Abstract
Study design:
Cohort study.
Objectives:
The objective of this study is to assess depression over a 5-year period in persons with spinal cord injury (SCI) and to assess risk factors for depression over time.
Setting:
Rehabilitation hospitals in the Southeast and Midwest.
Methods:
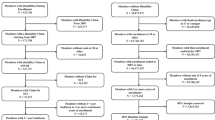
Participants included 801 adults with residual effects from a traumatic SCI averaging over 15 years post injury. Participants responded to two questionnaires, one in 2002 (Time1) and another in 2008 (Time 2). Probable major depression (PMD) was measured by the Older Adult Health and Mood Questionnaire.
Results:
In all, 22.1% of participants had PMD at Time 1 and 20.2% at Time 2. There was a non-significant trend for change in PMD status (P=0.058). Of those who had PMD at Time 1, 55.7% had PMD at Time 2. Between the two time points, the most change occurred in the group with clinically significant symptomatology. Demographic factors (race–gender, age, time since injury) and health behaviors (pain medication use, hours out of bed, days out of the house, exercise) were significantly associated with PMD over time. Socioeconomic factors (income, education) were significantly related to depression but were not significant after controlling for behavioral factors.
Conclusion:
Depression is fairly consistent over time in persons with SCI, with the majority of change coming from those in the clinically significant symptomatology group. Examining depression at multiple time points, our results underscore the importance of health behaviors in relation to PMD, even after controlling for demographic, injury and environmental factors.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Elliott TR, Frank RG . Depression following spinal cord injury. Arch Phys Med Rehabil 1996; 77: 816–823.
Frank RG, Chaney JM, Clay DL, Shutty MS, Beck NC, Kay DR et al. Dysphoria: a major symptom factor in persons with disability or chronic illness. Psych Res 1992; 43: 231–241.
Fuhrer MJ, Rintala DH, Hart KA, Clearman R, Young ME . Depressive symptomatology in persons with spinal cord injury who reside in the community. Arch Phys Med Rehabil 1993; 74: 255–260.
Northwest regional SCI system. Depression and spinal cord injury. Retrieved on 12 January 2011 from http://sci.washington.edu/info/pamphlets/depression_sci.asp.
Krause JS, Kemp B, Coker JL . Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil 2000; 81: 1099–1109.
Craig A, Tran Y, Middleton J . Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009; 47: 108–114.
Kroenke K, Spitzer RL, Williams JB . The PHQ-9: validity of a brief depression severity measure. J Gen Int Med 2001; 16: 606–613.
NSCISC. Annual Statistical Report. University of Alabama: Birmingham, AL, 2009.
Krause JS, Saladin LK, Adkins RH . Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. NeuroRehabilition 2009; 24: 47–56.
Kennedy P, Rogers BA . Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000; 81: 932–937.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from one to five years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Dorsett P, Geraghty T . Depression and adjustment after spinal cord injury: a three-year longitudinal study. Top Spinal Cord Inj Rehabil 2004; 9: 43–56.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from one to five years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Kemp BJ, Adams BM . The Older Adult Health and Mood Questionnaire: a measure of geriatric depressive disorder. J Ger Psych Neuro 1995; 8: 162–167.
Taylor G . Predicted Versus Actual Response to Spinal Cord Injury: A Psychological Study 1967.
Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN . . Craig Hospital: Englewood, CO, 1992.
Liang KY, Zeger SL . Longitudinal data analysis using generalized linear models. Biometrika 1986; 73: 13–22.
Krause JS . Secondary conditions and spinal cord injury: a model for prediction and prevention. Top Spinal Cord Inj Rehabil 1996; 2: 217–227.
Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG . Symptoms of major depression in people with spinal cord injury: implications for screening. Arch Phys Med Rehabil 2004; 85: 1749–1756.
National Institute of Mental Health. The Numbers Count: Mental Disorders in America. Retrieved on 12 January 2011 from http://www.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america/index.shtml.
Mitchell J, Adkins R . Five-year changes in self-rated health and associated factors for people with aging with versus without spinal cord injury. Top Spinal Cord Inj Rehabil 2010; 15: 21–33.
Hasin DS, Goodwin RD, Stinson FS, Grant BF . Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry 2005; 62: 1097–1106.
Krause JS, Broderick LE . Outcomes after spinal cord injury: comparisons as a function of gender and race and ethnicity. Arch Phys Med Rehabil 2004; 85: 355–362.
Migliorini CE, New PW, Tonge BJ . Comparison of depression, anxiety and stress in persons with traumatic and non-traumatic post-acute spinal cord injury. Spinal Cord 2009; 47: 783–788.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Krause JS, Coker J, Charlifue S, Whiteneck G . Depression and subjective well-being among 97 American Indians with spinal cord injury: a descriptive study. Rehabil Psychol 1999; 44: 354–372.
Acknowledgements
The contents of the publication were developed under a grant from the Department of Education, NIDRR Grant numbers H133G020239, H133G060126 and H133B090005. (However, those contents do not necessarily represent the policy of the Department of Education, and one should not assume endorsement by the Federal Government.)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saunders, L., Krause, J. & Focht, K. A longitudinal study of depression in survivors of spinal cord injury. Spinal Cord 50, 72–77 (2012). https://doi.org/10.1038/sc.2011.83
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2011.83
Keywords
This article is cited by
-
Psychological distress 12 years following injury in New Zealand: findings from the Prospective Outcomes of Injury Study-10 years on (POIS-10)
Injury Epidemiology (2023)
-
Relationships between cardiovascular disease risk, neuropathic pain, mental health, and autonomic function in chronic spinal cord injury
Spinal Cord (2023)
-
Greener on the other side? an analysis of the association between residential greenspace and psychological well-being among people living with spinal cord injury in the United States
Spinal Cord (2022)
-
Autonomic variability, depression and the disability paradox in spinal cord injury
Spinal Cord Series and Cases (2022)
-
Clinical and demographic predictors of symptoms of depression and anxiety in patients with spinal cord injury
Spinal Cord (2022)