Abstract
Study design:
Retrospective chart audit.
Objectives:
This study aims to compare the clinical features and surgical outcomes in patients with cervical spondylotic myelopathy (CSM) among different age groups.
Setting:
The first Affiliated Hospital of Anhui Medical University, China.
Methods:
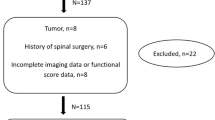
A total of 460 patients with CSM who were surgically treated over the period of 1995–2009 were investigated. Considering the peak age (40–60 years old) for the onset of symptoms, we divided the patients into three groups by age: young (<40), middle-aged (40–60), and old (>60). The differences in symptoms, symptom durations, involved levels, surgical approaches and outcomes were evaluated.
Results:
The number of symptoms and involved levels, symptom duration and posterior approach significantly increased with increasing age, whereas preoperative Japanese Orthopedic Association score decreased among the three groups. Spinal cord function improved after surgery in all groups. The highest degree of recovery occurred during the first 6 months after surgery, especially within the first week, and then reached a plateau. After 6 months, however, recovery continuously improved, stabilized and declined in the young, middle-aged, old groups, respectively. The recovery rate was not significantly different at an immediate period (1 week) after operation among the three groups, but was significantly different at later periods (3 or more months postoperatively). Three groups showed no difference in postoperative complication rates.
Conclusion:
The severity of CSM increased with increasing age. Age was inversely correlated with recovery, and recovery decreased as age increased. Six months post operation was the prime time for the recovery of spinal cord function.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kalsi-Ryan S, Karadimas SK, Fehlings MG . Cervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist 2013; 19: 409–421.
Karadimas SK, Erwin WM, Ely CG, Dettori JR, Fehlings MG . Pathophysiology and natural history of cervical spondylotic myelopathy. Spine 2013; 38 (22 Suppl 1): S21–S36.
Tracy JA, Bartleson JD . Cervical spondylotic myelopathy. Neurologist 2010; 16: 176–187.
Rhee JM, Shamji MF, Erwin WM, Bransford RJ, Yoon ST, Smith JS et al. Nonoperative management of cervical myelopathy: a systematic review. Spine 2013; 38 (22 Suppl 1): S55–S67.
Machino M, Yukawa Y, Hida T, Ito K, Nakashima H, Kanbara S et al. The prevalence of pre- and postoperative symptoms in patients with cervical spondylotic myelopathy treated by cervical laminoplasty. Spine 2012; 7: E1383–E1388.
Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Ito Z et al. Laminoplasty and skip laminectomy for cervical compressive myelopathy: range of motion, postoperative neck pain, and surgical outcomes in a randomized prospective study. Spine 2007; 32: 1980–1985.
Boogaarts HD, Bartels RH . Prevalence of cervical spondylotic myelopathy. Eur Spine J 2015; 24 (Suppl 2): 139–141.
Yamauchi H, Hirabayashi K . Scoring system (17–2) for cervical myelopathy (Japanese Orthopaedic Association). J Jpn Orthop Assoc 1994; 68: 490–503.
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K . Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 1981; 6: 354–364.
Northover JR, Wild JB, Braybrooke J, Blanco J . The epidemiology of cervical spondylotic myelopathy. Skeletal Radiol 2012; 41: 1543–1546.
Miller JA, Schmatz C, Schultz AB . Lumbar disc degeneration: correlation with age, sex, and spine level in 600 autopsy specimens. Spine 1998; 13: 173–178.
Lawrence JS . Disc degeneration: its frequency and relationship to symptoms. Ann Rheum Dis 1969; 28: 121–137.
Lee MJ, Cassinelli EH, Riew KD . Prevalence of cervical spine stenosis anatomic study in cadavers. J Bone Joint Surg Am 2007; 89: 376–380.
Brain R . Cervical spondylosis. Ann Intern Med 1954; 41: 439–446.
Doppman JL . The mechanism of ischemia in anteroposterior compression of the spinal cord1975. Invest Radiol 1990; 25: 444–452.
Chen J, Liu Z, Zhong G, Qian L, Li Z, Chen B et al. Surgical treatment for cervical spondylotic myelopathy in elderly patients: a retrospective study. Clin Neurol Neurosurg 2015; 132: 47–51.
Nagashima H, Dokai T, Hashiguchi H, Ishii H, Kameyama Y, Katae Y et al. Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: a multi-center retrospective study. Eur Spine J 2011; 20: 240–246.
Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T . Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery 2003; 52: 122–126.
Hasegawa K, Homma T, Chiba Y, Hirano T, Watanabe K, Yamazaki A . Effects of surgical treatment for cervical spondylotic myelopathy in patients C70 years of age: a retrospective comparative study. J Spinal Disord Tech 2002; 15: 458–460.
Matsuda Y, Shibata T, Oki S, Kawatani Y, Mashima N, Oishi H . Outcomes of surgical treatment for cervical myelopathy in patients more than 75 years of age. Spine 1999; 24: 529–534.
Acharya S, Srivastava A, Virmani S, Tandon R . Resolution of physical signs and recovery in severe cervical spondylotic myelopathy after cervical laminoplasty. Spine 2010; 35: E1083–E1087.
Tetreault LA, Côté P, Kopjar B, Arnold P, Fehlings MG, AOSpine North America and International Clinical Trial Research Network. A clinical prediction model to assess surgical outcome in patients with cervical spondylotic myelopathy: internal and external validations using the prospective multicenter AOSpine North American and international datasets of 743 patients. Spine J 2015; 15: 388–397.
Alafifi T, Kern R, Fehling M . Clinical and MRI predictors of outcome after surgical intervention for cervical spondylotic myelopathy. J Neuroimag 2007; 17: 315–322.
Uchida K, Nakajima H, Takeura N, Yayama T, Guerrero AR, Yoshida A et al. Prognostic value of changes in spinal cord signal intensity on magnetic resonance imaging in patients with cervical compressive myelopathy. Spine J 2014; 14: 1601–1610.
Ma L, Zhang D, Chen W, Shen Y, Zhang Y, Ding W et al. Correlation between magnetic resonance T2 image signal intensity ratio and cell apoptosis in a rabbit spinal cord cervical myelopathy model. Chin Med J 2014; 127: 305–313.
Zhou F, Zhang Y, Sun Y, Zhang F, Pan S, Diao Y et al. Profiles of and correlation between objective and subjective outcome assessments following open-door laminoplasty for cervical spondylotic myelopathy. Chin Med J 2014; 127: 2659–2663.
Tetreault LA, Nouri A, Singh A, Fawcett M, Fehlings MG . Predictors of outcome in patients with cervical spondylotic myelopathy undergoing surgical treatment: a survey of members from AOSpine International. World Neurosurg 2014; 81: 623–633.
Machino M, Yukawa Y, Imagama S, Ito K, Katayama Y, Matsumoto T et al. Surgical treatment assessment of cervical laminoplasty using quantitative performance evaluation in elderly patients. Spine 2016; 41: 757–763.
Nagano A, Miyamoto K, Hosoe H, Iinuma N, Nishimoto H, Sakaeda H et al. Surgical treatment for cervical myelopathy in patients aged >80 years. Orthopedics 2004; 27: 45–48.
Hasegawa K, Homma T, Chiba Y, Hirano T, Watanabe K, Yamazaki A . Effects of surgical treatment for cervical spondylotic myelopathy in patients⩾70 years of age: a retrospective comparative study. J Spinal Disord Tech 2002; 15: 458–460.
Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Abe Y, Kimura T . Pathomechanism of myelopathy and surgical results of laminoplasty in elderly patients with cervical spondylosis. Spine 2003; 28: 2209–2214.
Acknowledgements
This study is supported by the Natural Science Foundation Project of China, 2014 (No. 81472088).
Author contributions
RJZ participated in the study design and data analysis, and drafted the manuscript. FLD, PWS, PG, PX and HQZ reviewed the medical records of the patients, as well as the office notes and operative reports to collect the pre-, peri- and postoperative data. XJZ participated in data analysis. CLS and JXZ participated in the study design and performed the surgery. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, R., Shen, C., Zhang, J. et al. Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients of different ages: a retrospective study. Spinal Cord 56, 7–13 (2018). https://doi.org/10.1038/sc.2017.91
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sc.2017.91
This article is cited by
-
“White Cord Syndrome” as clinical manifestation of the spinal cord reperfusion syndrome: a systematic review of risk factors, treatments, and outcome
European Spine Journal (2025)
-
Tract-specific magnetization transfer ratio provides insights into the severity of degenerative cervical myelopathy
Spinal Cord (2024)