Abstract
Study design:
This is a prospective cohort study.
Objectives:
The objective of this study was to predict the progress of healing of pressure ulcers (PUs) in spinal cord injury (SCI) patients after the first 4 weeks.
Setting:
The study was conducted in a specialized SCI rehabilitation unit in The Netherlands.
Methods:
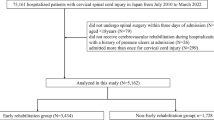
Weekly measurements of length, width and depth/undermining of grades II–IV PUs under sacrum or ischial tuberosity in SCI patients with the ‘Decu-stick’ were taken. The speed of reduction of the greatest dimension in the first 4 weeks of the granulation–epithelization (G–E) phase was compared with the speed of reduction of this dimension after week 4 until the end of observation.
Results:
Fifty-one PUs in 45 patients were measured. During the first 4 weeks of the G–E phase, the greatest dimension of 23/51 PUs reduced with a speed of ⩾0.5 cm per week. In 22 of these 23 PUs, this speed remained ⩾0.5 from week 4 until the end of observation (weeks 5–22). Closure: 21 patients (pts); operation: 2 pts. Of 28/51 PUs, this dimension reduced with <0.5 cm per week. In 27/28 PUs, this speed remained <0.5 from week 4 until the end of observation (weeks 9–37). Closure: 6 pts; operation: 16 pts; discharge with open ulcer: 6 pts.
Conclusion:
Measurement of PUs in SCI patients with the ‘Decu-stick’ provides a reliable, quick, cheap and easy-to-learn bedside method to predict the progress of healing in PUs in SCI patients after 4 weeks of conservative treatment with a positive predictive value of 0.95 and an negative predictive value of 0.96. This provides a scientific basis for the decision on operative or alternative conservative treatment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Consortium for Spinal Cord Medicine Pressure Ulcer Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals. Paralysed Veterans of America: Washington, DC, USA. 2000.
Raghavan P, Raza WA, Ahmed YS, Chamberlain MA . Prevalence of pressure sores in a community sample of spinal injury patients. Clin Rehabil 2003; 17: 879–884.
Nogueira PC, Caliri MH, Haas VJ . Profile of patients with spinal cord injuries and occurrence of pressure ulcer at a university hospital. Rev Lat Am Enfermagem 2006; 14: 372–377.
Verschueren JH, Post MW, de Groot S, van der Woude LH, van Asbeck FW, Rol M et al. Occurrence and predictors of pressure ulcers during primary in-patient spinal cord injury rehabilitation. Spinal Cord 2011; 49: 106–112.
Xu Y, Sun J, Carter RR, Bogie KM . Personalized prediction of chronic wound healing: an exponential mixed effects model using stereophotogrammetric measurement. J Tissue Viability 2014; 23: 48–59.
Flanagan M . Improving accuracy of wound measurement in clinical practice. Ostomy Wound Manage 2003; 49: 28–40.
Jessup RL . What is the best method for assessing the rate of wound healing? A comparison of 3 mathematical formulas. Adv Skin Wound Care 2006; 19: 138–147.
Landelijke Richtlijn Preventie en Behandeling Decubitus. Verpleegkundigen & Verzorgenden Nederland (V&VN) (National Guideline Prevention and Treatment Pressure Ulcers. Dutch Nursing Association): Utrecht, The Netherlands. 2011, pp 19.
Van Lis MS, van Asbeck FW, Post MW . Monitoring healing of pressure ulcers: a review of assessment instruments for use in the spinal cord unit. Spinal Cord 2010; 48: 92–99.
Matsui Y, Furue M, Sanada H, Tachibana T, Nakayama T, Sugama J et al. Development of the DESIGN-R with an observational study: an absolute evaluation tool for monitoring pressure ulcer wound healing. Wound Repair Regen 2011; 19: 309–315.
Kundin JI . A new way to size up a wound. Am J Nurs 1989; 89: 206–207.
Bates-Jensen BM . The Pressure Sore Status Tool, a few thousand assessments later. Adv Wound Care 1997; 10: 65–73.
Ferrell BA . The Sessing Scale for measurement of pressure ulcer healing. Adv Wound Care 1997; 10: 78–80.
Sussman C . Presenting a draft pressure ulcer scale to monitor healing. Adv Wound Care 1997; 10: 92.
Stotts NA, Rodeheaver GT, Thomas DR, Frantz RA, Bartolucci AA, Sussman C et al. An instrument to measure healing in pressure ulcers: development and validation of the Pressure Ulcer Scale for Healing (PUSH). J Gerontol A Biol Sci Med Sci 2001; 56: M795–M799.
Harris C, Bates-Jensen B, Parslow N, Raizman R, Singh M, Ketchen R et al. Bates-Jensen wound assessment tool: pictorial guide validation project. J Wound Ostomy Continence Nurs 2010; 37: 253–259.
Barber S . A clinically relevant wound assessment method to monitor healing progression. Ostomy Wound Manage 2008; 54: 42–49.
O'Meara SM, Bland JM, Dumville JC, Cullum NA . A systematic review of the performance of instruments designed to measure the dimensions of pressure ulcers. Wound Repair Regen 2012; 20: 263–276.
Asbeck FWA van . De DECU-stick: een eenvoudige manier om decubitus te meten. Ned Tijdschr Geneesk 1997; 141: 1718.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The first author is chairman of the non-profit foundation ‘Meten is weten’ (Measurement for knowledge) that has provided the instruction website www.decu-stick.org. The remaining authors declared no conflict of interest.
Rights and permissions
About this article
Cite this article
Van Asbeck, F., Post, M. Bedside prediction of the progress of pressure ulcer healing in patients with spinal cord injury using the ‘Decu-stick’. Spinal Cord 53, 539–543 (2015). https://doi.org/10.1038/sc.2015.40
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2015.40