Abstract
Study design:
Prospective vasopressor cross-over interventional study
Objectives:
To examine how two vasopressors used in acute traumatic spinal cord injury (SCI) affect intrathecal cerebrospinal fluid pressure and the corresponding spinal cord perfusion pressure (SCPP).
Setting:
Vancouver, British Columbia, Canada.
Methods:
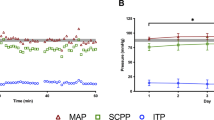
Acute SCI patients over the age of 17 with cervical or thoracic ASIA Impairment Scale (AIS). A, B or C injuries were enrolled in this study. Two vasopressors, norepinephrine and dopamine, were evaluated in a ‘crossover procedure’ to directly compare their effect on the intrathecal pressure (ITP). The vasopressor cross-over procedures were performed in the intensive care unit where ITP, mean arterial pressure (MAP) and heart rate were being continuously measured. The SCPP was calculated as the difference between MAP and ITP.
Results:
A total of 11 patients were enrolled and included in our analysis. There were 6 patients with AIS A, 3 with AIS B and 2 with AIS C injuries at baseline. We performed 24 cross-over interventions in these 11 patients. There was no difference in MAP with the use of norepinephrine versus dopamine (84±1 mm Hg for both; P=0.33). Conversely, ITP was significantly lower with the use of norepinephrine than with dopamine (17±1 mm Hg vs 20±1 mm Hg, respectively, P<0.001). This decrease in ITP with norepinephrine resulted in an increased SCPP during the norepinephrine infusion when compared with dopamine (67±1 mm Hg vs 65±1 mm Hg respectively, P=0.0049).
Conclusion:
Norepinephrine was able to maintain MAP with a lower ITP and a correspondingly higher SCPP as compared with dopamine in this study. These results suggest that norepinephrine may be preferable to dopamine if vasopressor support is required post SCI to maintain elevated MAPs in accordance with published guidelines.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tator CH, Fehlings MG . Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991; 75: 15–26.
Dumont RJ, Verma S, Okonkwo DO, Hurlbert RJ, Boulos PT, Ellegala DB et al. Acute spinal cord injury, part I: pathophysiologic mechanisms. Clin Neuropharmacol 2001; 24: 254–264.
Tator CH . Experimental and clinical studies of the pathophysiology and management of acute spinal cord injury. J Spinal Cord Med 1996; 19: 206–214.
Vale FL, Burns J, Jackson AB, Hadley MN . Combined medical and surgical treatment after acute spinal cord injury: results of a prospective pilot study to assess the merits of aggressive medical resuscitation and blood pressure management. J Neurosurg 1997; 87: 239–246.
Levi L, Wolf A, Belzberg H . Hemodynamic parameters in patients with acute cervical cord trauma: description, intervention, and prediction of outcome. Neurosurgery 1993; 33: 1007–1016.
Ryken CT, Hurlbert RJ, Hadley MN, Aarabi B, Dhall SS, Gelb DE et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery 2013; 72: 84–92.
Casha S, Christie S . A systematic review of intensive cardiopulmonary management after spinal cord injury. J Neurotrauma 2011; 28: 1479–1495.
Consortium for Spinal Cord Medicine. Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2008; 31: 403–479.
Hawryluk G, Whetstone W, Saigal R, Ferguson A, Talbott J, Bresnahan J et al. Mean arterial blood pressure correlates with neurological recovery after human spinal cord injury: analysis of high frequency physiologic data. J Neurotrauma 2015; 32: 1958–1967.
Kwon BK, Curt A, Belanger LM, Bernardo A, Chan D, Markez JA et al. Intrathecal pressure monitoring and cerebrospinal fluid draining in acute spinal cord injury: a prospective randomized trial. J Neurosurg Spine 2009; 10: 181–193.
Werndle MC, Saadoun S, Phang I, Czosnyka M, Varsos GV, Czosnyka ZH et al. Monitoring of spinal cord perfusion pressure in acute spinal cord injury: initial findings of the injured spinal cord pressure evaluation study. Crit Care Med 2014; 42: 646–655.
Phang I, Papadopoulos MC . Intraspinal pressure monitoring in a patient with spinal cord injury reveals different intradural compartments: Injured Spinal Cord Pressure Evaluation (ISCoPE) Study. Neurocritical Care 2015; 23: 414–418.
Ract C, Vigué B . Comparison of the cerebral effects of dopamine and norepinephrine in severely head-injured patients. Intensive Care Med 2001; 27: 101–106.
Steiner LA, Johnston AJ, Czosnyka M, Chatfield DA, Salvador R, Coles JP et al. Direct comparison of cerebrovascular effects of norepinephrine and dopamine in head-injured patients. Crit Care Med 2004; 32: 1049–1054.
Sookplung P, Siriussawakul A, Malakouti A, Sharma D, Wang J, Souter MJ et al. Vasopressor use and effect on blood pressure after severe adult traumatic brain injury. Neurocrit Care 2011; 15: 46–54.
Inoue T, Manley GT, Patel N, Whetstone WD . Medical and surgical management after spinal cord injury: vasopressor usage, early surgerys, and complications. J Neurotrauma 2014; 31: 284–291.
Readdy WJ, Whetstone WD, Ferguson AR, Talbott JF, Inoue T, Saigal R et al. Complications and outcomes of vasopressor usage in acute traumatic central cord syndrome. J Neurosurg Spine, (e-pub ahead of print 31 July 2015).
Kwon BK, Stammers AM, Belanger LM, Bernardo A, Chan D, Bishop CM et al. Cerebrospinal fluid inflammatory cytokines and biomarkers of injury severity in acute human spinal cord injury. J Neurotrauma 2010; 27: 669–682.
Hadley M, Walters B, Grabb P, Oyesiku NM, Przybylski GJ, Resnick DK et al. Guidelines for the management of acute cervical spine and spinal cord injuries. Clin Neurosurg 2002; 49: 407–498.
Di Gennaro JL, Mack CD, Malakouti A, Zimmerman JJ, Armstead W, Vavilala MS . Use and effect of vasopressors after pediatric traumatic brain injury. Dev Neurosci 2010; 32: 420–430.
Muzevich KM, Voils SA . Role of vasopressor administration in patients with acute neurologic injury. Neurocrit Care 2009; 11: 112–119.
Pfister D, Strebel SP, Steiner LA . Effects of catecholamines on cerebral blood vessels in patients with traumatic brain injury. Eur J Anaesthesiol Suppl 2008; 42: 98–103.
Kroppenstedt SN, Sakowitz OW, Thomale UW, Unterberg AW, Stover JF . Influence of norepinephrine and dopamine on cortical perfusion, EEG activity, extracellular glutamate, and brain edema in rats after controlled cortical impact injury. J Neurotrauma 2002; 19: 1421–1432.
Kroppenstedt SN, Sakowitz OW, Thomale UW, Unterberg AW, Stover JF . Norepinephrine is superior to dopamine in increasing cortical perfusion following controlled cortical impact injury in rats. Acta Neurochir Suppl 2002; 81: 225–227.
Beaumont A, Hayasaki K, Marmarou A, Barzo P, Fatouros P, Corwin F . The effects of dopamine on edema formation in two models of traumatic brain injury. Acta Neurochir Suppl 2000; 76: 147–151.
Johnston AJ, Steiner LA, Chatfield DA, Coles JP, Hutchinson PJ, Al-Rawi PG et al. Effect of cerebral perfusion pressure augmentation with dopamine and norepinephrine on global and focal brain oxygenation after traumatic brain injury. Intensive Care Med 2004; 30: 791–797.
Clifton GL, Choi SC, Miller ER, Levin HS, Smith KR Jr, Muizelaar JP et al. Intercenter variance in clinical trials of head trauma-experience of the National Acute Brain Injury Study: hypothermia. J Neurosurg 2001; 95: 751–755.
Kong CY, Hosseini AM, Belanger LM, Ronco JJ, Paquette SJ, Boyd MC et al. A prospective evaluation of hemodynamic management in acute spinal cord injury patients. Spinal Cord 2013; 51: 466–471.
Varsos GV, Werndle MC, Czosnyka ZH, Smielewski P, Kolias AG, Phang I et al. Intraspinal pressure and spinal cord perfusion pressure after spinal cord injury: an observational study. J Neurosurg Spine 2015; 14: 1–9.
Eriksen VR, Hahn GH, Greisen G . Dopamine therapy is associated with impaired cerebral autoregulation in preterm infants. Acta Paediatr 2014; 103: 1221–1226.
Armstead WM, Riley J, Vavilala MS . Dopamine prevents impairment of autoregulation after traumatic brain injury in the newborn pig through inhibition of up-regulation of endothelin-1 and extracellular signal-regulated kinase mitogen-activated protein kinase. Pediatr Crit Care Med 2013; 14: e103–e111.
Acknowledgements
We acknowledge the research staff of the Vancouver Spine Research Program, in particular Allan Aludino, Leilani Reichl, Angela Tsang and Jiwan Gill for their assistance with this study. We also acknowledge support for the conduct of this study from the Michael Smith Foundation for Health Research, the Craig H. Neilsen Foundation and the Rick Hansen Institute (RHI), including Daniel Rogers of RHI for project management. Dr Griesdale is supported by the VGH & UBC Hospital Foundation Best of Health Fund. MFD holds the Paetzold Chair in Spinal Cord Injury Research. FKK holds the Canada Research Chair in Spinal Cord Injury and VGH & UBC Hospital Foundation Dvorak Chair in Spine Trauma.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Altaf, F., Griesdale, D., Belanger, L. et al. The differential effects of norepinephrine and dopamine on cerebrospinal fluid pressure and spinal cord perfusion pressure after acute human spinal cord injury. Spinal Cord 55, 33–38 (2017). https://doi.org/10.1038/sc.2016.79
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2016.79
This article is cited by
-
Perioperative management in acute and chronic spinal cord injury, narrative review
Journal of Anesthesia, Analgesia and Critical Care (2025)
-
Invasive devices to monitor the intraspinal perfusion pressure in the hemodynamic management of acute spinal cord injury: A systematic scoping review
Acta Neurochirurgica (2024)
-
Critical Care of Spinal Cord Injury
Current Neurology and Neuroscience Reports (2024)
-
Pharmacologic and Acute Management of Spinal Cord Injury in Adults and Children
Current Treatment Options in Neurology (2022)
-
Neurorestorative interventions involving bioelectronic implants after spinal cord injury
Bioelectronic Medicine (2019)