Abstract
Study design:
A retrospective comparative study.
Objectives:
To compare clinical outcomes of surgery or non-operated treatment for mild cervical spondylotic myelopathy (CSM) patients with intramedullary increased signal intensity (ISI) on T2-weighted imaging (T2WI) of magnetic resonance imaging (MRI), related factors that may affect prognosis were explored.
Methods:
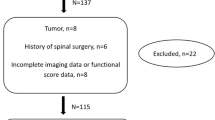
Data from 91 patients treated from July 2008 to June 2011 were retrospectively analyzed. The Japanese Orthopedic Association (JOA) recovery ratio was used to compare outcomes of surgery and non-operated treatment. Correlation and multiple linear regression analyses were performed between JOA recovery ratio and age, disease course, segmental lordosis, total range of motion (ROM), segmental ROM, local slip, extent of spinal cord compression or ISI type.
Results:
Patients were divided into two groups by therapy methods: Group A (n=53, 33 males, age 36–68 years) underwent anterior cervical decompression and fusion surgery, average follow-up 30.68±8.19 months; Group B (n=38, 14 males, age 28–76 years) received non-operated treatment, average follow-up 34.08±9.05 months. There were no significant differences in clinical outcomes between the two groups. There were significant correlations between JOA recovery ratio and clinical course (P<0.01) or segmental lordosis (P<0.01). Patients with shorter disease course and larger segmental lordosis have better clinical outcomes as shown by multiple linear regression analysis.
Conclusion:
For mild CSM patients with ISI on T2WI-MRI, there are no significant differences in clinical outcome between surgery and non-operated treatment during the short-term follow-up. Patients with shorter disease course and larger segmental lordosis have better clinical outcomes than those with longer course and segmental kyphosis.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tracy JA, Bartleson JD . Cervical spondylotic myelopathy. Neurologist 2010; 16: 176–187.
Takahashi M, Yamashita Y, Sakamoto Y, Kojima R . Chronic cervical cord compression: clinical significance of increased signal intensity on MR images. Radiology 1989; 173: 219–224.
Li F, Chen Z, Zhang F, Shen H, Hou T . A meta-analysis showing that high signal intensity on T2-weighted MRI is associated with poor prognosis for patients with cervical spondylotic myelopathy. J Clin Neurosci 2011; 18: 1592–1595.
Kadanka Z, Mares M, Bednarik J, Smrcka V, Krbec M, Chaloupka R et al. Predictive factors for mild forms of spondylotic cervical myelopathy treated conservatively or surgically. Eur J Neurol 2005; 12: 16–24.
Shimomura T, Sumi M, Nishida K, Maeno K, Tadokoro K, Miyamoto H et al. Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine (Phila Pa 1976) 2007; 32: 2474–2479.
Oshima Y, Seichi A, Takeshita K, Chikuda H, Ono T, Baba S et al. Natural course and prognostic factors in patients with mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spine (Phila Pa 1976) 2012; 37: 1909–1913.
Vedantam A, Jonathan A, Rajshekhar V . Association of magnetic resonance imaging signal changes and outcome prediction after surgery for cervical spondylotic myelopathy. J Neurosurg Spine 2011; 15: 660–666.
Matsuda Y, Miyazaki K, Tada K, Yasuda A, Nakayama T, Murakami H et al. Increased MR signal intensity due to cervical myelopathy. Analysis of 29 surgical cases. J Neurosurg 1991; 74: 887–892.
Wada E, Ohmura M, Yonenobu K . Intramedullary changes of the spinal cord in cervical spondylotic myelopathy. Spine 1995; 20: 2226–2232.
Morio Y, Yamamoto K, Kuranobu K, Murata M, Tuda K . Does increased signal intensity of the spinal cord on MR images due to cervical myelopathy predict prognosis? Arch Orthop Trauma Surg 1994; 113: 254–259.
Chen CJ, Lyu RK, Lee ST, Wong YC, Wang LJ . Intramedullary high signal intensity on T2-weighted MR images in cervical spondylotic myelopathy: prediction of prognosis with type of intensity. Radiology 2001; 221: 789–794.
Fernandez de Rota JJ, Meschian S, Fernandez de Rota A, Urbano V, Baron M . Cervical spondylotic myelopathy due to chronic compression: the role of signal intensity changes in magnetic resonance images. J Neurosurg Spine 2007; 6: 17–22.
Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C . Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery 1998; 43: 43–49.
Ramanauskas WL, Wilner HI, Metes JJ, Lazo A, Kelly JK . MR imaging of compressive myelomalacia. J Comput Assist Tomogr 1989; 13: 399–404.
Ito T, Oyanagi K, Takahashi H, Takahashi HE, Ikuta F . Cervical spondylotic myelopathy: clinicopathologic study on the progression pattern and thin myelinated fibers of the lesions of seven patients examined during complete autopsy. Spine 1996; 21: 827–833.
Yone K, Sakou T, Yanase M, Ijiri K . Preoperative and postoperative magnetic resonance image evaluations of the spinal cord in cervical myelopathy. Spine (Phila Pa 1976) 1992; 17 (10 Suppl): S388–S392.
Ohshio I, Hatayama A, Kaneda K, Takahara M, Nagashima K . Correlation between histopathologic features and magnetic resonance images of spinal cord lesions. Spine 1993; 18: 1140–1149.
Vedantam A, Rajshekhar V . Does the type of T2 weighted hyperintensity influence surgical outcome in patients with cervical spondylotic myelopathy? Eur Spine J 2013; 22: 96–106.
Kadanka Z, Mares M, Bednanik J, Smrcka V, Krbec M, Stejskal L et al. Approaches to spondylotic cervical myelopathy: conservative versus surgical results in a 3-year follow-up study. Spine (Phila Pa 1976) 2002; 27: 2205–2210.
Kadanka Z, Bednarik J, Novotny O, Urbánek I, Dušek L . Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J 2011; 20: 1533–1538.
Epstein JA, Janin Y, Carras R, Lavine LS . A comparative study of the treatment of cervical spondylotic myeloradiculopathy. Experience with 50 cases treated by means of extensive laminectomy, foraminotomy, and excision of osteophytes during the past 10 years. Acta Neurochir (Wien) 1982; 61: 89–104.
Sampath P, Bendebba M, Davis JD, Ducker TB . Outcome of patients treated for cervical myelopathy. A prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976) 2000; 25: 670–676.
Yarbrough CK, Murphy RK, Ray WZ, Stewart TJ . The natural history and clinical presentation of cervical spondylotic myelopathy. Adv Orthop 2012; 2012: 480643.
Matz PG . Does nonoperative management play a role in the treatment of cervical spondylotic myelopathy? Spine J 2006; 6 (6 Suppl): 175S–181S.
Albert TJ, Vacarro A . Postlaminectomy kyphosis. Spine (Phila Pa 1976) 1998; 23: 2738–2745.
Uchida K, Nakajima H, Sato R, Yayama T, Mwaka ES, Kobayashi S et al. Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment: outcome after anterior or posterior decompression. J Neurosurg Spine 2009; 11: 521–528.
Acknowledgements
This study was supported by the 1255 Project of Changhai Hospital of Shanghai (Number: CH125520900, CH125540200).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Li, F., Li, Z., Huang, X. et al. The treatment of mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spinal Cord 52, 348–353 (2014). https://doi.org/10.1038/sc.2014.11
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2014.11