Abstract
Study design:
Prospective cohort study.
Objectives:
Dysphagia is a relatively common secondary complication in patients with traumatic cervical spinal cord injuries (TCSCI). The purpose of this study was to determine the incidence of aspiration and penetration in patients with acute TCSCI.
Setting:
Tampere University Hospital, Tampere, Finland.
Methods:
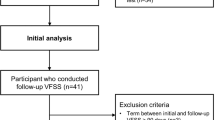
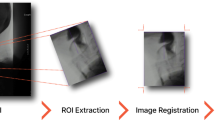
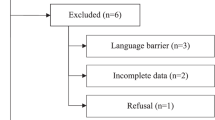
A total of 46 patients with TCSCI were evaluated with a videofluoroscopic swallowing study (VFSS). Rosenbek’s penetration-aspiration scale (PAS) was used to classify the degree of penetration or aspiration. The medical records of each patient were systematically reviewed.
Results:
Of the 46 patients, 85% were male. The mean age at the time of the injury was 62.1 years. Most patients had an incomplete injury (78%), and most of them due to a fall (78%). In the VFSS 19 (41%) patients penetrated and 15 (33%) aspirated. Only 12 (26%) of the patients had a PAS score of 1 indicating that swallowed material did not enter the airway. Of the patients who aspirated, 73% had silent aspiration.
Conclusion:
The incidence of penetration or aspiration according to VFSS is high in this cohort of patients with TCSCI. Therefore, the swallowing function of patients with acute TCSCI should be routinely evaluated before initiating oral feeding. VFSS is highly recommended, particularly to rule out the possibility of silent aspiration and to achieve information on safe nutrition consistency.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kirshblum S, Johnston MV, Brown J, O'Connor KC, Jarosz P . Predictors of dysphagia after spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1101–1105.
Wolf C, Meiners TH . Dysphagia in patients with acute cervical spinal cord injury. Spinal Cord 2003; 41: 347–353.
Brady S, Miserendino R, Statkus R, Springer T, Hakel M, Stambolis V . Predictors to dysphagia and recovery after cervical spinal cord injury during acute rehabilitation. J Appl Res 2004; 4: 1–11.
Abel R, Ruf S, Spahn B . Cervical spinal cord injury and deglutition disorders. Dysphagia 2004; 19: 87–94.
Shem K, Castillo K, Naran B . Factors associated with dysphagia in individuals with high tetraplegia. Top Spinal Cord Injury Rehabil 2005; 10: 8–18.
Seidl RO, Nusser-Muller-Busch R, Kurzweil M, Niedeggen A . Dysphagia in acute tetraplegics: a retrospective study. Spinal Cord 2010; 48: 197–201.
Shin JC, Yoo JH, Lee YS, Goo HR, Kim DH . Dysphagia in cervical spinal cord injury. Spinal Cord 2011; 49: 1008–1013.
Shem K, Castillo K, Wong S, Chang J . Dysphagia in individuals with tetraplegia: incidence and risk factors. J Spinal Cord Med 2011; 34: 85–92.
Shem K, Castillo K, Wong SL, Chang J, Kolakowsky-Hayner S . Dysphagia and Respiratory Care in Individuals with Tetraplegia: Incidence, Associated Factors, and Preventable Complications. Top Spinal Cord Inj Rehabil 2012; 18: 15–22.
Chaw E, Shem K, Castillo K, Wong SL, Chang J . Dysphagia and associated respiratory considerations in cervical spinal cord injury. Top Spinal Cord Inj Rehabil 2012; 18: 291–299.
Shem KL, Castillo K, Wong SL, Chang J, Kao MC, Kolakowsky-Hayner SA . Diagnostic accuracy of bedside swallow evaluation versus videofluoroscopy to assess dysphagia in individuals with tetraplegia. Pm R 2012; 4: 283–289.
Smithard DG, O'Neil PA, Park C, Morris J, Wyatt R, England R et al. Complications and outcome after acute stroke: does dysphagia matter?[Article]. Stroke 1996; 27: 1200–1204.
Carrión S, Cabré M, Monteis R, Roca M, Palomera E, Serra-Prat M et al. Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin Nutr 2015; 34: 436–442.
Garcia-Peris P, Paron L, Velasco C, de la Cuerda C, Camblor M, Breton I et al. Long-term prevalence of oropharyngeal dysphagia in head and neck cancer patients: Impact on quality of life. Clin Nutr 2007; 26: 710–717.
Leibovitz A, Baumoehl Y, Lubart E, Yaina A, Platinovitz N, Segal R . Dehydration among long-term care elderly patients with oropharyngeal dysphagia. Gerontology 2007; 53: 179–183.
Winslow C, Bode RK, Felton D, Chen D, Meyer PR Jr . Impact of respiratory complications on length of stay and hospital costs in acute cervical spine injury. Chest 2002; 121: 1548–1554.
Logemann JA . Introduction: Definitions and basic principles of evaluation and treatment of swallowing disorders. Evaluation and treatment of swallowing disorders 2nd ed. Austin, TX, USA: Pro-Ed. 1998 p 1–5.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL . A penetration-aspiration scale. Dysphagia 1996; 11: 93–98.
Koskinen EA, Alen M, Vaarala EM, Rellman J, Kallinen M, Vainionpaa A . Centralized spinal cord injury care in Finland: unveiling the hidden incidence of traumatic injuries. Spinal Cord 2014; 52: 779–784.
DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T et al. International Spinal Cord Injury Core Data Set. Spinal Cord 2006; 44: 535–540.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med 2011; 34: 547–554.
Robbins J, Coyle J, Rosenbek J, Roecker E, Wood J . Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia 1999; 14: 228–232.
Daggett A, Logemann J, Rademaker A, Pauloski B . Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia 2006; 21: 270–274.
Allen JE, White CJCCC, Leonard RJ, Belafsky PC . Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Otolaryngol Head Neck Surg 2010; 142: 208–213.
Smith CH, Logemann JA, Colangelo LA, Rademaker AW, Pauloski BR . Incidence and patient characteristics associated with silent aspiration in the acute care setting. Dysphagia 1999; 14: 1–7.
Garon BR, Sierzant T, Ormiston C . Silent aspiration: results of 2,000 video fluoroscopic evaluations. J Neurosci Nurs 2009 quiz 186-7; Aug 41: 178–185.
Acknowledgements
We thank the patients, biostatistician Mika Helminen, research assistant Anne Simi, and the physiotherapists at the ICU unit, the neurosurgical ward, and the neurological rehabilitation ward of Tampere University Hospital for their assistance. This work was supported by funds from the Maire Taponen Foundation (TI).
Author contributions
TI contributed to the study design, data collection, data analysis, data interpretation, and article preparation. IR-K contributed to the data collection and article preparation. TML contributed to the data interpretation and article preparation. EK contributed to the data collection and article preparation. A-MK-H contributed to the article preparation. AR contributed to the study design and article preparation
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ihalainen, T., Rinta-Kiikka, I., Luoto, T. et al. Traumatic cervical spinal cord injury: a prospective clinical study of laryngeal penetration and aspiration. Spinal Cord 55, 979–984 (2017). https://doi.org/10.1038/sc.2017.71
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2017.71
This article is cited by
-
Mortality and causes of death of traumatic spinal cord injury in Finland
Spinal Cord (2025)
-
Identification of immune-related hub genes in spinal cord injury
European Journal of Medical Research (2024)
-
Oropharyngeal Dysphagia in Acute Cervical Spinal Cord Injury: A Literature Review
Dysphagia (2023)
-
Videofluoroscopic Profiles of Swallowing and Airway Protection Post-traumatic Cervical Spinal Cord Injury
Dysphagia (2022)
-
The time course of dysphagia following traumatic cervical spinal cord injury: a prospective cohort study
Spinal Cord (2020)