Abstract
Study Design:
Retrospective investigation.
Objectives:
To investigate the association of patient and injury characteristics with bladder evacuation by indwelling catheterization in patients with chronic neurogenic lower urinary tract dysfunction (NLUTD).
Setting:
Tertiary urologic referral center.
Methods:
The patient database was screened for patients with chronic (>12 months) NLUTD. Patient characteristics and bladder management details were collected. Binary logistic regression analysis was used to investigate the effects of the investigated factors on bladder evacuation by indwelling catheterization.
Results:
The data of 1263 patients with a median age of 47 years (range 11–89 years) and a median NLTUD duration of 15.2 years (range 1.0–63.4 years) were investigated. The most common bladder evacuation method was intermittent catheterization (IC; 41.3%) followed by triggered reflex voiding (25.7%), suprapubic catheterization (11.8%), sacral anterior root stimulation (7.3%), spontaneous voiding (7.0%), abdominal straining (5.7%) and transurethral catheterization (1.3%). Female gender, tetraplegia, an age older than 45 years and injury duration were significant (<0.001) predictors of indwelling catheterization. The odds of bladder evacuation by indwelling catheterization were increased ~2.5, 3 and 4 times in women, patients older than 45 years and tetraplegics, respectively.
Conclusions:
IC is the most common bladder evacuation method. However, the majority of individuals with NLUTD are using other evacuation methods, because factors such as functional deficiencies, mental impairment or the social situation are relevant for choosing a bladder evacuation method. Individuals at risk of indwelling catheterization can be identified based on female gender, age, injury severity and injury duration.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Blok B, Pannek J, Castro-Diaz D, Del Popolo G, Groen J, Gross T et al. Guidelines on Neuro-Urology. (European Association of Urology, Bern, Switzerland, March 2015).
El-Masri WS, Chong T, Kyriakider AE, Wang D . Long-term follow-up study of outcomes of bladder management in spinal cord injury patients under the care of the Midlands Centre for Spinal Injuries in Oswestry. Spinal Cord 2012; 50: 14–21.
Bothig R, Hirschfeld S, Thietje R . Quality of life and urological morbidity in tetraplegics with artificial ventilation managed with suprapubic or intermittent catheterisation. Spinal Cord 2012; 50: 247–251.
Thorup J, Biering-Sorensen F, Cortes D . Urological outcome after myelomeningocele: 20 years of follow-up. BJU Int 2011; 107: 994–999.
Vaidyanathan S, Soni BM, Singh G, Oo T, Hughes PL . Barriers to implementing intermittent catheterisation in spinal cord injury patients in Northwest Regional Spinal Injuries Centre, Southport, UK. ScientificWorldJournal 2011; 11: 77–85.
Yavuzer G, Gok H, Tuncer S, Soygur T, Arikan N, Arasil T . Compliance with bladder management in spinal cord injury patients. Spinal Cord 2000; 38: 762–765.
Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ . Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol 2010; 184: 213–217.
West DA, Cummings JM, Longo WE, Virgo KS, Johnson FE, Parra RO . Role of chronic catheterization in the development of bladder cancer in patients with spinal cord injury. Urology 1999; 53: 292–297.
Stonehill WH, Dmochowski RR, Patterson AL, Cox CE . Risk factors for bladder tumors in spinal cord injury patients. J Urol 1996; 155: 1248–1250.
Bartel P, Krebs J, Wollner J, Gocking K, Pannek J . Bladder stones in patients with spinal cord injury: a long-term study. Spinal Cord 2014; 52: 295–297.
Mitsui T, Minami K, Furuno T, Morita H, Koyanagi T . Is suprapubic cystostomy an optimal urinary management in high quadriplegics?. A comparative study of suprapubic cystostomy and clean intermittent catheterization. Eur Urol 2000; 38: 434–438.
Ord J, Lunn D, Reynard J . Bladder management and risk of bladder stone formation in spinal cord injured patients. J Urol 2003; 170: 1734–1737.
Cameron AP, Wallner LP, Forchheimer MB, Clemens JQ, Dunn RL, Rodriguez G et al. Medical and psychosocial complications associated with method of bladder management after traumatic spinal cord injury. Arch Phys Med Rehabil 2011; 92: 449–456.
Rabadi MH, Aston C . Complications and urologic risks of neurogenic bladder in veterans with traumatic spinal cord injury. Spinal Cord (e-pub ahead of print 19 November 2014; doi:10.1038/sc.2014.205).
Singh R, Rohilla RK, Sangwan K, Siwach R, Magu NK, Sangwan SS . Bladder management methods and urological complications in spinal cord injury patients. Indian J Orthop 2011; 45: 141–147.
DeVivo MJ, Biering-Sorensen F, New P, Chen Y . Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord 2011; 49: 596–599.
Afsar SI, Yemisci OU, Cosar SN, Cetin N . Compliance with clean intermittent catheterization in spinal cord injury patients: a long-term follow-up study. Spinal Cord 2013; 51: 645–649.
Weld KJ, Graney MJ, Dmochowski RR . Differences in bladder compliance with time and associations of bladder management with compliance in spinal cord injured patients. J Urol 2000; 163: 1228–1233.
Hagen EM, Rekand T . Management of bladder dysfunction and satisfaction of life after spinal cord injury in Norway. J Spinal Cord Med 2014; 37: 310–316.
Yildiz N, Akkoc Y, Erhan B, Gunduz B, Yilmaz B, Alaca R et al. Neurogenic bladder in patients with traumatic spinal cord injury: treatment and follow-up. Spinal Cord 2014; 52: 462–467.
Kriz J, Relichova Z . Intermittent self-catheterization in tetraplegic patients: a 6-year experience gained in the spinal cord unit in Prague. Spinal Cord 2014; 52: 163–166.
Ginsberg D, Gousse A, Keppenne V, Sievert KD, Thompson C, Lam W et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol 2012; 187: 2131–2139.
Bellucci CH, de Castro Filho JE, Gomes CM, de Bessa J Jr, Battistella LR, Rubio de Souza D et al. Contemporary trends in the epidemiology of traumatic spinal cord injury: changes in age and etiology. Neuroepidemiology 2015; 44: 85–90.
Nijendijk JH, Post MW, van Asbeck FW . Epidemiology of traumatic spinal cord injuries in The Netherlands in 2010. Spinal Cord 2014; 52: 258–263.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Krebs, J., Wöllner, J. & Pannek, J. Bladder management in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord 54, 609–613 (2016). https://doi.org/10.1038/sc.2015.196
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2015.196
This article is cited by
-
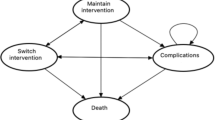
A cost-effectiveness analysis of bladder management strategies in neurogenic lower urinary tract dysfunction after spinal cord injury: A publicly funded health care perspective
Spinal Cord (2023)
-
Bladder management in individuals with spinal cord injury or disease during and after primary rehabilitation: a retrospective cohort study
World Journal of Urology (2022)
-
Usefulness of Hydrastis for the prevention of encrustation of long-term indwelling catheters in persons with neurogenic bladder dysfunction: a case series
Spinal Cord Series and Cases (2021)
-
Transvaginal bladder-neck closure: a step-by-step video for female pelvic surgeons
International Urogynecology Journal (2019)
-
Prevalence and Cost of Catheters to Manage Neurogenic Bladder
Current Bladder Dysfunction Reports (2018)