Abstract
Study design:
Methodological validation of dual-energy x-ray absorptiometry (DXA)-based measures of leg bone mineral density (BMD) based on the guidelines of the International Society for Clinical Densitometry.
Objectives:
The primary objective of this study was to determine the precision of BMD estimates at the knee and heel using the manufacturer provided DXA acquisition algorithm. The secondary objective was to determine the smallest change in DXA-based measurement of BMD that should be surpassed (least significant change (LSC)) before suggesting that a biological change has occurred in the distal femur, proximal tibia and calcaneus.
Setting:
Academic Research Centre, Canada.
Methods:
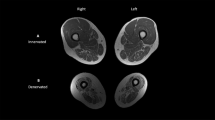
Ten people with motor-complete SCI of at least 2 years duration and 10 people from the general population volunteered to have four DXA-based measurements taken of their femur, tibia and calcaneus. BMDs for seven regions of interest (RIs) were calculated, as were short-term precision (root-mean-square (RMS) standard deviation (g cm−2), RMS-coefficient of variation (RMS-CV, %)) and LSC.
Results:
Overall, RMS-CV values were similar between SCI (3.63–10.20%, mean=5.3%) and able-bodied (1.85–5.73%, mean=4%) cohorts, despite lower absolute BMD values at each RIs in those with SCI (35%, heel to 54%, knee; P<0.0001). Precision was highest at the calcaneus and lowest at the femur. Except at the femur, RMS-CV values were under 6%.
Conclusions:
For DXA-based estimates of BMD at the distal femur, proximal tibia and calcaneus, these precision values suggest that LSC values >10% are needed to detect differences between treated and untreated groups in studies aimed at reducing bone mineral loss after SCI.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Qin W, Bauman WA, Cardozo C . Bone and muscle loss after spinal cord injury: organ interactions. Ann NY Acad Sci 2010; 1211: 66–84.
Biering-Sorensen F, Hansen B, Lee BS . Non-pharmacological treatment and prevention of bone loss after spinal cord injury: a systematic review. Spinal Cord. 2009; 47: 508–518.
Vestergaard P, Krogh K, Rejnmark L, Mosekilde L . Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord 1998; 36: 790–796.
Logan WC Jr, Sloane R, Lyles KW, Goldstein B, Hoenig HM . Incidence of fractures in a cohort of veterans with chronic multiple sclerosis or traumatic spinal cord injury. Arch Phys Med Rehabil 2008; 89: 237–243.
Lazo MG, Shirazi P, Sam M, Giobbie-Hurder A, Blacconiere MJ, Muppidi M . Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord 2001; 39: 208–214.
Gifre L, Vidal J, Carrasco J, Portell E, Puig J, Monegal A et al. Incidence of skeletal fractures after traumatic spinal cord injury: a 10-year follow-up study. Clin Rehabil 2014; 28: 361–369.
Mohr T, Podenphant J, Biering-Sorensen F, Galbo H, Thamsborg G, Kjaer M . Increased bone mineral density after prolonged electrically induced cycle training of paralyzed limbs in spinal cord injured man. Calcif Tissue Int 1997; 61: 22–25.
Dudley-Javoroski S, Saha PK, Liang G, Li C, Gao Z, Shields RK . High dose compressive loads attenuate bone mineral loss in humans with spinal cord injury. Osteoporos Int 2012; 23: 2335–2346.
de Bruin ED, Frey-Rindova P, Herzog RE, Dietz V, Dambacher MA, Stussi E . Changes of tibia bone properties after spinal cord injury: effects of early intervention. Arch Phys Med Rehabil 1999; 80: 214–220.
Alekna V, Tamulaitiene M, Sinevicius T, Juocevicius A . Effect of weight-bearing activities on bone mineral density in spinal cord injured patients during the period of the first two years. Spinal Cord 2008; 46: 727–732.
Bonnick SL . Bone Densitometry in Clincal Practice: Application and Interpretation, 3rd edn. Humana Press, Springer: New York, NY. 2010.
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S . Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom 2013; 16: 455–466.
Biering-Sorensen F, Bohr H, Schaadt O . Bone mineral content of the lumbar spine and lower extremities years after spinal cord lesion. Paraplegia 1988; 26: 293–301.
Garland DE, Adkins RH, Scott M, Singh H, Massih M, Stewart C . Bone loss at the os calcis compared with bone loss at the knee in individuals with spinal cord injury. J Spinal Cord Med 2004; 27: 207–211.
Suominen H, Heikkinen E, Vainio P, Lahtinen T . Mineral density of calcaneus in men at different ages: a population study with special reference to life-style factors. Age Ageing 1984; 13: 273–281.
Pettersson U, Nilsson M, Sundh V, Mellstrom D, Lorentzon M . Physical activity is the strongest predictor of calcaneal peak bone mass in young Swedish men. Osteoporos Int 2010; 21: 447–455.
Williams JA, Wagner J, Wasnich R, Heilbrun L . The effect of long-distance running upon appendicular bone mineral content. Med Sci Sports Exerc 1984; 16: 223–227.
Szucs J, Jonson R, Granhed H, Hansson T . Accuracy, precision, and homogeneity effects in the determination of the bone mineral content with dual photon absorptiometry in the heel bone. Bone 1992; 13: 179–183.
Yamada M, Ito M, Hayashi K, Nakamura T . Calcaneus as a site for assessment of bone mineral density: evaluation in cadavers and healthy volunteers. Am J Roentgenol 1993; 161: 621–627.
Pacheco EM, Harrison EJ, Ward KA, Lunt M, Adams JE . Detection of osteoporosis by dual energy X-ray absorptiometry (DXA) of the calcaneus: is the WHO criterion applicable? Calcif Tissue Int 2002; 70: 475–482.
Sievanen H, Oja P, Vuori I . Precision of dual-energy x-ray absorptiometry in determining bone mineral density and content of various skeletal sites. J Nucl Med 1992; 33: 1137–1142.
Dauty M, Perrouin Verbe B, Maugars Y, Dubois C, Mathe JF . Supralesional and sublesional bone mineral density in spinal cord-injured patients. Bone 2000; 27: 305–309.
Morse LR, Lazzari AA, Battaglino R, Stolzmann KL, Matthess KR, Gagnon DR et al. Dual energy x-ray absorptiometry of the distal femur may be more reliable than the proximal tibia in spinal cord injury. Arch Phys Med Rehabil 2009; 90: 827–831.
Haddaway MJ, Davie MW, Davies HL, Sharp CA . Application of sub-regional analysis to bone mineral density of the lower limb from whole body DXA scans. Physiol Meas 2013; 34: 757–768.
McPherson JG, Edwards WB, Prasad A, Troy KL, Griffith JW, Schnitzer TJ . Dual energy X-ray absorptiometry of the knee in spinal cord injury: methodology and correlation with quantitative computed tomography. Spinal Cord 2014; 52: 821–825.
Bakkum AJ, Janssen TW, Rolf MP, Roos JC, Burcksen J, Knol DL et al. A reliable method for measuring proximal tibia and distal femur bone mineral density using dual-energy X-ray absorptiometry. Med Eng Phys 2014; 36: 387–390.
Yu EW, Thomas BJ, Brown JK, Finkelstein JS . Simulated increases in body fat and errors in bone mineral density measurements by DXA and QCT. J Bone Miner Res 2012; 27: 119–124.
Tothill P, Weir N, Loveland J . Errors in dual-energy X-ray scanning of the hip because of nonuniform fat distribution. J Clin Densitom 2014; 17: 91–96.
Tothill P, Avenell A . Errors in dual-energy X-ray absorptiometry of the lumbar spine owing to fat distribution and soft tissue thickness during weight change. Br J Radiol 1994; 67: 71–75.
Farrell TJ, Webber CE . The error due to fat inhomogeneity in lumbar spine bone mineral measurements. Clin Phys Physiol Measure 1989; 10: 57–64.
Bonnick SL, Johnston CC Jr, Kleerekoper M, Lindsay R, Miller P, Sherwood L et al. Importance of precision in bone density measurements. J Clin Densitom 2001; 4: 105–110.
Kendall FP, Kendall McCreary E, Provance PG, Rodgers M, Romani W . Muscles: Testing and Function, with Posture and Pain, 5th edn. Lippincott Williams and Wilkins, Baltimore, MD, USA, 2005, 560pp.
Lohmann TG, Roche AF, Martorell R . Anthropometric Standardization Reference Manual. Human Kinetics Books: Champaign, IL, USA. 1988, 177pp.
Baim S, Wilson CR, Lewiecki EM, Luckey MM, Downs RW Jr, Lentle BC . Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom 2005; 8: 371–378.
Ito M, Nishida A, Kono J, Kono M, Uetani M, Hayashi K . Which bone densitometry and which skeletal site are clinically useful for monitoring bone mass? Osteoporos Int 2003; 14: 959–964.
Leslie WD, Moayyeri A . Minimum sample size requirements for bone density precision assessment produce inconsistency in clinical monitoring. Osteoporos Int 2006; 17: 1673–1680.
Acknowledgements
Funding for this project was provided from the University of Manitoba Research Grants Program, the Will to Win Gifted Professorship (to KC), the Daremax Foundation (to WP) and the Canadian Institutes of Health Research (to WP) and the University of Manitoba Undergraduate Research Award (to WJK). We thank the participants for volunteering their time and Christopher MacDonell (PhD) for critical comments and review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Peppler, W., Kim, W., Ethans, K. et al. Precision of dual-energy X-ray absorptiometry of the knee and heel: methodology and implications for research to reduce bone mineral loss after spinal cord injury. Spinal Cord 55, 483–488 (2017). https://doi.org/10.1038/sc.2016.170
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2016.170
This article is cited by
-
Electrical stimulation paradigms on muscle quality and bone mineral density after spinal cord injury
Osteoporosis International (2025)
-
Bone Loss and the Current Diagnosis of Osteoporosis and Risk of Fragility Fracture in Persons with Spinal Cord Injury
Current Physical Medicine and Rehabilitation Reports (2020)
-
Incidental bilateral calcaneal fractures following overground walking with a wearable robotic exoskeleton in a wheelchair user with a chronic spinal cord injury: is zero risk possible?
Osteoporosis International (2020)