Abstract
Study design:
Retrospective review study.
Objectives:
To identify whether it is safe to perform a magnetic resonance imaging (MRI) exam on patients who have a sacral anterior root stimulator (SARS).
Setting:
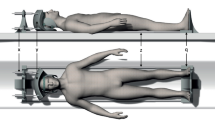
Adult patients with spinal cord injury and implanted SARS attending the National Spinal Injuries Centre who have had MRI scans.
Methods:
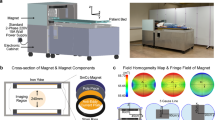
Retrospective review between 1989 and 2010. The effect of the MRI scans on the function of the SARS (Finetech-Brindley, UK) was assessed up to 6 months following MRI at 0.2 and 1.5 T.
Results:
A total of 18 patients with SARS implants had MRI scans at 0.2 and 1.5 T of the cervical, thoracic and lumbar spine, head, shoulder and pelvis. MRI examinations were abandoned on two occasions in one patient due to radiofrequency interference. One patient's stimulator ceased to function 5 months following MRI; both of these patients showing complications had their MRI examinations at 0.2 T. There were no adverse effects at 1.5 T. In one patient the SARS was removed within 6 months after MRI due to an unrelated medical condition. A total of 17 patients showed no symptoms that required terminating the examination. In all the 11 patients with a complete and functioning implant before MRI at 1.5 T, the SARS was functioning appropriately, and no change in bladder function was reported up to 6 months following MRI.
Conclusion:
It is safe to perform an MRI scan on patients with SARS providing the examination is conducted in a 1.5 T system.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Brindley GS . History of the sacral anterior root stimulator, 1969–1982. Neurourol Urodyn 1993; 12: 481–483.
Brindley GS . The sacral anterior root stimulator as a means of managing the bladder in patients with spinal cord lesions. Baillieres Clin Neurol 1995; 4: 1–13.
Brindley GS . The first 500 patients with sacral anterior root stimulator implants: general description. Paraplegia 1994; 32: 795–805.
Ruan CM, Escobedo E, Harrison S, Goldstein B . Magnetic resonance imaging of nonhealing pressure ulcers and myocutaneous flaps. Arch Phys Med Rehabil 1998; 79: 1080–1088.
Wick L, Berger M, Knecht H, Glucker T, Ledermann HP . Magnetic resonance signal alterations in the acute onset of heterotopic ossification in patients with spinal cord injury. Eur Radiol 2005; 15: 1867–1875.
Planner AC, Pretorius PM, Graham A, Meagher TM . Subacute progressive ascending myelopathy following spinal cord injury: MRI appearances and clinical presentation. Spinal Cord 2008; 46: 140–144.
Loewy J, Loewy A, Kendall EJ . Reconsideration of pacemakers and MR imaging. Radiographics 2004; 24: 1257–1267.
Gimbel JR, Johnson D, Levine PA, Wilkoff BL . Safe performance of magnetic resonance imaging on five patients with permanent cardiac pacemakers. Pacing Clin Electrophysiol 1996; 19: 913–919.
Martin ET, Coman JA, Shellock FG, Pulling CC, Fair R, Jenkins K . Magnetic resonance imaging and cardiac pacemaker safety at 1.5-Tesla. J Am Coll Cardiol 2004; 43: 1315–1324.
Elkelini MS, Hassouna MM . Safety of MRI at 1.5Tesla in patients with implanted sacral nerve neurostimulator. Eur Urol 2006; 50: 311–316.
Shellock FG . Vocare bladder system, implantable functional neuromuscular stimulation. In: Reference Manual for Magnetic Resonance Safety, Implants, and Devices: 2007 EDITION, 3rd edn. Biomedical Research Publishing Company: Los Angeles, CA, 2007, pp 311–315.
Fine Tech Medical Ltd,. MRI Guidance Instruction for FineTech-Brindley Bladder Stimulator. In: Document Reference: TF1-BS-402, 2008 (http://www.finetech-medical.co.uk/LinkClick.aspx?fileticket=s%2bs1cG57Z4k%3d&tabid=95&language=en-GB).
Ng K-H, Faust O, Acharya UR . Health effects and safety of magnetic resonance imaging. J Med Syst 2010 (doi: 10.1007/s10916-010-9460-9).
Baker KB, Nyenhuis JA, Hrdlicka G, Rezai AR, Tkach JA, Shellock FG . Neurostimulation systems: assessment of magnetic field interactions associated with 1.5- and 3-Tesla MR systems. J Magn Reson Imaging 2005; 21: 72–77.
Luechinger R, Duru F, Scheidegger MB, Boesiger P, Candinas R . Force and torque effects of a 1.5-Tesla MRI scanner on cardiac pacemakers and ICDs. Pacing Clin Electrophysiol 2001; 24: 199–205.
Roguin A, Zviman MM, Meininger GR, Rodrigues ER, Dickfeld TM, Bluemke DA et al. Modern pacemaker and implantable cardioverter/defibrillator systems can be magnetic resonance imaging safe: in vitro and in vivo assessment of safety and function at 1.5T. Circulation 2004; 110: 475–482.
Sommer T, Vahlhaus C, Lauck G, von SA, Reinke M, Hofer U et al. MR imaging and cardiac pacemakers: in-vitro evaluation and in-vivo studies in 51 patients at 0.5T. Radiology 2000; 215: 869–879.
Duru F, Luechinger R, Candinas R . MR imaging in patients with cardiac pacemakers. Radiology 2001; 219: 856–858.
Tronnier VM, Staubert A, Hahnel S, Sarem-Aslani A . Magnetic resonance imaging with implanted neurostimulators: an in vitro and in vivo study. Neurosurgery 1999; 44: 118–125.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
de Heredia, L., Meagher, T., Jamous, M. et al. Long-term effect of MRI on sacral anterior root stimulator: the Stoke Mandeville experience. Spinal Cord 50, 294–297 (2012). https://doi.org/10.1038/sc.2011.135
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2011.135
Keywords
This article is cited by
-
Neuromodulation for Neurogenic Bladder
Current Bladder Dysfunction Reports (2013)