Abstract
Objectives:
This observational study aimed to determine the types of urological lesion encountered in veterans with traumatic spinal cord injury (SCI) with neurogenic bladder (NGB), and the usage of bladder management programs to deal with NGB.
Setting:
NGB (detrusor muscle and urethral sphincter dysfunction with loss of bladder sensation to void) is common in daily practice; however, information on types of urological lesions encountered in these veterans with NGB and how best to manage their NGB is limited.
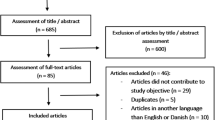
Methods:
We retrospectively reviewed the electronic charts of veterans with SCI enrolled in our program and regularly followed in our SCI clinic. Demographic data collected included: age, gender, ethnicity and age, level, severity and cause of spinal injury. Also noted was presence of NGB, episodes of urinary tract infection (UTI), bladder program followed and urological lesions found on renal nuclear scans, renal ultrasounds and cystoscopies.
Results:
Of the 161 veterans with SCI, symptoms of NGB was present in 133 (82.6%). Veterans with NGB had more severe spinal injury and more frequent UTI (P<0.05). Renal atrophy and hydronephrosis were the most common urological lesions seen in patients with UTI. Clean intermittent catheterization (CIC) was the most frequently used bladder program resulting in less frequent occurrence of UTI.
Conclusion:
Renal atrophy and hydronephrosis were the most common urological lesions encountered in veterans with NGB especially in those with UTI. CIC was the most frequently used bladder management program with the least risk for UTI.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rackley R, Kim ED . Neurogenic bladder. Available on: http://emedicine.medscape.com/article/453539-overview. Accessed on September 2012.
Wein AJ . Classification of neurogenic voiding dysfunction. J Urol 1981; 125: 605–609.
Chen Y, DeVivo MJ, Roseman JM . Current trend and risk factors for kidney stones in persons with spinal cord injury: a longitudinal study. Spinal Cord 2000; 38: 346–353.
Larsen LD, Chamberlin DA, Khonsari F, Ahlering TE . Retrospective analysis of urologic complications in male patients with spinal cord injury managed with and without indwelling urinary catheters. Urology 1997; 50: 418–422.
Smith JM . Indwelling catheter management: from habit-based to evidence-based practice. Ostomy Wound Manage 2003; 49: 34–45.
Guttmann L, Frankel H . The value of intermittent catheterisation in the early management of traumatic paraplegia and tetraplegia. Paraplegia 1966; 4: 63–84.
Lapides J, Diokno AC, Silber SJ, Lowe BS . Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Razdan S, Leboeuf L, Meinbach DS, Weinstein D, Gousse AE . Current practice patterns in the urologic surveillance and management of patients with spinal cord injury. Urology 2003; 61: 893–896.
Stöhrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol 2009; 56: 81–88.
American Spinal Injury Association Reference Manual of the International Standards for Neurological Classification of Spinal Cord Injury. American Spinal Injury Association: Chicago, IL, USA. 2003.
Chen D, Apple DF Jr, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury—current experience of the Model Systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Weld KJ, Dmochowski RR . Effect of bladder management on urological complications in spinal cord injured patients. J Urol 2000; 163: 768–772.
Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ . Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol 2010; 184: 213–217.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ . Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil 1999; 80: 1402–1410.
Weld KJ, Graney MJ, Dmochowski RR . Differences in bladder compliance with time and associations of bladder management with compliance in spinal cord injured patients. J Urol 2000; 163: 1228–1233.
Acknowledgements
CEA was funded for this study by the National Institutes of Health, National Institute of General Medical Sciences, grant 1 U54GM104938.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rabadi, M., Aston, C. Complications and urologic risks of neurogenic bladder in veterans with traumatic spinal cord injury. Spinal Cord 53, 200–203 (2015). https://doi.org/10.1038/sc.2014.205
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2014.205
This article is cited by
-
Bladder management in individuals with spinal cord injury or disease during and after primary rehabilitation: a retrospective cohort study
World Journal of Urology (2022)
-
Urinary bladder cancer as a late sequela of traumatic spinal cord injury
Military Medical Research (2021)
-
Harnblasenkarzinom als Spätfolge einer Querschnittlähmung
Der Urologe (2020)
-
Ursachenzusammenhang zwischen langjähriger Querschnittlähmung und malignen Harnblasentumoren
Trauma und Berufskrankheit (2019)
-
Long-term bladder and bowel management after spinal cord injury: a 20-year longitudinal study
Spinal Cord (2018)