Abstract
Study design:
Survey.
Objectives:
To describe and compare perceived barriers with patient flow in spinal rehabilitation units (SRUs).
Setting:
International. Ten SRUs (Australia, Canada, India, Ireland, Italy, Netherlands, Pakistan, Switzerland, UK and USA) that admit both traumatic and non-traumatic spinal cord injury patients.
Methods:
Survey completed between December 2010 and February 2013 on perception of barriers for admission into and discharge from SRUs. Opinion was sought from the participants regarding the utility of collecting data on the timeliness of access to SRUs and occurrence of discharge barriers for benchmarking and quality improvement purposes.
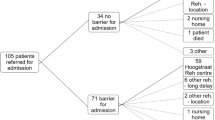
Results:
The perceived barriers in accessing SRUs ranged from no access problem to a severe access problem (no access problems n=3; minor access problems n=3; moderate access problems n=2; severe access problem n=1 and extreme n=1). Most units (n=9/10) agreed that collecting data on timeliness of access to SRUs for acute hospital patients may help improve patient outcomes and health system processes by providing information for benchmarking and quality improvement purposes. All units reported perceived barriers to discharge from SRUs. Compared with admission barriers, a greater perception of barriers to discharge was reported (minor problem n=3; moderate problem n=3; severe problem n=3; and extreme n=1). All units agreed that collecting data on barriers to discharge from SRU may help improve patient outcomes and system processes.
Conclusions:
Perceived barriers to patient flow in SRUs are reported in many countries. Projects to identify and minimise the occurrence and impact of admission and discharge barriers could increase access to rehabilitation and improve the rehabilitation outcomes for patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Trzeciak S, Rivers EP . Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J 2003; 20: 402–405.
Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2009; 16: 1–10.
Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM . Improving service quality by understanding emergency department flow: a White Paper and Position Statement prepared for the American Academy of Emergency Medicine. J Emerg Med 2010; 38: 70–79.
Weaver FM, Guihan M, Hynes DM, Byck G, Conrad KJ, Demakis JG . Prevalence of subacute patients in acute care: results of a study of VA hospitals. J Med Syst 1998; 22: 161–172.
Flintoft VF, Williams Jl, Williams RC, Basinski AS, Blackstien-Hirsch P, Naylor CD . The need for acute, subacute and nonacute care at 105 general hospital sites in Ontario. CMAJ 1998; 158: 1289–1296.
Carey MR, Sheth H, Braithwaite RS . A prospective study of reasons for prolonged hospitalizations on a general medical teaching service. J Gen Intern Med 2005; 20: 108–115.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S et al. An Italian survey of traumatic spinal cord injury. The gruppo Italiano studio epidemiologico mielolesioni study. Arch Phys Med Rehabil 2003; 84: 1266–1275.
Amin A, J B, Najarajah R, Davies N, Gow F, Tucker S . Spinal injuries admitted to a specialist centre over a 5-year period: a study to evaluate delayed admission. Spinal Cord 2005; 43: 434–437.
Bradley LJ, Kirker SG, Corteen E, Seeley HM, Pickard JD, Hutchinson PJ . Inappropriate acute neurosurgical bed occupancy and short falls in rehabilitation: implications for the National Service Framework. Br J Neurosurg 2006; 20: 36–39.
New PW, Poulos CJ . Functional improvement of the Australian health care system — can rehabilitation assist? Med J Aust 2008; 189: 340–343.
New PW, Cameron PA, Olver JH, Stoelwinder JU . Key stakeholders’ perception of barriers to admission and discharge from inpatient subacute care in Australia. Med J Aust 2011; 195: 538–541.
Smith M . Efficacy of specialist versus non-specialist management of spinal cord injury within the UK. Spinal Cord 2002; 40: 11–16.
New PW . Non-traumatic spinal cord injury: what is the ideal setting for rehabilitation? Aust Health Rev 2006; 30: 353–361.
New PW, Simmonds F, Stevermuer T . Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord 2011; 49: 909–916.
New PW, Townson A, Scivoletto G, Post MWM, Eriks-Hoogland I, Gupta A et al. International comparison of the organisation of rehabilitation services and systems of care for patients with spinal cord injury. Spinal Cord 2013; 51: 33–39.
Anzai K, Young J, McCallum J, Miller B, Jongbloed L . Factors influencing discharge location following high lesion spinal cord injury rehabilitation in British Columbia, Canada. Spinal Cord 2006; 44: 11–18.
Dobrez D, Heinemann AW, Deutsch A, Manheim L, Mallinson T . Impact of Medicare’s prospective payment system for inpatient rehabilitation facilities on stroke patient outcomes. Am J Phys Med Rehabil 2010; 89: 198–204.
Pezzin LE, Roberts BA, Miao H, Dillingham TR . Regulatory policies, the ‘‘75% rule,’’ and post-acute care discharge setting. Am J Phys Med Rehabil 2011; 90: 954–958.
Post MWM, van Asbeck FWA, van Dijk AJ, Schrijvers AJP . Services for spinal cord injured: availability and satisfaction. Spinal Cord 1997; 35: 109–115.
Silver J, Ljungberg I, Libin A, Groah S . Barriers for individuals with spinal cord injury returning to the community: a preliminary classification. Disabil Health J 2012; 5: 190–196.
Andrews LB, Stocking C, Krizek L, Gottlieb L, Krizek C, Vargish T et al. An alternative strategy for studying adverse events in medical care. Lancet 1997; 349: 309–313.
Maulden SA, Gassaway J, Horn SD, Smout RJ, DeJong G . Timing of initiation of rehabilitation after stroke. Arch Phys Med Rehabil 2005; 86 (Suppl 2): S34–S40.
Sirois M, Lavoie A, Dionne C . Impact of transfer delays to rehabilitation in patients with severe trauma. Arch Phys Med Rehabil 2004; 85: 184–191.
Aung TS, El Masry WS . Audit of a British centre for spinal injury. Spinal Cord 1997; 35: 147–150.
Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R . Early rehabilitation effects for traumatic spinal cord injury. Arch Phys Med Rehabil 2001; 82: 391–395.
Scivoletto G, Morganti B, Molinari M . Early versus delayed inpatient spinal cord injury rehabilitation: An Italian study. Arch Phys Med Rehabil 2005; 86: 512–516.
New PW, Cameron PA, Olver JH, Stoelwinder JU . Defining barriers to discharge from inpatient rehabilitation, classifying their causes, and proposed performance indicators for rehabilitation patient flow. Arch Phys Med Rehabil 2013; 94: 201–208.
Atkins D, Noonan VK, Santos A, Lewis R, Fehlings M, Burns A et al. Secondary complications in SCI across the continuum: using operations research to predict the impact and optimize management strategies. Top Spinal Cord Inj Rehabil 2012; 1: 57–66.
Noonan VK, Soril L, Atkins D, Lewis R, Santos A, Fehlings MG et al. The application of operations research methodoligies to the delivery of care model for traumatic spinal cord injury: the access to care and timing (ACT) project. J Neurotrauma 2012; 29: 2272–2282.
Acknowledgements
For assisting in refining the pilot version of the survey, we thank Michele New; Associate Professor Christopher J Poulos, Hammond Chair of Positive Ageing and Care, University of New South Wales, Australia; Dr Richard Bignell; Associate Professor Fary Kahn, Principal Fellow, Department of Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia; and Dr Hean See Tan, Rehabilitation and Aged Services, Medicine Program, Kingston Centre, Southern Health, Victoria, Australia. The following people are thanked for their assistance with facilitating the data collection: Bianca Fedele (Caulfield Hospital, Australia), Michael Baumberger (Swiss Paraplegic Center, Switzerland), Joost van Middendorp and Salman Lari (National Spinal Injuries Centre, Stoke Mandeville Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
New, P., Scivoletto, G., Smith, É. et al. International survey of perceived barriers to admission and discharge from spinal cord injury rehabilitation units. Spinal Cord 51, 893–897 (2013). https://doi.org/10.1038/sc.2013.69
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2013.69
Keywords
This article is cited by
-
Unmet healthcare needs and health inequalities in people with spinal cord injury: a direct regression inequality decomposition
International Journal for Equity in Health (2023)
-
Challenges and potential improvements in the admission process of patients with spinal cord injury in a specialized rehabilitation clinic – an interview based qualitative study of an interdisciplinary team
BMC Health Services Research (2017)
-
Understanding the Role of Rehabilitation Medicine in the Care of Patients with Tumor Causing Spinal Cord Dysfunction
Current Physical Medicine and Rehabilitation Reports (2017)
-
Time-series analysis of the barriers for admission into a spinal rehabilitation unit
Spinal Cord (2016)
-
Developing human rights based indicators to support country monitoring of rehabilitation services and programmes for people with disabilities: a study protocol
BMC International Health and Human Rights (2015)