Abstract
Objective:
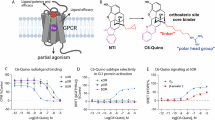
The current study aimed to evaluate the contribution(s) of specific opioid receptor systems to the analgesic and detrimental effects of morphine, observed after spinal cord injury in prior studies.
Study design:
We used specific opioid receptor agonists to assess the effects of μ- (DAMGO), δ- (DPDPE) and κ- (GR89696) opioid receptor activation on locomotor (Basso, Beattie and Bresnahan scale, tapered beam and ladder tests) and sensory (girdle, tactile and tail-flick tests) recovery in a rodent contusion model (T12). We also tested the contribution of non-classic opioid binding using [+]- morphine.
Methods:
First, a dose–response curve for analgesic efficacy was generated for each opioid agonist. Baseline locomotor and sensory reactivity was assessed 24 h after injury. Subjects were then treated with an intrathecal dose of a specific agonist and re-tested after 30 min. To evaluate the effects on recovery, subjects were treated with a single dose of an agonist and both locomotor and sensory function were monitored for 21 days.
Results:
All agonists for the classic opioid receptors, but not the [+]- morphine enantiomer, produced antinociception at a concentration equivalent to a dose of morphine previously shown to produce strong analgesic effects (0.32 μmol). DAMGO and [+]- morphine did not affect long-term recovery. GR89696, however, significantly undermined the recovery of locomotor function at all doses tested.
Conclusions:
On the basis of these data, we hypothesize that the analgesic efficacy of morphine is primarily mediated by binding to the classic μ-opioid receptor. Conversely, the adverse effects of morphine may be linked to activation of the κ-opioid receptor. Ultimately, elucidating the molecular mechanisms underlying the effects of morphine is imperative to develop safe and effective pharmacological interventions in a clinical setting.
Setting:
USA.
Sponsorship:
Grant DA31197 to MA Hook and the NIDA Drug Supply Program.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Consortium for Spinal Cord Medicine. Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2008; 31: 408–479.
Neighbor ML, Honner S, Kohn MA . Factors affecting emergency department opioid administration to severely injured patients. Acad Emerg Med 2004; 11: 1290–1296.
Woller SA, Moreno GL, Hart N, Wellman PJ, Grau JW, Hook MA . Analgesia or addiction?: implications for morphine use after spinal cord injury. J Neurotrauma 2012; 29: 1650–1662.
Hook MA, Washburn SN, Moreno G, Woller SA, Puga D, Lee KH et al. An IL-1 receptor antagonist blocks a morphine-induced attenuation of locomotor recovery after spinal cord injury. Brain Behav Immun 2011; 25: 349–359.
Hook MA, Liu GT, Washburn SN, Ferguson AR, Bopp AC, Huie JR et al. The impact of morphine after a spinal cord injury. Behav Brain Res 2007; 179: 281–293.
Hook MA, Moreno G, Woller S, Puga D, Hoy K Jr, Balden R et al. Intrathecal morphine attenuates recovery of function after a spinal cord injury. J Neurotrauma 2009; 26: 741–752.
Woller SA, Malik JS, Aceves M, Hook MA . Morphine self-administration following spinal cord injury. J Neurotrauma 2014; 31: 1570–1583.
Kristensen K, Christensen CB, Christrup LL . The mu 1, mu 2, delta, kappa opioid receptor binding profiles of methadone stereoisomers and morphine. Life Sci 1994; 56: 45–50.
Wang X, Loram LC, Ramos K, de Jesus AJ, Thomas J, Cheng K et al. Morphine activates neuroinflammation in a manner parallel to endotoxin. Proc Natl Acad Sci USA 2012; 109: 6325–6330.
Chen L, Huang L-YM . Protein kinase C reduces Mg2+ block of NMDA-receptor channels as a mechanism of modulation. Nature 1992; 356: 521–523.
Yang L, Wang S, Sung B, Lim G, Mao J . Morphine induces ubiquitin-proteasome activity and glutamate transporter degradation. J Biol Chem 2008; 283: 21703–21713.
Mao J, Sung B, Ji R-R, Lim G . Chronic morphine induces downregulation of spinal glutamate transporters: implications in morphine tolerance and abnormal pain sensitivity. J Neurosci 2002; 22: 8312–8323.
Mao J, Sung B, Ji R-R, Lim G . Neuronal apoptosis associated with morphine tolerance: evidence for an opioid-induced neurotoxic mechanism. J Neurosci 2002; 22: 7650–7661.
Woolf CJ, Thompson SW . The induction and maintenance of central sensitization is dependent on N-methyl-D-aspartic acid receptor activation; implications for the treatment of post-injury pain hypersensitivity states. Pain 1991; 44: 293–299.
Faden AI, Jacobs TP . Dynorphin induces partially reversible paraplegia in the rat. Eur J Pharmacol 1983; 91: 321–324.
Faden AI, Takemori A, Portoghese P . κ-Selective opiate antagonist nor-binaltorphimine improves outcome after traumatic spinal cord injury in rats. Cent Nerv Syst Trauma 1987; 4: 227–234.
Watkins LR, Hutchinson MR, Rice KC, Maier SF . The “toll” of opioid-induced glial activation: improving the clinical efficacy of opioids by targeting glia. Trends Pharmacol Sci 2009; 30: 581–591.
Tawfik VL, Lacroix-Fralish ML, Nutile-McMenemy N, DeLeo JA . Transcriptional and translational regulation of glial activation by morphine in a rodent model of neuropathic pain. J Pharmacol Exp Ther 2005; 313: 1239–1247.
Hutchinson MR, Zhang Y, Brown K, Coats BD, Shridhar M, Sholar PW et al. Non‐stereoselective reversal of neuropathic pain by naloxone and naltrexone: involvement of toll‐like receptor 4 (TLR4). Eur J Neurosci 2008; 28: 20–29.
Hutchinson MR, Bland ST, Johnson KW, Rice KC, Maier SF, Watkins LR . Opioid-induced glial activation: mechanisms of activation and implications for opioid analgesia, dependence, and reward. ScientificWorldJournal 2007; 7: 98–111.
Hutchinson MR, Zhang Y, Shridhar M, Evans JH, Buchanan MM, Zhao TX et al. Evidence that opioids may have toll-like receptor 4 and MD-2 effects. Brain Behav Immun 2010; 24: 83–95.
Lewis SS, Hutchinson MR, Rezvani N, Loram LC, Zhang Y, Maier SF et al. Evidence that intrathecal morphine-3-glucuronide may cause pain enhancement via toll-like receptor 4/MD-2 and interleukin-1β. Neuroscience 2010; 165: 569–583.
Hutchinson MR, Lewis SS, Coats BD, Rezvani N, Zhang Y, Wieseler JL et al. Possible involvement of toll-like receptor 4/myeloid differentiation factor-2 activity of opioid inactive isomers causes spinal proinflammation and related behavioral consequences. Neuroscience 2010; 167: 880–893.
Hutchinson MR, Coats BD, Lewis SS, Zhang Y, Sprunger DB, Rezvani N et al. Proinflammatory cytokines oppose opioid-induced acute and chronic analgesia. Brain Behav Immun 2008; 22: 1178–1189.
Johnston IN, Milligan ED, Wieseler-Frank J, Frank MG, Zapata V, Campisi J et al. A role for proinflammatory cytokines and fractalkine in analgesia, tolerance, and subsequent pain facilitation induced by chronic intrathecal morphine. J Neurosci 2004; 24: 7353–7365.
Christensen MD, Hulsebosch CE . Chronic central pain after spinal cord injury. J Neurotrauma 1997; 14: 517–537.
Basso DM, Beattie MS, Bresnahan JC . A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma 1995; 12: 1–21.
Ferguson AR, Hook MA, Garcia G, Bresnahan JC, Beattie MS, Grau JW . A simple post hoc transformation that improves the metric properties of the BBB scale for rats with moderate to severe spinal cord injury. J Neurotrauma 2004; 21: 1601–1613.
Soblosky JS, Colgin LL, Chorney-Lane D, Davidson JF, Carey ME . Some functional recovery and behavioral sparing occurs independent of task-specific practice after injury to the rat's sensorimotor cortex. Behav Brain Res 1997; 89: 51–59.
Hicks SP, D'Amato CJ . Motor-sensory cortex-corticospinal system and developing locomotion and placing in rats. Am J Anat 1975; 143: 1–42.
von Euler M, Akesson E, Samuelsson EB, Seiger A, Sundstrom E . Motor performance score: a new algorithm for accurate behavioral testing of spinal cord injury in rats. Exp Neurol 1996; 137: 242–254.
von Euler M, Seiger A, Sundstrom E . Clip compression injury in the spinal cord: a correlative study of neurological and morphological alterations. Exp Neurol 1997; 145: 502–510.
Beattie MS . Anatomic and behavioral outcome after spinal cord injury produced by a displacement controlled impact device. J Neurotrauma 1992; 9: 157–159.
Behrmann DL, Bresnahan JC, Beattie MS, Shah BR . Spinal cord injury produced by consistent mechanical displacement of the cord in rats: behavioral and histologic analysis. J Neurotrauma 1992; 9: 197–217.
Grau JW, Washburn SN, Hook MA, Ferguson AR, Crown ED, Garcia G et al. Uncontrollable stimulation undermines recovery after spinal cord injury. J Neurotrauma 2004; 21: 1795–1817.
Arvidsson U, Riedl M, Chakrabarti S, Lee J-H, Nakano AH, Dado R et al. Distribution and targeting of a mu-opioid receptor (MOR1) in brain and spinal cord. J Neurosci 1995; 15: 3328–3341.
Mansour A, Fox CA, Burke S, Akil H, Watson SJ . Immunohistochemical localization of the cloned μ opioid receptor in the rat CNS. J Chem Neuroanat 1995; 8: 283–305.
Leighton G, Rodriguez R, Hill R, Hughes J . kappa-Opioid agonists produce antinociception after iv and icv but not intrathecal administration in the rat. Br J Pharmacol 1988; 93: 553.
Millan M . Kappa-opioid receptor-mediated antinociception in the rat. I. Comparative actions of mu-and kappa-opioids against noxious thermal, pressure and electrical stimuli. J Pharmacol Exp Ther 1989; 251: 334–341.
Schmauss C . Spinal κ-opioid receptor-mediated antinociception is stimulus-specific. Eur J Pharmacol 1987; 137: 197–205.
Schmauss C, Yaksh TL . In vivo studies on spinal opiate receptor systems mediating antinociception. II. Pharmacological profiles suggesting a differential association of mu, delta and kappa receptors with visceral chemical and cutaneous thermal stimuli in the rat. J Pharmacol Exp Ther 1984; 228: 1–12.
Herman BH, Goldstein A . Antinociception and paralysis induced by intrathecal dynorphin A. J Pharmacol Exp Ther 1985; 232: 27–32.
Piercey M, Lahti R, Schroeder L, Einspahr F, Barsuhn C . U-50488H, a pure kappa receptor agonist with spinal analgesic loci in the mouse. Life Sci 1982; 31: 1197–1200.
Lahti R, VonVoigtlander P, Barsuhn C . Properties of a selective kappa agonist, U-50,488 H. Life Sci 1982; 31: 2257–2260.
Yamada H, Shimoyama N, Sora I, Uhl GR, Fukuda Y, Moriya H et al. Morphine can produce analgesia via spinal kappa opioid receptors in the absence of mu opioid receptors. Brain Res 2006; 1083: 61–69.
Dietis N, Rowbotham D, Lambert D . Opioid receptor subtypes: fact or artifact? Br J Anaesth 2011; 107: 8–18.
Law P-Y, Reggio PH, Loh HH . Opioid receptors: toward separation of analgesic from undesirable effects. Trends Biochem Sci 2013; 38: 275–282.
Ho J, Mannes AJ, Dubner R, Caudle RM . Putative kappa-2 opioid agonists are antihyperalgesic in a rat model of inflammation. J Pharmacol Exp Ther 1997; 281: 136–141.
Nielsen CK, Ross FB, Lotfipour S, Saini KS, Edwards SR, Smith MT . Oxycodone and morphine have distinctly different pharmacological profiles: radioligand binding and behavioural studies in two rat models of neuropathic pain. Pain 2007; 132: 289–300.
Chang PC, Aicher SA, Drake CT . Kappa opioid receptors in rat spinal cord vary across the estrous cycle. Brain Res 2000; 861: 168–172.
Besse D, Lombard M, Zajac J, Roques B, Besson J . Pre-and postsynaptic distribution of μ, δ and κ opioid receptors in the superficial layers of the cervical dorsal horn of the rat spinal cord. Brain Res 1990; 521: 15–22.
Besse D, Weil-Fugazza J, Lombard M-C, Butler SH, Besson J-M . Monoarthritis induces complex changes in μ-, δ-and κ-opioid binding sites in the superficial dorsal horn of the rat spinal cord. Eur J Pharmacol 1992; 223: 123–131.
Maekawa K, Minami M, Masuda T, Satoh M . Expression of μ-and κ-, but not δ-, opioid receptor mRNAs is enhanced in the spinal dorsal horn of the arthritic rats. Pain 1996; 64: 365–371.
Faden AI, Molioneaux CJ, Rosenberger JG, Jacobs TP, Cox BM . Endogenous opioid immunoreactivity in rat spinal cord following traumatic injury. Ann Neurol 1985; 17: 386–390.
Krumins SA, Faden AI . Traumatic injury alters opiate receptor binding in rat spinal cord. Ann Neurol 1986; 19: 498–501.
Xu M, Bruchas MR, Ippolito DL, Gendron L, Chavkin C . Sciatic nerve ligation-induced proliferation of spinal cord astrocytes is mediated by κ opioid activation of p38 mitogen-activated protein kinase. J Neurosci 2007; 27: 2570–2581.
Raghavendra V, Rutkowski MD, DeLeo JA . The role of spinal neuroimmune activation in morphine tolerance/hyperalgesia in neuropathic and sham-operated rats. J Neurosci 2002; 22: 9980–9989.
Raghavendra V, Tanga FY, DeLeo JA . Attenuation of morphine tolerance, withdrawal-induced hyperalgesia, and associated spinal inflammatory immune responses by propentofylline in rats. Neuropsychopharmacology 2004; 29: 327–334.
Song P, Zhao Z-Q . The involvement of glial cells in the development of morphine tolerance. Neurosci Res 2001; 39: 281–286.
Cui Y, Chen Y, Zhi J-L, Guo R-X, Feng J-Q, Chen P-X . Activation of p38 mitogen-activated protein kinase in spinal microglia mediates morphine antinociceptive tolerance. Brain Res 2006; 1069: 235–243.
Ikeda H, Kiritoshi T, Murase K . Contribution of microglia and astrocytes to the central sensitization, inflammatory and neuropathic pain in the juvenile rat. Mol Pain 2012; 8: 43.
Faden AI . Opioid and nonopioid mechanisms may contribute to dynorphin's pathophysiological actions in spinal cord injury. Ann Neurol 1990; 27: 67–74.
Long JB, Petras J, Mobley WC, Holaday JW . Neurological dysfunction after intrathecal injection of dynorphin A (1-13) in the rat. II. Nonopioid mechanisms mediate loss of motor, sensory and autonomic function. J Pharmacol Exp Ther 1988; 246: 1167–1174.
Bakshi R, Ni R-X, Faden AI . N-methyl-D-aspartate (NMDA) and opioid receptors mediate dynorphin-induced spinal cord injury: behavioral and histological studies. Brain Res 1992; 580: 255–264.
Mao J, Price DD, Phillips LL, Lu J, Mayer DJ . Increases in protein kinase C gamma immunoreactivity in the spinal cord of rats associated with tolerance to the analgesic effects of morphine. Brain Res 1995; 677: 257–267.
Acknowledgements
We thank Eric Bancroft and Alejandro R Aceves for their comments on a previous version of this manuscript and the NIDA Drug Supply Program for their generous support. The NIDA Drug Supply Program generously provided the [+]- morphine enantiomer. This work was funded by grant DA31197 to MA Hook.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Aceves, M., Mathai, B. & Hook, M. Evaluation of the effects of specific opioid receptor agonists in a rodent model of spinal cord injury. Spinal Cord 54, 767–777 (2016). https://doi.org/10.1038/sc.2016.28
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2016.28
This article is cited by
-
Comparative Analysis of Infarct-Limiting Activity of Peptide and Non-Peptide δ- and κ-Opioid Receptor Agonists during Heart Reperfusion In Vivo
Bulletin of Experimental Biology and Medicine (2024)
-
Morphine-induced changes in the function of microglia and macrophages after acute spinal cord injury
BMC Neuroscience (2022)