1593–1604 (2011).
Ryan, K. A. et al. Predictive evidence for the impact of personality styles on depression and functioning in two bipolar disorder cohorts. J. Affect. Disord. 380, 746–755 (2025).
Faurholt-Jepsen, M. et al. Mood instability and activity/energy instability in patients with bipolar disorder according to day-to-day smartphone-based data—an exploratory post hoc study. J. Affect. Disord. 334, 83–91 (2023).
Kessing, L. V. & Faurholt-Jepsen, M. Mood instability—a new outcome measure in randomised trials of bipolar disorder? Eur. Neuropsychopharmacol. 58, 39–41 (2022).
Goldberg, J. F. et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am. J. Psychiatry 166, 173–181 (2009).
Watson, D., Ellickson-Larew, S., Stanton, K., Levin-Aspenson, H. F. & Khoo, S. Examining the criterion validity and diagnostic specificity of self-report measures of narcissism and mania. Assessment 28, 3–14 (2021).
Yocum, A. K. et al. Cohort profile update: the Heinz C. Prechter Longitudinal Study of Bipolar Disorder. Int. J. Epidemiol. 52, e324–e331 (2023).
McInnis, M. G. et al. Cohort profile: the Heinz C. Prechter Longitudinal Study of Bipolar Disorder. Int. J. Epidemiol. 47, 28–28n (2018).
Nurnberger, J. I. Jr. et al. Diagnostic Interview for Genetic Studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch. Gen. Psychiatry 51, 849–859 (1994).
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index—a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Roenneberg, T., Wirz-Justice, A. & Merrow, M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms 18, 80–90 (2003).
Bernstein, D. et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am. J. Psychiatry 151, 1132–1136 (1994).
Costa, P. T. & McCrae, R. R. Revised NEO-PI: Professional Manual (Psychological Assessment Resources, 1992).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Altman, E. G., Hedeker, D., Peterson, J. L. & Davis, J. M. The Altman Self-Rating Mania Scale. Biol. Psychiatry 42, 948–955 (1997).
Johns, M. W. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 14, 540–545 (1991).
Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., Monteiro, M. G. & World Health Organization. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care (World Health Organization, 2001).
Ware, J. E., Kosinski, M. & Keller, S. D. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care 34, 220–233 (1996).
Altshuler, L., Mintz, J. & Leight, K. The Life Functioning Questionnaire (LFQ): a brief, gender-neutral scale assessing functional outcome. Psychiatry Res. 112, 161–182 (2002).
McNeish, D. & Hamaker, E. L. A primer on two-level dynamic structural equation models for intensive longitudinal data in Mplus. Psychol. Methods 25, 610–635 (2020).
Hamaker, E. L., Asparouhov, T. & Muthén, B. in Handbook of Structural Equation Modeling (ed. Hoyle, R. H.) (Guilford Press, 2021).
Weller, B. E., Bowen, N. K. & Faubert, S. J. Latent class analysis: a guide to best practice. J. Black Psychol. 46, 287–311 (2020).
Acknowledgements
With gratitude, we acknowledge the Prechter Bipolar Longitudinal Research participants and thank the research team of the University of Michigan Prechter Bipolar Research Program for their contributions in the collection and stewardship of the data used in this publication. We acknowledge the funding for this study, including the Prechter Family Charitable Fund (to M.G.M.) and the Richard Tam Foundation (to M.G.M.). S.H.S. has grant-funded support for the present paper from a Brain and Behavior Foundation Young Investigator Award (number 30719; S.H.S.), a National Institute of Mental Health Loan Repayment Award (L30MH127613; S.H.S.) and a National Institute of Mental Health K23 Career Development Award (K23MH131601; S.H.S.). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the paper.
Author information
Authors and Affiliations
Contributions
A.R.S.: methodology, formal analysis and writing (original draft). A.K.Y.: methodology, software, validation, formal analysis, data curation, writing (original draft) and visualization. M.G.M.: conceptualization, resources, writing (review and editing), supervision and funding acquisition. I.F.T.: conceptualization, writing (review and editing) and supervision. S.H.S.: conceptualization, methodology, validation, formal analysis, data curation, writing (original draft), visualization, supervision, project administration and funding acquisition. A.R.S., A.K.Y. and S.H.S. all accessed the data, verified the data and replicated all results.
Corresponding author
Ethics declarations
Competing interests
A.R.S., A.K.Y., M.G.M. and I.F.T. have no competing interests to disclose. S.H.S. serves as an ad hoc consultant for Boehringer Ingelheim International GmbH.
Peer review
Peer review information
Nature Mental Health thanks Jess G. Fiedorowicz, Pedro Vieira Da Silva Magalhães and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–8, Figs. 1 and 2, Appendices 1–4, and Supplementary and Appendix References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stromberg, A.R., Yocum, A.K., McInnis, M.G. et al. Modeling and predicting mood instability in a longitudinal cohort of bipolar disorder. Nat. Mental Health 3, 1267–1275 (2025). https://doi.org/10.1038/s44220-025-00506-3
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-025-00506-3