Abstract
Study design:
Prospective multicenter longitudinal cohort study.
Objective:
To validate the prognostic value of the acute phase sacral sparing measurements with regard to chronic phase-independent ambulation in patients with traumatic spinal cord injury (SCI).
Setting:
European Multicenter Study of Human Spinal Cord Injury (EM-SCI).
Methods:
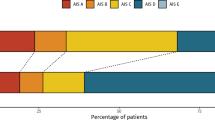
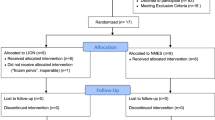
In 432 patients, acute phase (0–15 days) American Spinal Injury Association (ASIA)/International Spinal Cord Society neurological standard scale (AIS) grades, ASIA sacral sparing measurements, which are S4–5 light touch (LT), S4–5 pin prick (PP), anal sensation and voluntary anal contraction; and chronic phase (6 or 12 months) indoor mobility Spinal Cord Independence Measure (SCIM) measurements were analyzed. Calculations of positive and negative predictive values (PPV/NPV) as well as univariate and multivariate logistic regressions were performed in all four sacral sparing criteria. The area under the receiver-operating characteristic curve (AUC) ratios of all regression equations was calculated.
Results:
To achieve independent ambulation 1-year post injury, a normal S4–5 PP score showed the best PPV (96.5%, P<0.001, 95% confidence interval (95% CI): 87.9–99.6). Best NPV was reported in the S4–5 LT score (91.7%, P<0.001, 95% CI: 81.6–97.2). The use of the combination of only voluntary anal contraction and the S4–5 LT and PP sensory scores (AUC: 0.906, P<0.001, 95% CI: 0.871–0.941) showed significantly better (P<0.001, 95% CI: 0.038–0.128) discriminating results in prognosticating 1-year independent ambulation than with the use of currently used distinction between complete and incomplete SCI (AUC: 0.823, P<0.001, 95% CI: 0.781–0.864).
Conclusions:
Out of the four sacral sparing criteria, the acute phase anal sensory score measurements do not contribute significantly to the prognosis of independent ambulation. The combination of the acute phase voluntary anal contraction and the S4–5 LT and PP scores, predicts significantly better chronic phase-independent ambulation outcomes than the currently used distinction between complete and incomplete SCI.
Sponsorship:
This study was granted by ‘Acute Zorgregio Oost’ and the ‘Internationale Stiftung für Forschung in Paraplegie (IFP)’.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury, revised 2003. American Spinal Injury Association: Chicago, IL, 2003.
American Spinal Injury Association. Standards for Neurological Classification of Spinal Injured Patients. American Spinal Injury Association: Chicago, IL, 1982.
Kirshblum SC, Memmo P, Kim N, Campagnolo D, Millis S . Comparison of the revised 2000 American Spinal Injury Association classification standards with the 1996 guidelines. Am J Phys Med Rehabil 2002; 81: 502–505.
Waters RL, Adkins RH, Yakura JS . Definition of complete spinal cord injury. Paraplegia 1991; 29 : 573–581.
American Spinal Injury Association. Standards for Neurological Classification of SCI Worksheet, Revised 2006, Accessed: May 2008. Available from URL: http://www.asia-spinalinjury.org/publications/2006_Classif_worksheet.pdf.
American Spinal Injury Association/International Medical Society of Paraplegia (ASIA/IMSOP). International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients (Revised). American Spinal Injury Association: Chicago, IL, 1992.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007; 45: 190–205.
Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord 2007; 45: 206–221.
Waters RL, Adkins RH, Yakura JS, Sie I . Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil 1993; 74: 242–247.
Marino RJ, Ditunno Jr JF, Donovan WH, Maynard Jr F . Neurologic recovery after traumatic spinal cord injury: data from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil 1999; 80: 1391–1396.
Waters RL, Adkins R, Yakura J, Vigil D . Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil 1994; 75: 756–760.
Oleson CV, Burns AS, Ditunno JF, Geisler FH, Coleman WP . Prognostic value of pinprick preservation in motor complete, sensory incomplete spinal cord injury. Arch Phys Med Rehabil 2005; 86: 988–992.
Ditunno Jr JF, Burns AS, Marino RJ . Neurological and functional capacity outcome measures: essential to spinal cord injury clinical trials. J Rehabil Res Dev 2005; 42 (3 Suppl 1): 35–41.
Ditunno PL, Patrick M, Stineman M, Ditunno JF . Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord 2008; 46: 500–506.
Granger CV, Hamilton BB, Keith RA, Zielesny M, Sherwin FS . Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil 1986; 1: 59–74.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Dittuno PL, Dittuno Jr JF . Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord 2001; 39: 654–656.
Lam T, Noonan VK, Eng JJ . A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 2008; 46: 246–254.
Kirshblum SC, Priebe MM, Ho CH, Scelza WM, Chiodo AE, Wuermser LA . Spinal cord injury medicine. 3. Rehabilitation phase after acute spinal cord injury. Arch Phys Med Rehabil 2007; 88 (3 Suppl 1): S62–S70.
Kirshblum SC, O'Connor KC . Predicting neurologic recovery in traumatic cervical spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1456–1466.
Burns AS, Ditunno JF . Establishing prognosis and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine 2001; 26 (24 Suppl): S137–S145.
Hanley JA, McNeil BJ . The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982; 143 : 29–36.
Hosmer DW, Lemeshow S (eds). Applied Logistic Regression, 2nd edn. John Wiley & Sons: New York, USA, 2000, pp 47–69.
Hanley JA, McNeil BJ . A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983; 148: 839–843.
Stauffer ES . Diagnosis and prognosis of acute cervical spinal cord injury. Clin Orthop Relat Res 1975; 112: 9–15.
Greving I, Tegenthoff M, Nedjat S, Orth G, Botel U, Meister V et al. Anorectal functions in patients with spinal cord injury. Neurogastroenterol Motil 1998; 10: 509–515.
Wietek BM, Baron CH, Erb M, Hinninghofen H, Badtke A, Kaps HP et al. Cortical processing of residual ano-rectal sensation in patients with spinal cord injury: an fMRI study. Neurogastroenterol Motil 2008; 20: 488–497.
Neumann S, Woolf CJ . Regeneration of dorsal column fibers into and beyond the lesion site following adult spinal cord injury. Neuron 1999; 23: 83–91.
Blaustein DM, Zafonte R, Thomas D, Herbison GJ, Ditunno JF . Predicting recovery of motor complete quadriplegic patients. 24 hour v 72 hour motor index scores. Am J Phys Med Rehabil 1993; 72: 306–311.
Brown PJ, Marino RJ, Herbison GJ, Ditunno Jr JF . The 72-h examination as a predictor of recovery in motor complete quadriplegia. Arch Phys Med Rehabil 1991; 72: 546–548.
Savic G, Bergstrom EM, Frankel HL, Jamous MA, Jones PW . Inter-rater reliability of motor and sensory examinations performed according to American Spinal Injury Association standards. Spinal Cord 2007; 45: 444–451.
Acknowledgements
We thank all the members of the European Multicenter Study of Human Spinal Cord Injury (EM-SCI), especially Mrs. Henny Janssen, Christian Schuld and René Koller for their assistance in data collection and data processing. We acknowledge dr. Rogier Donders for his time and expertise with the statistical analyses.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
van Middendorp, J., Hosman, A., Pouw, M. et al. Is determination between complete and incomplete traumatic spinal cord injury clinically relevant? Validation of the ASIA sacral sparing criteria in a prospective cohort of 432 patients. Spinal Cord 47, 809–816 (2009). https://doi.org/10.1038/sc.2009.44
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2009.44
Keywords
This article is cited by
-
Guidelines for neuroprognostication in adults with traumatic spinal cord injury
Neurocritical Care (2024)
-
Testing sensation of gently squeezing the testes has diagnostic value in spinal cord injury men
Spinal Cord Series and Cases (2021)
-
Daily acute intermittent hypoxia to improve walking function in persons with subacute spinal cord injury: a randomized clinical trial study protocol
BMC Neurology (2020)
-
An interview based approach to the anorectal portion of the International Standards of Neurological Classification of Spinal Cord Injury Exam (I-A-ISNCSCI): a pilot study
Spinal Cord (2020)
-
The Effect of Non-Gabapentinoid Anticonvulsants on Sensorimotor Recovery After Human Spinal Cord Injury
CNS Drugs (2019)