Abstract
Objective:
To determine optimal timing of operation for repairing atonic bladder after medullary cone injury in rats.
Materials and methods:
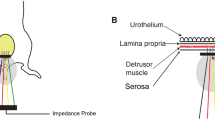
In all, 56 adult female Sprague–Dawley rats were equally randomized into seven groups: normal control group, and 4w, 6w, 8w, 10w, 12w and 16w groups after medullary cone injury, assigned as groups A–G. The model was established by sharp transaction of spinal cord at the level of L4/5 vertebral body. Bladder weight, cross-sectional area and ultrastructure of the detrusor muscle and its neuromuscular junction (NMJ), fibrotic change, and α-smooth muscle antibody (α-SMA) expression in the detrusor muscle were examined individually.
Results:
Bladder weight in groups E–G was significantly increased than that in group A (P<0.05). And cross-sectional area of detrusor muscle fiber in groups E–G was significantly smaller than that in group A (P<0.05). Transmission electronic microscopy showed that the number of synaptic vesicles, mitochondria and other organelles in NMJ decreased markedly in group E. In groups F and G, NMJ further degenerated with synaptic vesicles and organelles decreased or even disappeared. Masson's stain showed that the proportion of connective tissue in the detrusor muscle of groups E–G was significantly different from that of group A (P<0.05). α-SMA expression in the detrusor muscle decreased with the lapse of time.
Conclusions:
The 10th week after rat medullary cone injury can be regarded as the time node when the detrusor muscle and NMJ undergo changes, and therefore surgical nerve repair should be performed before this.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Benevento BT, Sipski ML . Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phys Ther 2002; 82: 601–612.
Dogan S, Safavi-Abbasi S, Theodore N, Chang SW, Horn EM, Mariwalla NR et al. Thoracolumbar and sacral spinal injuries in children and adolescents: a review of 89 cases. J Neurosurg 2007; 106: 426–433.
Heary RF, Salas S, Bono CM, Kumar S . Complication avoidance: thoracolumbar and lumbar burst fractures. Neurosurg Clin N Am 2006; 17: 377–388.
Blok BF, Karsenty G, Corcos J . Urological surveillance and management of patients with neurogenic bladder: results of a survey among practicing urologists in Canada. Can J Urol 2006; 13: 3239–3243.
Samson G, Cardenas DD . Neurogenic bladder in spinal cord injury. Phys Med Rehabil Clin N Am 2007; 18: 255–274, vi.
Chuang DC, Chang PL, Cheng SY . Root reconstruction for bladder reinnervation: an experimental study in rats. Microsurgery 1991; 12: 237–245.
Sundin T, Carlsson CA . Reconstruction of severed dorsal roots innervating the urinary bladder. An experimental study in cats. II. Regeneration studies. Scand J Urol Nephrol 1972; 6: 185–196.
Xiao CG, Godec CJ . A possible new reflex pathway for micturition after spinal cord injury. Paraplegia 1994; 32: 300–307.
Zhong G, Hou C, Wang S . Experimental study on the artificial bladder reflex arc established in therapy of flaccid bladder after spinal cord injury. Chinese Journal of Reparative and Reconstructive Surgery 2006; 20: 812–815.
Hou CL, Zhong GB, Xie QP, Wang SB . Establishing an artificial reflex arc restore controlled micturition of flaccid bladder after spinal cord injury: a preliminary report. Chin J Microsurg 2006; 29: 92–94.
Hiersemenzel LP, Curt A, Dietz V . From spinal shock to spasticity: neuronal adaptations to a spinal cord injury. Neurology 2000; 54: 1574–1582.
Storch JS . Lumbar burst fracture associated with bowel, bladder, and sexual dysfunction: case study. J Neurosci Nurs 2005; 37: 68–71.
Dahlberg A, Perttilä I, Wuokko E, Ala-Opas M . Bladder management in persons with spinal cord lesion. Spinal Cord 2004; 42: 694–698.
Hirsch NP . Neuromuscular junction in health and disease. Br J Anaesth 2007; 99: 132–138.
Kobayashi H, Yamataka A, Lane GJ, Miyano T . Disseminated mixed intestinal dysmotility (DMID): a new intestinal ganglion cell disorder? Pediatr Surg Int 2005; 21: 883–888.
Pirker ME, Rolle U, Shinkai T, Shinkai M, Puri P . Prenatal and postnatal neuromuscular development of the ureterovesical junction. J Urol 2007; 177: 1546–1551.
Burnstock G . Innervation of bladder and bowel. Ciba Found Symp 1990; 151: 2–18; discussion 18–26.
Fry CH, Hussain M, McCarthy C, Ikeda Y, Sui GP, Wu C . Recent advances in detrusor muscle function. Scand J Urol Nephrol Suppl 2004; 215: 20–25.
Hashitani H, Bramich NJ, Hirst GD . Mechanisms of excitatory neuromuscular transmission in the guinea-pig urinary bladder. J Physiol 2000; 524: 565–579.
Zashikhin AL . Development and ultrastructure of the neuromuscular junction in bronchial smooth muscle tissue. Arkh Anat Gistol Embriol 1989; 97: 80–85.
Acknowledgements
This work was supported by National Natural Science Foundation Of China (30672111), China Postdoctoral Science Foundation (20060390593) and Shanghai Postdoctoral Science Foundation (06R214102).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zheng, Xy., Hou, Cl., Chen, Am. et al. Optimal timing of operation for repairing atonic bladder after medullary cone injury: an experimental study in rats. Spinal Cord 46, 574–581 (2008). https://doi.org/10.1038/sc.2008.39
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2008.39
Keywords
This article is cited by
-
Laser-capture microdissection for analysis of cell type-specific gene expression of muscarinic receptor subtypes in the rat bladder with cyclophosphamide-induced cystitis
International Urology and Nephrology (2015)