Abstract
Introduction:
The impact of muscle spasticity on weight change and energy expenditure after spinal cord injury (SCI) is not well understood.
Case presentation:
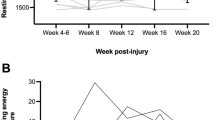
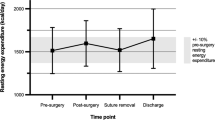
This case study reports changes to body weight and resting energy expenditure (REE) in a 36-year-old female (T3 AIS A SCI; 80 kg; body mass index=28 kg m−2 at injury) requiring escalating therapies to manage severe spasticity. Body weight, spasticity medications and fasted REE (measured using indirect calorimetry, canopy hood) were recorded at 4, 16, 17, 20 and 44 months post injury. Spasticity was assessed at each time point using the Modified Ashworth Scale (MAS). At 4 months post injury, REE was high (1710 kcal per day) corresponding with severe spasticity in the lower limbs (4 on the MAS). Over the following 12 months, the patient experienced an 8 kg weight loss, visible lower limb muscle wasting and a 30% reduction in REE while requiring increasing drug therapies for spasticity. With insertion of an intrathecal Baclofen pump at 17 months and cessation of other medications, spasticity improved markedly and weight increased by 6 kg in 27 months without any significant change to REE (mean=1260 kcal±2%).
Discussion:
Effective management of spasticity with intrathecal Baclofen appears to be associated with weight gain but not REE. Without body composition and activity energy expenditure data, this observation is difficult to explain. Regardless, routine weight monitoring with appropriate dietary counselling should be considered in this patient group to help prevent unintentional weight gain.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lance JW . The control of muscle tone, reflexes, and movement: Robert Wartenberg Lecture. Neurology 1980; 30: 1303–1313.
Maynard FM, Karunas RS, Waring WP III . Epidemiology of spasticity following traumatic spinal cord injury. Arch Phys Med Rehabil 1990; 71: 566–569.
Andresen SR, Biering-Sorensen F, Hagen EM, Nielsen JF, Bach FW, Finnerup NB . Pain, spasticity and quality of life in individuals with traumatic spinal cord injury in Denmark. Spinal Cord 2016; 54: 973–979.
Westerkam D, Saunders LL, Krause JS . Association of spasticity and life satisfaction after spinal cord injury. Spinal Cord 2011; 49: 990–994.
Skold C, Levi R, Seiger A . Spasticity after traumatic spinal cord injury: nature, severity, and location. Arch Phys Med Rehabil 1999; 80: 1548–1557.
Krause JS, Vines CL, Farley TL, Sniezek J, Coker J . An exploratory study of pressure ulcers after spinal cord injury: relationship to protective behaviors and risk factors. Arch Phys Med Rehabil 2001; 82: 107–113.
Adams MM, Hicks AL . Spasticity after spinal cord injury. Spinal Cord 2005; 43: 577–586.
Gorgey AS, Dudley GA . Spasticity may defend skeletal muscle size and composition after incomplete spinal cord injury. Spinal Cord 2008; 46: 96–102.
Buchholz AC, McGillivray CF, Pencharz PB . Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr 2003; 77: 371–378.
Yilmaz B, Yasar E, Goktepe S, Alaca R, Yazicioglu K, Dal U et al. Basal metabolic rate and autonomic nervous system dysfunction in men with spinal cord injury. Obesity (Silver Spring, MD) 2007; 15: 2683–2687.
Gorgey AS, Chiodo AE, Zemper ED, Hornyak JE, Rodriguez GM, Gater DR . Relationship of spasticity to soft tissue body composition and the metabolic profile in persons with chronic motor complete spinal cord injury. J Spinal Cord Med 2010; 33: 6–15.
Garrow JS, Ralph WPT . Human Nutrition and Dietetics, 9th edn. Churchill Livingstone Medical Division: New York, NY, USA, 1993.
Nevin AN, Steenson J, Vivanti A, Hickman IJ . Investigation of measured and predicted resting energy needs in adults after spinal cord injury: a systematic review. Spinal Cord 2016; 54: 248–253.
Nevin A, Mayr H, Atresh S, Kemp I, Simmons J, Vivanti A et al. Feasibility and acceptability of implementing indirect calorimetry into routine clinical care of patients with spinal cord injury. Top Spinal Cord Inj Rehabil 2016; 22: 269–276.
Bohannon RW, Smith MB . Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 1987; 67: 206–207.
Compher C, Frankenfield D, Keim N, Roth-Yousey L . Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc 2006; 106: 881–903.
Taittonen M, Raty H, Kirvela O, Aantaa R, Kanto J . The metabolic effects of oral tizanidine in healthy volunteers. Acta Anaesthesiol Scand 1995; 39: 628–632.
Elia M . Energy expenditure in the whole body. In: Kinney J, Tucker H (eds). Energy Metabolism: Tissue Determinants and Cellular Corollaries. Raven Press: New York NY, USA, 1992, pp 19–60.
Festa A, D'Agostino R Jr, Williams K, Karter AJ, Mayer-Davis EJ, Tracy RP et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord 2001; 25: 1407–1415.
Acknowledgements
This work was granted an exemption from requiring formal ethical review by the Metro South Human Research Ethics committee. Patient consent was obtained for this information to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nevin, A., Nguyen, K., Atresh, S. et al. Effective management of spasticity and impacts on weight change and resting energy expenditure in a female with spinal cord injury: a case report. Spinal Cord Ser Cases 3, 17057 (2017). https://doi.org/10.1038/scsandc.2017.57
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2017.57