Abstract
Background:
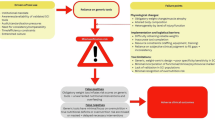
Data on the prevalence of malnutrition in paediatric patients with spinal cord injury (SCI) are limited. The present study aimed to establish the risk of (i) under-nutrition by using the Screening Tool for Assessment of Malnutrition in Paediatrics: STAMP (score ⩾2) and (ii) over-nutrition by body mass index (BMI) centile (⩾91st: overweight; ⩾98th: obese).
Methods:
After obtaining informed consent, a standardized questionnaire was used to collect baseline demographic data and nutrition risk score; BMI was measured and routine blood biochemistry was reviewed in every child (>6 months and <18 years) admitted to the SCI centre.
Results:
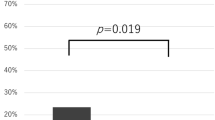
Sixty-two children (mean age, 11.4 years; s.d., 4.9; median, 13 years; interquartile range, 7.8–15.6, 39.4% female) with SCI (46.5% tetraplegia, 53.4% complete SCI) were assessed. Prevalence of over-nutrition was high (BMI centile ⩾91st, 41.1%; ⩾98th, 25.5%). Under-nutrition risk was 47.1% (STAMP ⩾2). Only 60% of these ‘at risk’ patients were referred for further nutritional assessment. Associated phenomena included previous intensive care (55.6 versus 20.8%, P<0.05), mechanical ventilation (58.3 versus 18.2%, P<0.01) and past need for artificial nutrition support (75 versus 12.8%, P<0.01).
Conclusions:
Both over- and under-nutrition appear common in children with SCI. Our data indicate, furthermore, that children at nutritional risk are under-managed. Future research is needed to complete the validation of the screening tools and to determine how effective intervention can be ensured.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
American Dietetic Association. Spinal cord Injury (SCI) evidence-based nutrition practice guideline. 2009. www.adaevidencelibrary.com. assessed April 2010.
Brotherton A, Simmonds N, Stroud M . Malnutrition Matters: Meeting Quality Standards in Nutritional Care. BAPEN: Redditch, 2010. http://www.bapen.org.uk/pdfs/bapen_pubs/mm-toolkit-exec-summary.pdf; accessed 19.08.2011.
Schneider SM, Veyers P, Pivot X, Soummer A, Jambou P, Filippi J et al. Malnutrition is an independent factor associated with nosocomial infections. Br J Nutr 2004; 92: 105–111.
National Institute for Health and Clinical Excellence (NICE). The Management of Pressure Ulcers in Primary and Secondary Care: a Clinical Practice Guideline. NICE: London, 2005.
National Institute for Health and Clinical Excellence (NICE). Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. NICE: London, 2006. http://www.nice.org.uk/nicemedia/live/11000/30365/30365.pdf; accessed 19.08.2011.
National Institute for Health and Clinical Excellence (NICE). Nutrition Support in Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. NICE: London, 2006. http://www.nice.org.uk/nicemedia/live/10978/29981/29981.pdf; accessed 19.08.2011.
Pelletier DL, Frongillo Jr EA, Habicht JP . Epidemiological evidence for a potentiating effect of malnutrition on child mortality. Am J Public Health 1993; 83: 1130–1133.
World Health Organization (WHO). WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: a Joint Statement by the World Health Organization and the United Nations Children's Fund 2009. http://www.who.int/nutrition/publications/severemalnutrition/9789241598163_eng.pdf; accessed 7.May.2011.
Seid RO, Nusser-Muller-Busch R, Kurzweil M, Niedeggen A . Dysphagia in acute tetraplegics: a retrospective study. Spinal Cord 2010; 48: 197–201.
Kirshbkum S, Johnston MV, Brown J, O’Connor KC, Jarosz P . Predictors of dysphagia after spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1101–1105.
Cheshire DJE, Coats DA . Respiratory and metabolic management in acute tetraplegia. Paraplegia 1966; 4: 1–23.
Buchholz AC, Pencharz PB . Energy expenditure in chronic spinal cord injury. Curr Opin Clin Nutr Metab Care 2004; 7: 635–639.
Wong SS, Derry F, Sherrington K, Gerogery G . An audit to evaluate the use of nutrition screening tool in the National Spinal Injury Centre, Stoke Mandeville Hospital, Buckinghamshire Hospitals NHS Trust. Proc Nutr Soc 2009; 68: E53.
Sermet-Gaudelus I, Poisson-Salmon AS, Colomb V, Brusset MC, Mosser F, Berrier F et al. Simple pediatric nutritional risk score to identify children at risk of malnutrition. Am J Clin Nutr 2000; 72: 64–70.
Secker DJ, Jeejeebhoy KN . Subjective global nutritional assessment for children. Am J Clin Nutr 2007; 85: 1083–1089.
Hulst JM, Zwart H, Hop W, Joosten KF . Dutch national survey to test the STRONGkids nutritional risk screening tool in hospitalized children. Clinl Nutr 2010; 29: 106–111.
McCarthy H, McNulty H, Dixon M, Eaton-Evans MJ . Screening for nutritional risk in children: the validation of a new tool. J Hum Nutr Diet 2008; 21: 395–396. www.stampscreeningtool.org accessed 19.08.2011.
Rasmussen HH, Kondrup J, Staun M, Ladefoged K, Kristensen H, Wengler A . A prevalence of patients at nutritional risk in Danish hospitals. Clin Nutr 2004; 23: 1009–1015.
Joosten KFM, Hulst JM . Prevalence of malnutrition in paediatric hospital patients. Curr Opin Pediatr 2008; 20: 590–596.
Government Office for Science. Foresight: Tackling Obesities: Future Choices—Project Report. HMSO: London, 2007.
Acknowledgements
We thank the patients and ward staff of St Francis ward, Ebba Bergstrom and Kirsten Hart for height estimation, and Pauline Bateman from Medical Records at the National Spinal Injuries Centre at Stoke Mandeville Hospital. We also thank Dr Joan Gandy (The British Dietetic Association) and Professor John Reilly (University of Glasgow) for protocol development.
Author contributions: SW: Protocol development, data collection, data analysis and manuscript preparation. AG: Protocol development, clinical supervision and manuscript revision. SH: Statistical supervision and manuscript revision. GG: Academic supervision and manuscript revision. AF: Academic supervision and manuscript revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
This study was funded by unrestricted educational grants from the Waterloo Foundation and Abbott Nutrition (Abbott Laboratories Ltd). The University College London (UCL) staff receive support from the Comprehensive Biomedical Research Centre funding awarded to UCL and its partner Trust by National Institute for Health and Research.
Rights and permissions
About this article
Cite this article
Wong, S., Graham, A., Harini, S. et al. Profile and prevalence of malnutrition in children with spinal cord injuries—assessment of the Screening Tool for Assessment of Malnutrition in Paediatrics (STAMP). Spinal Cord 50, 67–71 (2012). https://doi.org/10.1038/sc.2011.139
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2011.139
Keywords
This article is cited by
-
Risks of undernutrition and malnutrition in hospitalized pediatric patients with spinal cord injury
Spinal Cord (2017)
-
Is undernutrition risk associated with an adverse clinical outcome in spinal cord-injured patients admitted to a spinal centre?
European Journal of Clinical Nutrition (2014)
-
Validation of the Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP) in patients with spinal cord injuries (SCIs)
Spinal Cord (2013)