Abstract
Study design:
A cross-sectional study.
Objectives:
Neuropathic pain (NP) after spinal cord injury (SCI) tends to be hard to treat, and its heterogeneous properties make it difficult to identify and characterize. This study was conducted to assess the characteristics of SCI-related NP in detail.
Setting:
A single hospital for SCI rehabilitation.
Methods:
This study included 72 patients who were seen at our hospital in 2012 and 2013 and who had sustained SCI at least 3 months before enrollment. The patients completed the Neuropathic Pain Symptom Inventory (NPSI) and the Short Form (SF)-36 Health Inventory. The NPSI score was analyzed for correlations with clinical presentations of SCI and SF-36 subitems.
Results:
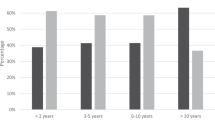
Paresthesia/dysesthesia was the most common subtype of NP after SCI. With regard to location, below-level superficial NP was significantly more intense than at-level pain. Patients who underwent surgery showed significantly less evoked pain compared with patients with non-surgery. Patients reported significantly more severe pain if >1 year had elapsed after the SCI. Patients with an American Spinal Injury Association Impairment Scale grade of B for completeness of injury reported more intense NP than those with other grades. Among the SF-36 subitems, NP correlated significantly with bodily pain, general health and mental health.
Conclusion:
NP in SCI patients was significantly associated with the location of pain, the time period since the injury, surgery and quality-of-life factors. A more detailed understanding of the characteristics of NP may contribute to better strategies for relieving the pain associated with SCI.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ . A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Jensen MP, Kuehn CM, Amtmann D, Cardenas DD . Symptom burden in persons with spinal cord injury. Arch Phys Med Rehabil 2007; 88: 638–645.
Rintala DH, Loubser PG, Castro J, Hart KA, Fuhrer MJ . Chronic pain in a community-based sample of men with spinal cord injury: prevalence, severity, and relationship with impairment, disability, handicap, and subjective well-being. Arch Phys Med Rehabil 1998; 79: 604–614.
Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T et al. International spinal cord injury pain classification: part I. Background and description. March 6-7, 2009. Spinal Cord 2012; 50: 413–417.
Norrbrink Budh C, Hultling C, Lundeberg T . Quality of sleep in individuals with spinal cord injury: a comparison between patients with and without pain. Spinal Cord 2005; 43: 85–95.
Melzack R . The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975; 1: 277–299.
Bennett M . The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain 2001; 92: 147–157.
Jang JY, Lee SH, Kim M, Ryu JS . Characteristics of neuropathic pain in patients with spinal cord injury. Ann Rehabil Med 2014; 38: 327–334.
Krause SJ, Backonja MM . Development of a neuropathic pain questionnaire. Clin J Pain 2003; 19: 306–314.
Bouhassira D, Attal N, Fermanian J, Alchaar H, Gautron M, Masquelier E et al. Development and validation of the Neuropathic Pain Symptom Inventory. Pain 2004; 108: 248–257.
Bouhassira D, Chassany O, Gaillat J, Hanslik T, Launay O, Mann C et al. Patient perspective on herpes zoster and its complications: an observational prospective study in patients aged over 50 years in general practice. Pain 2012; 153: 342–349.
Truini A, Padua L, Biasiotta A, Caliandro P, Pazzaglia C, Galeotti F et al. Differential involvement of A-delta and A-beta fibres in neuropathic pain related to carpal tunnel syndrome. Pain 2009; 145: 105–109.
Nakamura M, Tsuji O, Iwanami A, Tsuji T, Ishii K, Toyama Y et al. Central neuropathic pain after surgical resection in patients with spinal intramedullary tumor. J Orthop Sci 2012; 17: 352–357.
Calmels P, Mick G, Perrouin-Verbe B, Ventura M . SOFMER (French Society for Physical Medicine and Rehabilitation). Neuropathic pain in spinal cord injury: identification, classification, evaluation. Ann Phys Rehabil Med 2009; 52: 83–102.
Widerstrom-Noga E, Biering-Sorensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP et al. The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord 2014; 52: 282–286.
Maynard FM Jr., Bracken MB, Creasey G, Ditunno JF Jr., Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Fukuhara S, Ware JE Jr., Kosinski M, Wada S, Gandek B . Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol 1998; 51: 1045–1053.
Finnerup NB, Johannesen IL, Sindrup SH, Bach FW, Jensen TS . Pain and dysesthesia in patients with spinal cord injury: a postal survey. Spinal Cord 2001; 39: 256–262.
Siddall PJ, Taylor DA, McClelland JM, Rutkowski SB, Cousins MJ . Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain 1999; 81: 187–197.
Werhagen L, Budh CN, Hultling C, Molander C . Neuropathic pain after traumatic spinal cord injury—relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord 2004; 42: 665–673.
Chang Y, Jung TD, Yoo DS, Hyun JK . Diffusion tensor imaging and fiber tractography of patients with cervical spinal cord injury. J Neurotrauma 2010; 27: 2033–2040.
Sved P, Siddall PJ, McClelland J, Cousins MJ . Relationship between surgery and pain following spinal cord injury. Spinal Cord 1997; 35: 526–530.
Ataoglu E, Tiftik T, Kara M, Tunc H, Ersoz M, Akkus S . Effects of chronic pain on quality of life and depression in patients with spinal cord injury. Spinal Cord 2013; 51: 23–26.
Hallstrom H, Norrbrink C . Screening tools for neuropathic pain: can they be of use in individuals with spinal cord injury? Pain 2011; 152: 772–779.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nagoshi, N., Kaneko, S., Fujiyoshi, K. et al. Characteristics of neuropathic pain and its relationship with quality of life in 72 patients with spinal cord injury. Spinal Cord 54, 656–661 (2016). https://doi.org/10.1038/sc.2015.210
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2015.210
This article is cited by
-
Factors associated with neuropathic pain in Colombian patients with spinal cord injury of traumatic origin: case–control study
Spinal Cord Series and Cases (2022)
-
The association of Type D personality with functional outcomes, quality of life and neuropathic pain in persons with spinal cord injury
Spinal Cord (2022)
-
Neuropathic pain after spinal intradural benign tumor surgery: an underestimated complication?
Neurosurgical Review (2022)
-
Pain characteristics in Italian people with spinal cord injury: a multicentre study
Spinal Cord (2022)
-
Which factors have an association to the Quality of Life (QoL) of people with acquired Spinal Cord Injury (SCI)? A cross-sectional explorative observational study
Spinal Cord (2021)