Abstract
Study design:
A cross-sectional study.
Objectives:
To describe the use of medicines and adherence among persons with spinal cord injury (SCI). Further, to examine the influence of pain, spasms and beliefs about medicines on adherence.
Setting:
Sunnaas Rehabilitation Hospital, Norway.
Methods:
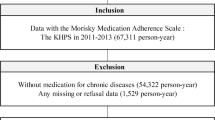
Persons (⩾18 years) with chronic SCI (more than 1-year post injury), using at least one drug regularly, and admitted for a follow-up stay at Sunnaas Rehabilitation Hospital were included. Participants were interviewed about their drug regimen and filled out validated self-report questionnaires: Morisky Medication Adherence Scale (MMAS-8), beliefs about medicines questionnaire (BMQ), visual analogue scale (VAS) for pain and modified Penn spasm frequency scale (mPSFS).
Results:
The 105 participants used in average 4.2 drugs regularly (range, 1–15), and 70% reported high or moderate adherence to their treatment. Of the 39 participants using oral spasmolytics, 74% reported high or moderate adherence to these drugs. A total of 97% of the participants reported high perceptions of necessity to their treatment and 54% reported a high level of concern.
Conclusion:
The persons with SCI included in this study used in average the same number of regular drugs compared to persons with other chronic conditions. Regardless of high overall adherence, the participants were more concerned about their medicines compared to other patient groups. Further studies are required for understanding adherence and attitudes toward medicines in this population, especially to help the persons with chronic SCI feel safe about their drug regimen.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Garstang SV, Miller-Smith SA . Autonomic nervous system dysfunction after spinal cord injury. Phys Med Rehab Clin North Am 2007; 18: 275–296.
Hsieh JT, Wolfe DL, Miller WC, Curt A . Spasticity outcome measures in spinal cord injury: psychometric properties and clinical utility. Spinal Cord 2008; 46: 86–95.
Hagen EM, Rekand T . Management of neuropathic pain associated with spinal cord injury. Pain Ther 2015; 4: 51–65.
World Health Organization. Adherence to long-term therapies-Evidence for action. Geneva, Switzerland, 2003. Available at http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf (accessed 23 June 2017).
Nguyen TM, La Caze A, Cottrell N . What are validated self-report adherence scales really measuring?: a systematic review. Br J Clin Pharmacol 2014; 77: 427–445.
Adams MM, Hicks AL . Spasticity after spinal cord injury. Spinal Cord 2005; 43: 577–586.
Halpern R, Gillard P, Graham GD, Varon SF, Zorowitz RD . Adherence associated with oral medications in the treatment of spasticity. J Injury Funct Rehab 2013; 5: 747–756.
Sunnaas sykehus HF, Haukeland Universitetssykehus HF, St. Olavs Hospital HF. ABC om ryggmargsskade for helsepersonell. Landsforeningen for Ryggmargsskadde. Oslo, 2012. Available at http://lars.no/vare-publikasjoner (accessed 23 June 2017).
Scullin C, Scott MG, Hogg A, McElnay JC . An innovative approach to integrated medicines management. J Eval Clin Pract 2007; 13: 781–788.
WHO Collaborating Centre for Drug Statistic Methodology Anatomical Therapeutic Chemical Code. WHO: Oslo, Norway. 2013. Available at http://www.whocc.no (accesses 23 June 2017).
Morisky DE, DiMatteo MR . Improving the measurement of self-reported medication nonadherence: final response. J Clin Epidemiol 2011; 64: 262–263.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ . Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens 2008; 10: 348–354.
Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P . New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care 2009; 15: 59–66.
Horne R, Weinman J, Hankins M . The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health 1999; 14: 1–24.
McCormack HM, de L Horne DJ, Sheather S . Clinical applications of visual analogue scales: a critical review. Psychol Med 2009; 18: 1007–1019.
Collins SL, Moore RA, McQuay HJ . The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain 1997; 72: 95–97.
Penn RD . Intrathecal Baclofen for severe spasticity. Ann N Y Acad Sci 1988; 531: 157–166.
Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V et al. International spinal cord injury core data set (version 2.0)-including standardization of reporting. Spinal Cord 2017; 55: 759–764.
Napolitano F, Napolitano P, Angelillo IF . Medication adherence among patients with chronic conditions in Italy. Eur J Public Health 2016; 26: 48–52.
Akincigil A, Bowblis JR, Levin C, Walkup JT, Jan S, Crystal S . Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care 2007; 45: 363–369.
Nilsson N, Lea M, Lao Y, Wendelbo K, Gløersen G, Mowé M et al. Medication discrepancies revealed by medication reconciliation and their potential short-term and long-term effects: a Norwegian multicentre study carried out on internal medicine wards. Eur J Hosp Pharm 2015; 22: 298–303.
Stevenson VL . Rehabilitation in practice: spasticity management. Clin Rehab 2010; 24: 293–304.
Rekand T, Hagen EM, Gronning M . Spasticity following spinal cord injury. Tidsskrift for den Norske laegeforening 2012; 132: 970–973.
Finnerup NB, Baastrup C, Jensen TS . Neuropathic pain following spinal cord injury pain: mechanisms and treatment. Scand J Pain 2009; 1: S3–S11.
Baastrup C, Finnerup NB . Pharmacological management of neuropathic pain following spinal cord injury. CNS Drugs 2008; 22: 455–475.
Saadat Z, Nikdoust F, Aerab-Sheibani H, Bahremand M, Shobeiri E, Saadat H et al. Adherence to antihypertensives in patients with comorbid condition. Nephro Urol Month 2015; 7: e29863.
Castellucci LA, Shaw J, van der Salm K, Erkens P, Le Gal G, Petrcich W et al. Self-reported adherence to anticoagulation and its determinants using the Morisky medication adherence scale. Thromb Res 2015; 136: 727–731.
Morisky DE, Malotte CK, Choi P, Davidson P, Rigler S, Sugland B et al. A patient education program to improve adherence rates with antituberculosis drug regimens. Health Educ Q 1990; 17: 253–267.
Osterberg L, Blaschke T . Adherence to medication. N Engl J Med 2005; 353: 487–497.
Krueger K, Botermann L, Schorr SG, Griese-Mammen N, Laufs U, Schulz M . Age-related medication adherence in patients with chronic heart failure: a systematic literature review. Int J Cardiol 2015; 184: 728–735.
Horne R, Weinman J . Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res 1999; 47: 555–567.
Maguire LK, Hughes CM, McElnay JC . Exploring the impact of depressive symptoms and medication beliefs on medication adherence in hypertension-a primary care study. Patient Educ Counsel 2008; 73: 371–376.
Viktil KK, Froyland H, Rogvin M, Moger TA . Beliefs about medicines among Norwegian outpatients with chronic cardiovascular disease. Eur J Hosp Pharm 2014; 21: 118–120.
Neame R, Hammond A . Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatology 2005; 44: 762–767.
Stirratt MJ, Dunbar-Jacob J, Crane HM, Simoni JM, Czajkowski S, Hilliard ME et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med 2015; 5: 470–482.
Acknowledgements
The study was funded by the Hospital Pharmacies Enterprise, South Eastern Norway and Sunnaas Rehabilitation Hospital. We thank the study participants and the nursing staff of department for follow-up at Sunnaas Rehabilitation Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Høgholen, H., Storhaug, A., Kvernrød, K. et al. Use of medicines, adherence and attitudes to medicines among persons with chronic spinal cord injury. Spinal Cord 56, 35–40 (2018). https://doi.org/10.1038/sc.2017.95
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/sc.2017.95