Abstract
Study design:
Longitudinal observational study.
Objective:
To quantify the amount of upper- and lower-extremity movement repetitions (that is, voluntary movements as part of a functional task or specific motion) occurring during inpatient spinal cord injury (SCI), physical (PT) and occupational therapy (OT), and examine changes over the inpatient rehabilitation stay.
Setting:
Two stand-alone inpatient SCI rehabilitation centers.
Methods:
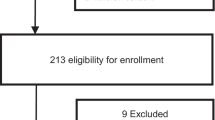
Participants: A total of 103 patients were recruited through consecutive admissions to SCI rehabilitation. Interventions: Trained assistants observed therapy sessions and obtained clinical outcome measures in the second week following admission and in the second to last week before discharge. Main outcome measures: PT and OT time, upper- and lower-extremity repetitions and changes in these outcomes over the course of rehabilitation stay.
Results:
We observed 561 PT and 347 OT sessions. Therapeutic time comprised two-thirds of total therapy time. Summed over PT and OT, the median upper-extremity repetitions in patients with paraplegia were 7 repetitions and in patients with tetraplegia, 42 repetitions. Lower-extremity repetitions and steps primarily occurred in ambulatory patients and amounted to 218 and 115, respectively (summed over PT and OT sessions at discharge). Wilcoxon-signed rank tests revealed that most repetition variables did not change significantly over the inpatient rehabilitation stay. In contrast, clinical outcomes for the arm and leg improved over this time period.
Conclusions:
Repetitions of upper- and lower-extremity movements are markedly low during PT and OT sessions. Despite improvements in clinical outcomes, there was no significant increase in movement repetitions over the course of inpatient rehabilitation stay.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Whiteneck G, Gassaway J, Dijkers M, Backus DD, Charlifue S, Chen D et al. Inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med 2011; 34: 133–148.
Teeter L, Gassaway J, Taylor S, LaBarbera J, McDowell S, Backus DD et al. Relationship of physical therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Cord Med 2012; 35: 503–526.
Ozelie R, Gassaway J, Buchman E, Thimmaiah D, Heisler L, Cantoni K et al. Relationship of occupational therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med 2012; 35: 527–546.
Heinemann AW, Hamilton B, Linacre JM, Wright BD, Granger C . Functional status and therapeutic intensity during inpatient rehabilitation. Am J Phys Med Rehabil 1995; 74: 315–326.
van Langeveld SA, Post MW, van Asbeck FW, Gregory M, Halvorsen A, Rijken H et al. Comparing content of therapy for people with a spinal cord injury in postacute inpatient rehabilitation in Australia, Norway, and the Netherlands. Phys Ther 2011; 91: 210–224.
van Langeveld SA, Post MW, van Asbeck FW, Horst ter P, Leenders J, Postma K et al. Contents of physical therapy, occupational therapy, and sports therapy sessions for patients with a spinal cord injury in three Dutch rehabilitation centres. Disabil Rehabil 2011; 33: 412–422.
Taylor-Schroeder S, LaBarbera J, McDowell S, Zanca JM, Natale A, Mumma S et al. The SCIRehab project: treatment time spent in SCI rehabilitation. Physical therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011; 34: 149–161.
Foy T, Perritt G, Thimmaiah D, Heisler L, Offutt JL, Cantoni K et al. The SCIRehab project: treatment time spent in SCI rehabilitation. Occupational therapy treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med 2011; 34: 162–175.
Edgerton VR, Tillakaratne NJK, Bigbee AJ, de Leon RD, Roy RR . Plasticity of the spinal neural circuitry after injury. Annu Rev Neurosci 2004; 27: 145–167.
Girgis J, Merrett D, Kirkland S, Metz GAS, Verge V, Fouad K . Reaching training in rats with spinal cord injury promotes plasticity and task specific recovery. Brain 2007; 130: 2993–3003.
Beekhuizen KS, Field-Fote EC . Massed practice versus massed practice with stimulation: effects on upper extremity function and cortical plasticity in individuals with incomplete cervical spinal cord injury. Neurorehabil Neural Repair 2005; 19: 33–45.
Hoffman LR, Field-Fote EC . Functional and corticomotor changes in individuals with tetraplegia following unimanual or bimanual massed practice training with somatosensory stimulation: a pilot study. J Neurol Phys Ther 2010; 34: 193–201.
Behrman AL, Bowden MG, Nair PM . Neuroplasticity after spinal cord injury and training: an emerging paradigm shift in rehabilitation and walking recovery. Phys Ther 2006; 86: 1406–1425.
de Leon RD, Hodgson JA, Roy RR, Edgerton VR . Locomotor capacity attributable to step training versus spontaneous recovery after spinalization in adult cats. J Neurophysiol 1998; 79: 1329–1340.
Lovely RG, Gregor RJ, Roy RR, Edgerton VR . Effects of training on the recovery of full-weight-bearing stepping in the adult spinal cat. Exp Neurol 1986; 92: 421–435.
Battistuzzo CR, Callister RJ, Callister R, Galea MP . A systematic review of exercise training to promote locomotor recovery in animal models of spinal cord injury. J Neurotrauma 2012; 29: 1600–1613.
Norrie BA, Nevett-Duchcherer JM, Gorassini MA . Reduced functional recovery by delaying motor training after spinal cord injury. J Neurophysiol 2005; 94: 255–264.
Harkema S, Gerasimenko Y, Hodes J, Burdick J, Angeli C, Chen Y et al. Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: a case study. Lancet 2011; 377: 1938–1947.
Winchester P, Smith P, Foreman N, Mosby JM, Pacheco F, Querry R et al. A prediction model for determining over ground walking speed after locomotor training in persons with motor incomplete spinal cord injury. J Spinal Cord Med 2009; 32: 63–71.
McKinley WO, Seel RT, Hardman JT . Nontraumatic spinal cord injury: incidence, epidemiology, and functional outcome. YAPMR 1999; 80: 619–623.
Ozelie RR, Sipple CC, Foy TT, Cantoni KK, Kellogg KK, Lookingbill JJ et al. SCIRehab project series: the occupational therapy taxonomy. J Spinal Cord Med 2009; 32: 283–297.
Natale A, Taylor S, LaBarbera J, Bensimon L, McDowell S, Mumma SL et al. SCIRehab project series: the physical therapy taxonomy. J Spinal Cord Med 2009; 32: 270–282.
Lang CE, MacDonald JR, Reisman DS, Boyd L, Kimberley TJ, Schindler-Ivens SM et al. Observation of amounts of movement practice provided during stroke rehabilitation. YAPMR 2009; 90: 1692–1698.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC et al. The spinal cord independence measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil 2007; 29: 1926–1933.
Burns AS, Delparte JJ, Patrick M, Marino RJ, Ditunno JF . The reproducibility and convergent validity of the walking index for spinal cord injury (WISCI) in chronic spinal cord injury. Neurorehabil Neural Repair 2011; 25: 149–157.
Mathiowetz V, Weber K, Volland G, Kashman N . Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am 1984; 9: 222–226.
Bohannon RW, Schaubert KL . Test-retest reliability of grip-strength measures obtained over a 12-week interval from community-dwelling elders. J Hand Ther 2005; 18: 426–427 –quiz428.
Rudhe C, Van Hedel HJA . Upper extremity function in persons with tetraplegia: relationships between strength, capacity, and the spinal cord independence measure. Neurorehabil Neural Repair 2009; 23: 413–421.
Kalsi-Ryan S, Beaton D, Curt A, Duff S, Popovic MR, Rudhe C et al. The graded redefined assessment of strength sensibility and prehension: reliability and validity. J Neurotrauma 2012; 29: 905–914.
Rosenthal R . Parametric measures of effect size. In: Cooper H, Hedges LV (eds). The Handbook of Research Synthesis. Russell Sage Foundation: New York, NY, USA. 1994.
Cohen J . Statistical Power Analysis for the Behavioral Sciences, 2nd edn. Lawrence Erlbaum Associates: Hillsdale, NJ, USA. 1988.
Benjamini Y, Hochberg Y . Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 1995; 57: 289–300.
Cha J, Heng C, Reinkensmeyer DJ, Roy RR, Edgerton VR, de Leon RD . Locomotor ability in spinal rats is dependent on the amount of activity imposed on the hindlimbs during treadmill training. J Neurotrauma 2007; 24: 1000–1012.
Cowan RE, Boninger ML, Sawatzky BJ, Mazoyer BD, Cooper RA . Preliminary outcomes of the SmartWheel Users' Group database: a proposed framework for clinicians to objectively evaluate manual wheelchair propulsion. Arch Phys Med Rehabil 2008; 89: 260–268.
Weishaupt N, Li S, Di Pardo A, Sipione S, Fouad K . Synergistic effects of BDNF and rehabilitative training on recovery after cervical spinal cord injury. Behav Brain Res 2013; 239: 31–42.
Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual [Internet]. www.cms.gov.www.cms.gov, 2014. Available from http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/bp102c01.pdf. Accessed on 7 March 2014.
Harris JE, Eng JJ, Miller WC, Dawson AS . A self-administered Graded Repetitive Arm Supplementary Program (GRASP) improves arm function during inpatient stroke rehabilitation: a multi-site randomized controlled trial. Stroke 2009; 40: 2123–2128.
Connell LA, McMahon NE, Simpson LA, Watkins CL, Eng JJ . Investigating measures of intensity during a structured upper limb exercise program in stroke rehabilitation: an exploratory study. Arch Phys Med Rehabil 2014; 95: 2410–2419.
Acknowledgements
DZ is supported by a Doctoral Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. JJE acknowledges salary support from the Canada Research Chair Program. This research is supported by the Canadian Institutes of Health Research. We thank the research assistants for their work, especially Erika Brown, Jenna Homer, and Amanda Mow, and the rehabilitation centers, therapists and patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zbogar, D., Eng, J., Miller, W. et al. Movement repetitions in physical and occupational therapy during spinal cord injury rehabilitation. Spinal Cord 55, 172–179 (2017). https://doi.org/10.1038/sc.2016.129
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2016.129
This article is cited by
-
Arm-hand training strategies and therapy dose dimensions during the subacute rehabilitation of people with cervical spinal cord injury: a longitudinal observational study
Spinal Cord (2025)
-
Artificial intelligence tools for engagement prediction in neuromotor disorder patients during rehabilitation
Journal of NeuroEngineering and Rehabilitation (2024)
-
Early and intensive Motor Training for people with spinal cord injuries (the SCI-MT Trial): description of the intervention
Spinal Cord (2023)
-
Early and intensive motor training to enhance neurological recovery in people with spinal cord injury: trial protocol
Spinal Cord (2023)
-
Feasibility of home hand rehabilitation using musicglove after chronic spinal cord injury
Spinal Cord Series and Cases (2022)